Trauma Imaging in Pregnancy: A Review of the Evolving Appearance of the Placenta on CT and Mimics of Placental Injury
Images





CME credits are available for this article here.
Blunt abdominopelvic trauma in pregnant patients can be a cause of great concern for both the mother and the fetus. The fetus should always undergo sonographic evaluation and monitoring to assess for signs of distress or demise.
Cross-sectional imaging should be used judiciously, as radiation emitted by computed tomography (CT) increases the risk of harm to the fetus and development of childhood cancers. Given the rarity with which CT is performed on pregnant patients, this manuscript will review the indications and risks of CT in pregnant trauma patients, the normal CT appearance and evolution of the placenta, physiologic findings of pregnancy on CT that may mimic placental injury, and commonly encountered pregnancy-related traumatic injuries.
Abdominopelvic trauma in pregnancy poses a clinical conundrum with respect to imaging in the emergency room. In pregnant trauma patients, various imaging modalities may be utilized to evaluate the mother and fetus. Radiography is the first line of imaging, used as a primary survey of the cervical spine, chest, and pelvis.1-3 The benefit of radiography is its ability to rapidly assess possible fractures and common thoracic trauma with relatively low radiation dose.
Ultrasound is used both to assess the fetus and to detect intra-abdominal and pericardial fluid in the mother, the latter as part of a focused assessment with sonography in trauma (FAST) scan.3 Fetal assessment should include evaluation of cardiac activity and examination for possible injuries. Performing FAST poses a challenge under these circumstances, owing to the distorted pelvic view from the gravid uterus; therefore, evaluating the pouch of Douglas for hemoperitoneum requires skill and experience. Moreover, potential hemorrhage from solid organ injury, amniotic fluid from uterine rupture, or both can make it difficult to distinguish the etiology of free intraperitoneal fluid with FAST.4
FAST is indicated in hemodynamically unstable pregnant patients, as it can efficiently determine the presence of intra-abdominal free fluid that requires exploratory laparotomy. FAST has an overall sensitivity of 61%–83% for detection of free fluid, although this varies by trimester.1 Serial FAST examinations raise overall sensitivity to 72%–93%.4 A study by Richards, et al, found that sensitivity and specificity of FAST was highest in the first trimester of pregnancy, and declined in the second or third trimester.13 Despite these findings, the negative predictive value of FAST remained relatively high (above 95%) regardless of gestational age.5 FAST is especially useful in the initial assessment of pregnancy trauma during the first trimester, particularly in hemodynamically unstable patients. In stable patients, on the other hand, FAST has limited sensitivity for detecting injuries that may require intervention.
Computed tomography is the preferred imaging modality for evaluating high-energy trauma, such as from a motor vehicle accident, in hemodynamically stable patients.2 Per the American College of Radiology (ACR) Appropriateness Criteria, single portal venous phase CT of the abdomen and pelvis with intravenous contrast is indicated in cases of life-threatening emergencies.6 Noncontrast CT is never indicated in these cases, owing to its low sensitivity for detecting solid-organ injuries. CT angiography (CTA) may be indicated in cases of unstable pelvic fractures with a high suspicion for arterial injury to help guide surgical or vascular intervention.6
Magnetic resonance imaging (MRI) is seldom used in the acute setting for initial evaluation of pregnant patients, owing to extended, and often delayed, acquisition time. In the setting of a stabilized patient who requires follow-up imaging, MRI may be useful in situations that require visualization of the spine and soft-tissue injuries. MRI is safe for use during pregnancy, as it presents no radiation to the fetus.7
Effects of Radiation on Pregnancy
In hemodynamically stable patients, contrast-enhanced CT (CECT) is indicated for assessment of suspected hollow- and solid-organ, vascular, and bony pelvic injuries.1,2 CECT is recommended by the ACR when the required information can only be acquired through the modality and when imaging may affect care management.3 In most cases, those two criteria are met in the setting of trauma in pregnancy.
Radiation exposure may affect the fetus in many ways; thus, CT should be used judiciously. For pregnant patients undergoing CT within the first two weeks of conception, the main risk is failure of blastocyst implantation.7 Beyond this point, the fetus is most vulnerable to radiation from the second through the twentieth weeks of gestation, when the fetus is rapidly developing; the primary concern is for teratogenesis.1,7 Therefore, CT should not be used during the first trimester except in life-threatening emergencies for which no other imaging modality is suitable.
