Study Compares FDG-PET/CT and CT for Treatment Evaluation in Patients With Unresectable Pleural Mesothelioma
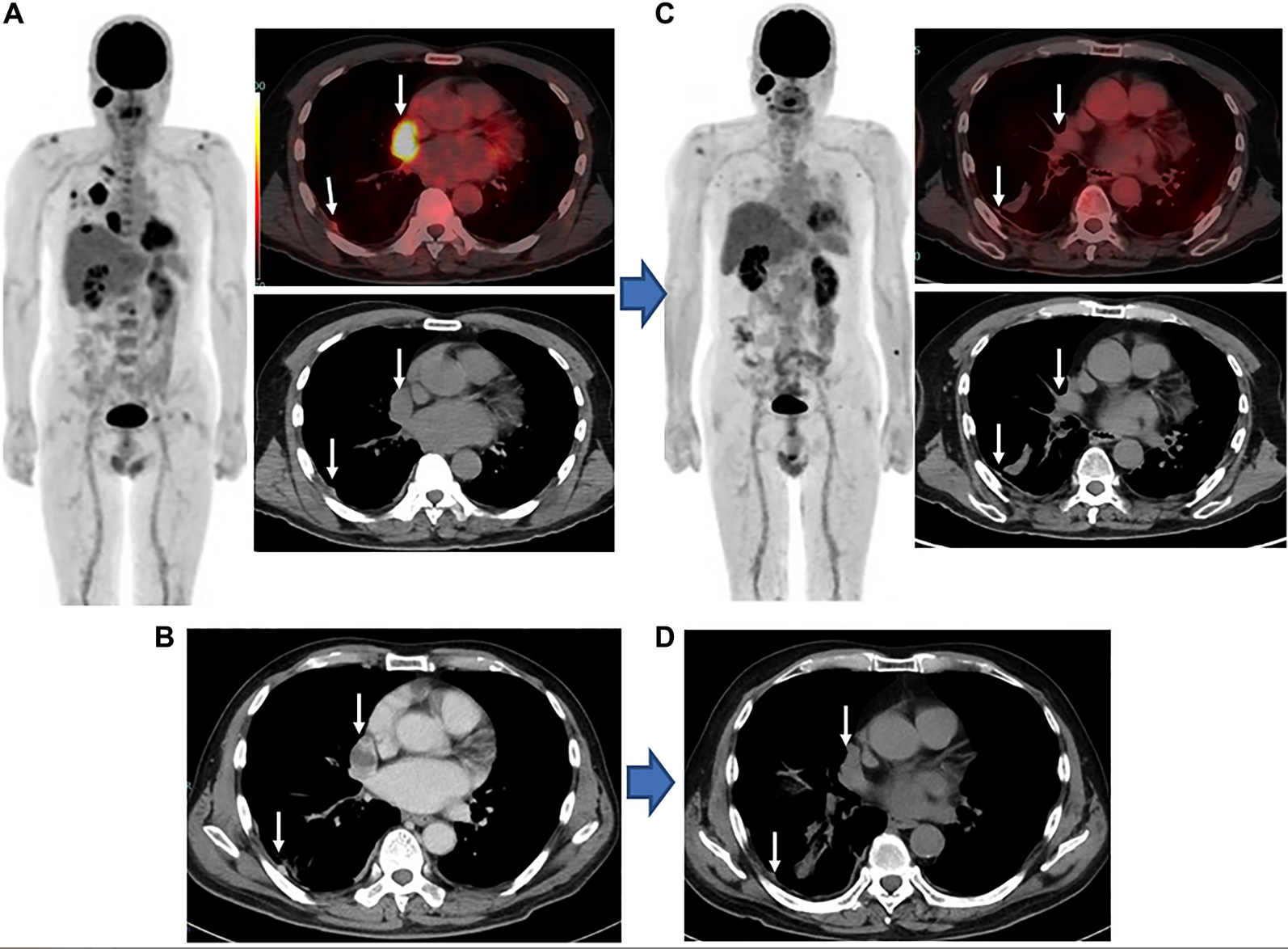
Images
A study published in Oncotarget reports that both FDG-PET/CT (imPERCIST) and CT (mRECIST) results were found useful for evaluating the response of tumors to the combination of nivolumab and ipilimumab (approximately three cycles) used as first-line therapy, and also progression prediction in patients with unresectable malignant pleural mesothelioma (MPM).
Malignant pleural mesothelioma (MPM) is an aggressive neoplasm and affected patients have low survival rates. In this new retrospective study, researchers from Hyogo Medical University and Kindai University Faculty of Medicine examined the effectiveness of fluorodeoxyglucose positron emission tomography (FDG-PET) criteria, i.e., immunotherapy-modified PET response criteria in solid tumors (imPERCIST), with morphological computed tomography (CT) criteria, i.e., modified response evaluation criteria in solid tumors (mRECIST), to evaluate patients with unresectable MPM undergoing nivolumab plus ipilimumab combination therapy as first-line treatment regarding response and prognosis prediction.
“Results for malignant pleural mesothelioma (MPM) patients following first-line treatment with nivolumab plus ipilimumab obtained with immunotherapy-modified PERCIST (imPERCIST), shown by [18F] (FDG-PET/CT), and modified RECIST (mRECIST), shown by CT, were compared for response evaluation and prognosis prediction,” the authors wrote.
Twenty-six patients (23 males, 3 females; median 73.5 years) with histologically proven MPM and no curative surgery received nivolumab plus ipilimumab combination therapy. FDG-PET/CT and diagnostic CT scanning at the baseline, and after 2–4 cycles (2 in three, 3 in 17, 4 in six patients) were performed. Therapeutic response findings evaluated using imPERCIST and mRECIST were compared. PFS and OS analyses were done using log-rank and Cox methods.
Results: imPERCIST indicated nine progressive metabolic disease (PMD), eight stable metabolic disease (SMD), four partial metabolic response (PMR), and five complete metabolic response (CMR) cases. mRECIST showed nine with progressive disease (PD), nine stable disease (SD), seven partial response (PR), and one complete response (CR). Although high concordance was noted (κ = 0.827), imPERCIST correctly judged a greater percentage with CMR (15.4%). Following a median 10.0 months, 15 patients showed progression and eight died from MPM. With both, progression-free survival (PFS) and overall survival (OS) were significantly longer in patients without progression (CMR/PMR/SMD, CR/PR/SD, respectively) as compared to PMD/PD patients (imPERCIST p < 0.0001 and p = 0.015, respectively; mRECIST p < 0.0001 and p = 0.015, respectively).
The authors concluded, “For unresectable MPM patient examinations, FDG-PET and CT provide accurate findings for evaluating tumor response and also prognosis prediction following first-line nivolumab plus ipilimumab immunotherapy (approximately three cycles).”