The short-term risks of radiation exposure to a fetus include death, abnormal growth causing deformities, and intellectual underdevelopment.7 Long-term risks include a two-fold increased risk of fatal childhood cancer, from a baseline of 1 in 2000 to 1 in 1000.1,2 The expected exposure threshold for these risks to manifest is greater than 100 mGy of radiation; however, radiation doses do not exceed 50 mGy with any diagnostic imaging modality, including abdominopelvic CT.1,7 Hence, the radiation dose from imaging should not pose any of the aforementioned risks unless serial imaging is performed, which could exceed the radiation dose considered safe for fetal imaging.
CT Dose Reduction in Pregnancy
Although typical CT imaging doses do not exceed 50 mGy,1,4 caution should still be taken to keep radiation exposure to the fetus as low as reasonably achievable (ALARA) during these examinations. The most common method of reducing dose is to alter acquisition parameters by decreasing the milliamperage, kilovolt peak, and craniocaudal extent of acquisition.8 A wide pitch and narrow collimation can also help reduce the dose,8 as can employing a single-phase protocol if a multiphasic protocol is unnecessary. A lead shield may be used while obtaining CT images outside of the abdomen and pelvis; however, exposure to scattered radiation is minimal, as most of it is internal rather than external.8
Effects of Iodinated Intravenous Contrast on Fetal Development
Another aspect of CT imaging to consider during pregnancy is the use of iodinated contrast. While no teratogenic effects have been described following intravenous administration of iodinated contrast, iodine-based compounds can impact the thyroid gland of the fetus.7,9 The thyroid uses iodine to synthesize thyroid hormones; therefore, any iodine-containing drug should be used with caution during pregnancy due to the risk of iodine uptake leading to secondary hypothyroidism in the fetus. Congenital hypothyroidism occurs in 1 of every 4000 births; left untreated, the condition can lead to failure to thrive as well as mental and developmental impairments.9 The ACR recommends iodinated contrast media in pregnancy only when no acceptable alternative test is available, when the expected information to be obtained from the study is vital to the well-being of the mother and fetus, and when the referring physician deems it necessary based on their clinical judgement.9
Review of Cross-sectional Trauma Imaging in Pregnancy
Trauma is the leading cause of non-obstetrical maternal mortality and a significant cause of fetal loss.2 In the setting of trauma during pregnancy, there are two patients, the mother and the fetus, and the decision to use CT in these circumstances should consider the risks and benefits to both. In the acute setting, the primary concern for the treating physician should be for maternal benefit from early and accurate diagnosis. While the risk of radiation exposure to the fetus is of significant concern, the dose is low enough to pose no expected, tangible effects on the fetus. Given the infrequency with which cross-sectional imaging is performed during pregnancy, certain CT findings of normal physiologic changes may initially appear concerning to those unfamiliar with the normal appearance.
Normal Placental Appearance
The CT imaging appearance of a normal placenta will evolve with progression of pregnancy as follows:
First Trimester
Computed tomography should not be utilized to evaluate patients in their first trimester except under life-threatening circumstances. During this period, the placenta is almost indistinguishable from the myometrium, with a homogeneous appearance and indistinguishable smooth chorionic plates along the periphery of the uterine cavity.10,11 Depending on gestational age, the only indications of early pregnancy identifiable on CT may be endometrial thickening or a small, ovoid fluid collection representing a gestational sac.
Second Trimester
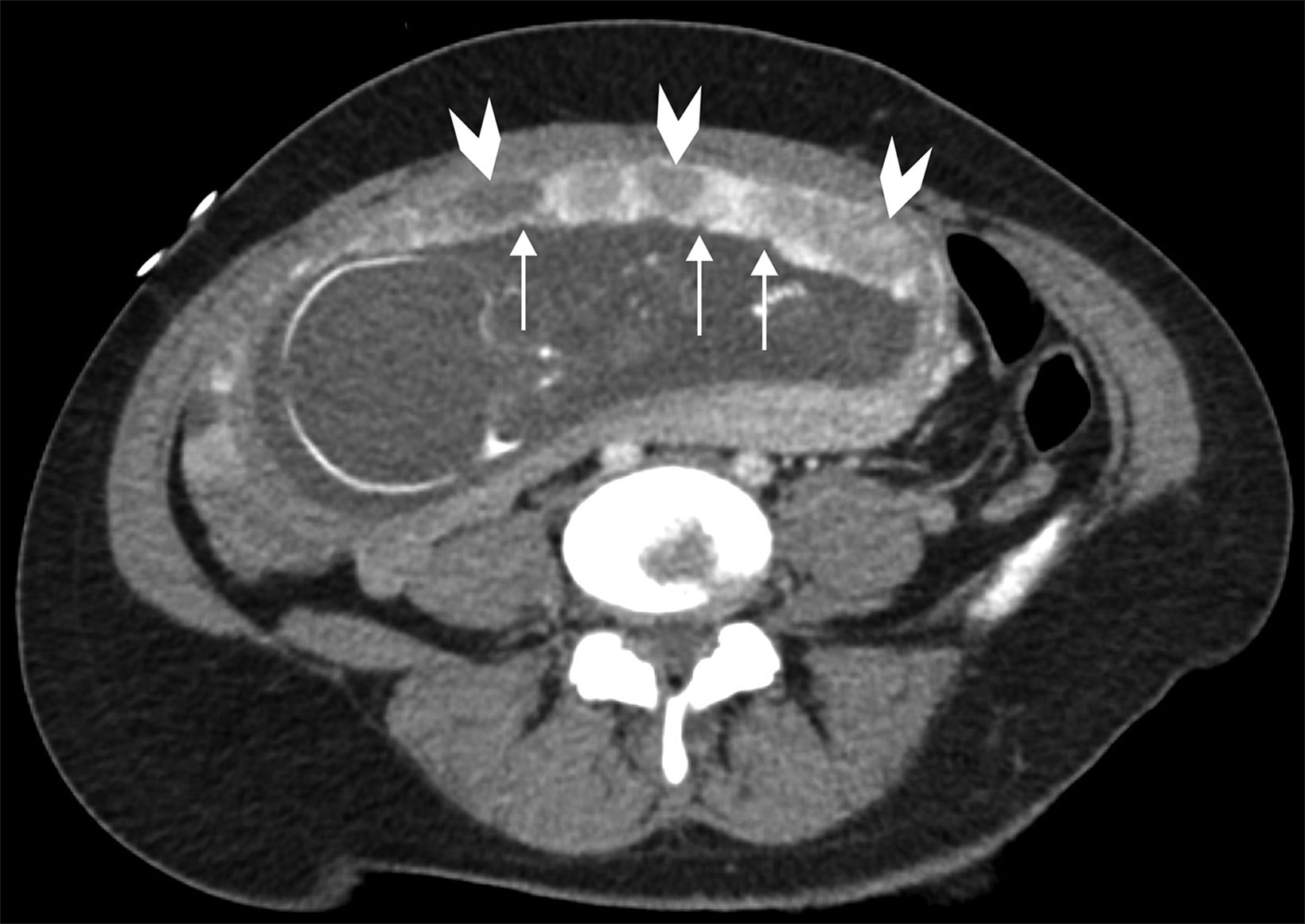
Throughout the second trimester, the placenta becomes heterogeneous in appearance and increases in attenuation relative to the myometrium.10 It is during the second trimester that placental cotyledons begin forming. These appear as multiple foci of low attenuation throughout the placenta (Figure 1).1,11 Chorionic plate indentations may begin appearing by the late second or third trimester as scattered, hypoattenuating indentations at the interface of the fetal surface of the placenta and the amniotic sac (Figure 1).1,10 Placental cotyledons and chorionic plate indentations share features with those of placental abruption, including hypoattenuation of placental tissue, although the lesion seen in placental abruption will involve the full placental thickness.
Third Trimester
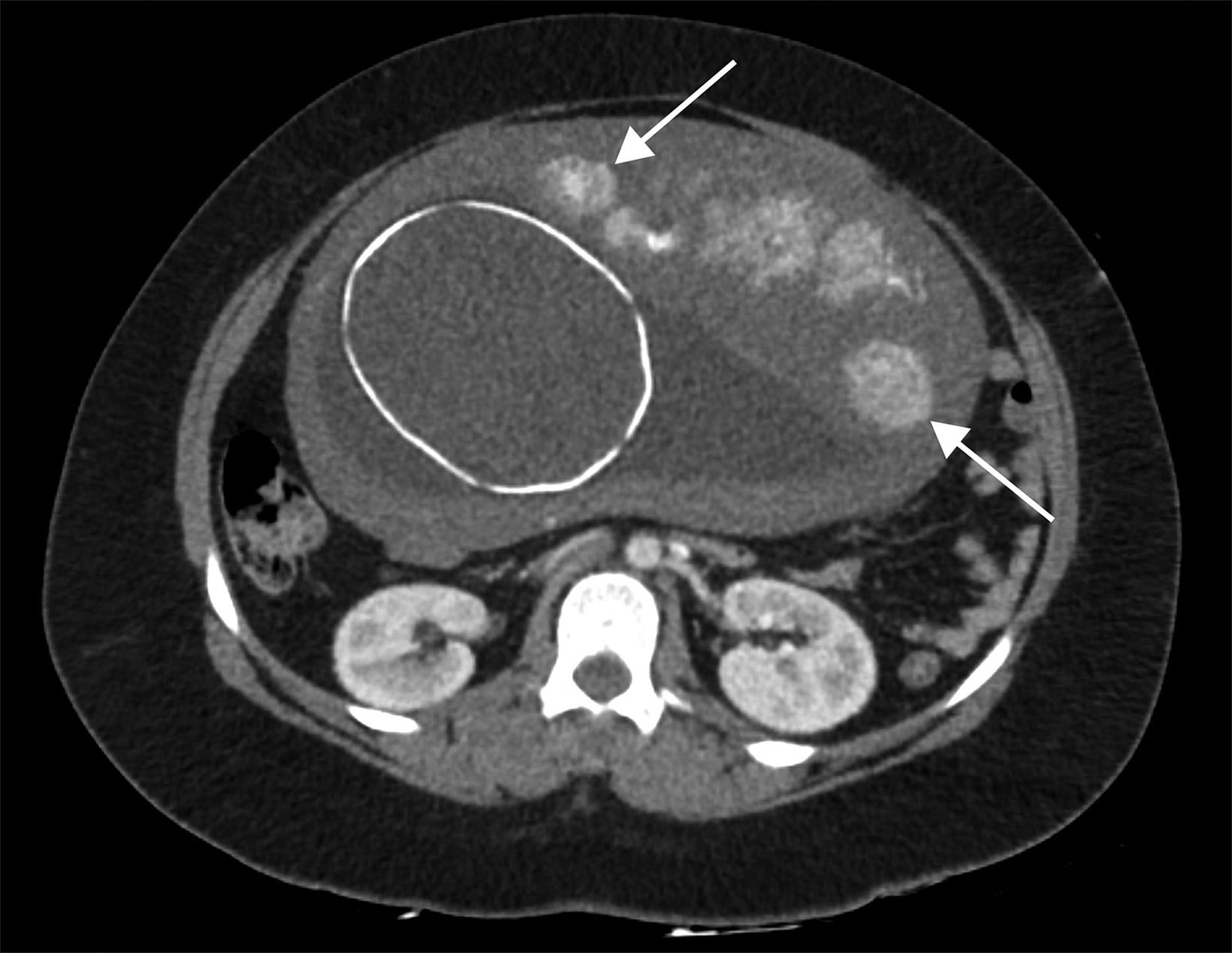
By this period, the placenta appears increasingly heterogeneous, with better visualization of the venous lakes. Also referred to as placental lakes, venous lakes are located on the maternal side of the placenta and appear as patchy regions of hyperdense foci or placental enhancement on CECT owing to their rich venous supply (Figure 2).1,2 Given their appearance, these may be mistaken for regions of placental hemorrhage.
Mimics of Placental Injury
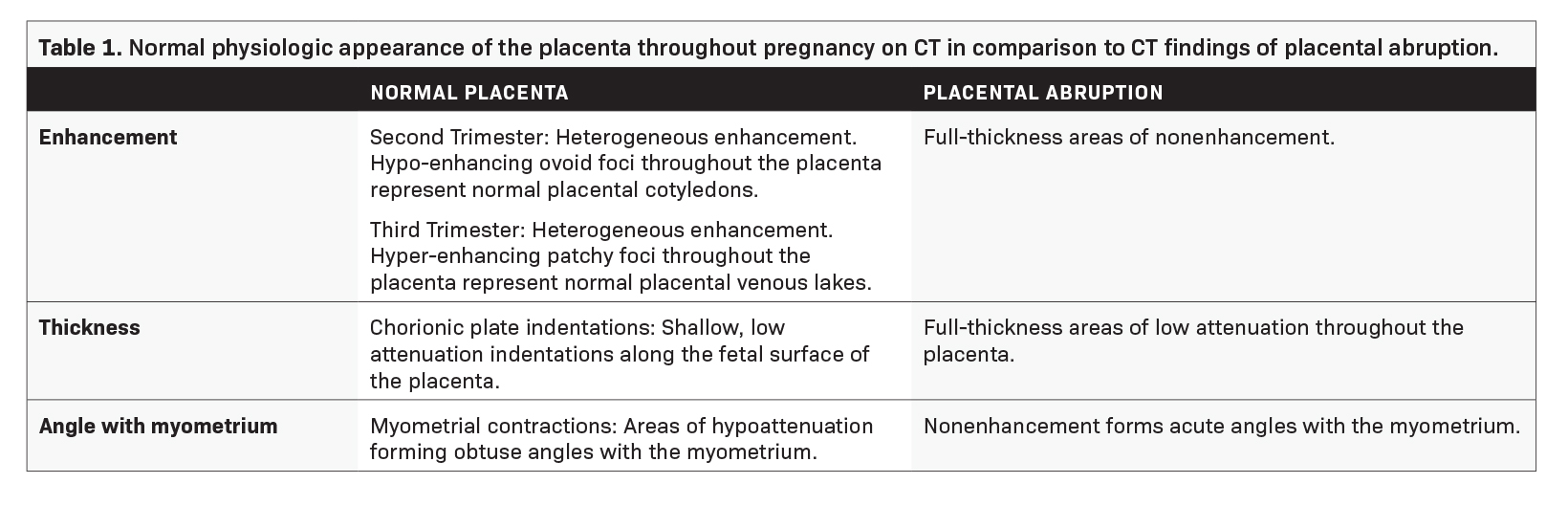
Given the evolving nature of the placenta, some its features on CT images can be misinterpreted as placental injury (Table 1).
Myometrial contractions typically appear hypoattenuating in comparison to the placenta. The angle of the hypoattenuation relative to the myometrium is the primary differentiator between injury and contractions; myometrial contractions tend to form obtuse angles with myometrial tissue, while injury such as abruption often forms acute angles.1,10
Chorionic plate indentations appear as scattered, low-attenuation, shallow, and wedge-shaped indentations along the fetal surface of the placenta (Figure 1).1,10 This is in contrast to placental abruption, which appears as full-thickness areas of low-attenuation or nonenhancement. Venous lakes may appear as areas of contrast blush on the maternal side of the placenta and can be mistaken for placental hemorrhage or abruption (Figure 2).1 Several retrospective and prospective studies have demonstrated that placental lakes are associated with increased placental thickness and do not confer any increased risk of gestational or placental complications.12,13
Wedge-shaped placental infarcts can appear as low-attenuation wedges along the periphery of the placenta as it matures and tend to have no clinical significance.10
During early pregnancy, subchorionic hemorrhages may also be visualized as low- to intermediate-density fluid immediately subjacent to the chorion; when small, they also tend to be clinically insignificant.1,10
Pregnancy-related Injuries
One of the most common pregnancy-related injuries during the second and third trimesters is placental abruption, which may occur in up to 50% of major traumas.1 Abruptions related to trauma have a high fetal mortality ranging from 67% to 75%.1 The diagnosis is primarily clinical, with signs and symptoms including abdominal pain, uterine contractions, and non-reassuring fetal heart rates. Ultrasound may be used to identify placental hematomas, but the modality has poor sensitivity compared to CT.6,10 Placental abruption on CT images appears as a full-thickness area of nonenhancing placenta that forms an acute angle with the myometrium (Figure 3).1,10
The most troubling traumatic obstetrical injury is uterine rupture, which occurs in 0.6% of all maternal injuries and carries a high risk of mortality for both the fetus and the mother.3 Patients typically present with hemodynamic instability, sudden severe abdominal pain, palpable fetal parts, and non-reassuring fetal heart rates. Imaging can help confirm diagnosis by showing endometrial or myometrial defects, intraperitoneal fetal parts, and possible extrauterine hematoma, for which urgent laparotomy is warranted.8
Other Modalities Used to Image Trauma During Pregnancy
Following CT imaging for initial assessment, follow-up sonography or MRI can be used during pregnancy to reduce the cumulative radiation dose that results from repeated CT examinations. Importantly, while ultrasound can assist in diagnosis, the modality is insensitive for placental abruption and a negative examination does not exclude this diagnosis.1,3 Ultrasound is preferred in fetal assessment, while MRI allows for improved soft-tissue evaluation and can be used to evaluate the pelvic anatomy and the fetus.
Conclusion
Given the high mortality rate of nonobstetrical trauma to both mother and fetus, CT should be utilized only after discussing the risks and benefits with the patient and care team. Computed tomography visualizes greater anatomic detail than does ultrasound, and it is superior to MRI with respect to availability and the time required for examination. The imaging appearance of the placenta evolves throughout pregnancy; not all radiologists may be aware of the expected CT findings of a normal placenta, as the modality is rarely used during pregnancy. Radiologists should be aware of the changing appearance of the normal placenta to avoid confusing these features with those of placental injury.
Subsequent ultrasound or MR imaging may be performed to further evaluate or monitor findings suspicious for uterine or placental injury.
References
- Raptis CA, Mellnick VM, Raptis DA, et al. Imaging of trauma in the pregnant patient. Radiographics, 2014;34(3):748-763. doi: 10.1148/rg.343135090.
- Sadro C, Bernstein MP, Kanal KM. Imaging of trauma: Part 2. Abdominal trauma and pregnancy — a radiologist’s guide to doing what is best for the mother and baby. Am J Roentgenol, 2012;199(6):1207-1219. doi: 10.2214/AJR.12.9091.
- Jain V, Chari R, Maslovitz S, et al. Guidelines for the management of a pregnant trauma patient. J Obstet Gynaecol Can. 2015;37(6):553-574. doi: 10.1016/s1701-2163(15)30232-2.
- Richards J, McGahan J. Focused assessment with sonography in trauma (FAST) in 2017: what radiologists can learn. Radiology, 2017;283(1):30-48. doi: 10.1148/radiol.2017160107.
- Richards JR, Ormsby EL, Romo MV, Gillen MA, McGahan JP. Blunt abdominal injury in the pregnant patient: detection with US. Radiology, 2004;233(2):463-470. doi:10.1148/ radiol.2332031671.
- Expert Panel on Major Trauma Imaging, Shyu JY, Khurana B, et al. ACR Appropriateness Criteria® Major Blunt Trauma. J Am Coll Radiol, 2020;17(5S):S160-S174.doi:10.1016/j.jacr.2020.01.024.
- Chen MM, Coakley FV, Kaimal A, Laros RKJr. Guidelines for computed tomography and magnetic resonance imaging use during pregnancy and lactation. Obstet Gynecol, 2008;112:333-340.
- Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental imaging: normal appearance with review of pathologic findings. Radiographics, 2017;37(3):979-998. doi: 10.1148/rg.2017160155.
- Tremblay E, Thérasse E, Thomassin-Naggara I, Trop I. Quality initiatives: guidelines for use of medical imaging during pregnancy and lactation. RadioGraphics, 2012;32(3):897-911. doi:10.1148/rg.323115120.
- Wei SH, Helmy M, Cohen AJ. CT evaluation of placental abruption in pregnant trauma patients. Emerg Radiol. 2009;16(5):365-373. doi: 10.1007/s10140-009-0804-z.
- Elsayes KM, Trout AT, Friedkin AM, et al. Imaging of the placenta: a multimodality pictorial review. Radiographics, 2009;29(5):1371-1391. doi: 10.1148/rg.295085242.
- hompson MO, Vines SK, Aquilina J, Wathen NC, Harrington K. Are placental lakes of any clinical significance?. Placenta, 2002;23(8-9):685-690. doi: 10.1053/plac.2002.0837.
- Hwang HS, Sohn IS, Kwon HS. The clinical significance of large placental lakes. Eur J Obstet Gynecol Reprod Biol, 2012;162(2):139-143. doi: 10.1016/j.ejogrb.2012.02.015.
References
Citation
K Z, M K, H W, B T, N M, Y L, B H, L A,. Trauma Imaging in Pregnancy: A Review of the Evolving Appearance of the Placenta on CT and Mimics of Placental Injury. Appl Radiol. 2022;(6):7-12.
April 26, 2022