Studies Find Lunit AI Predicts Breast Cancer Risk up to Six Years in Advance, Reduces Radiologist Workload
Images
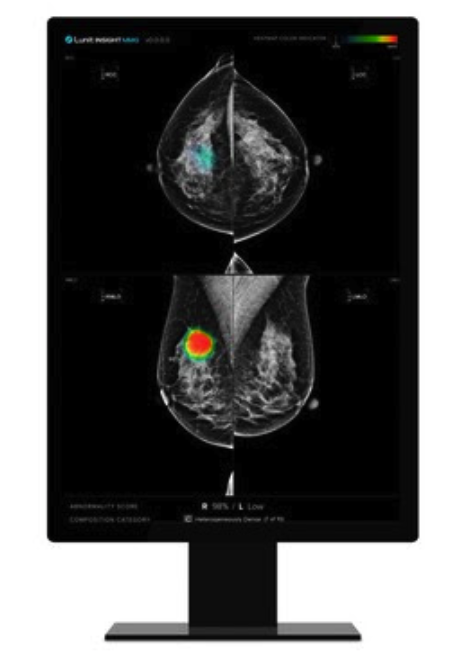
A study conducted by researchers at the Cancer Registry of Norway and Odense University Hospital in Denmark, published in JAMA Network Open, and led by Professor Solveig Hofvind, evaluated how Lunit INSIGHT MMG could estimate the development of future cancer. The research analyzed data from 116,495 women aged 50-69 who underwent at least three consecutive biennial screening rounds at 9 breast centers in Norway. The research found that Lunit INSIGHT MMG can estimate future breast cancer risk up to 4 to 6 years before it becomes detectable.
Lunit's AI assigns each breast a score from 0 to 100, with higher values indicating a greater likelihood of cancer being present on the current mammogram. The study found that the mean AI scores were consistently higher for breasts that developed cancer compared to those that remained cancer-free, even 4 to 6 years before detection. Over multiple screening rounds, the gap in these AI scores between breasts that developed cancer and those that did not grew larger, indicating the AI's ability to detect subtle signs of cancer earlier.
Specifically, for women who developed screen-detected cancer, the mean absolute differences in AI scores between the two breasts were 21.3 in the first study round, 30.7 in the second, and 79.0 in the third. Additionally, Lunit's AI achieved an Area Under the Curve (AUC) for the absolute difference of 0.63, 0.72, and 0.96 across the three screening rounds for screen-detected cancer. These findings indicate that Lunit's AI can effectively identify early signs of cancer and offer a pathway for personalized screening approaches.
In another study led by Dr Mohammad T. Elhakim and published in Radiology: Artificial Intelligence, explored how Lunit INSIGHT MMG could enhance double reading without compromising screening performance. The research team evaluated three AI-integrated screening scenarios on 249,402 mammograms, demonstrating significant reductions in radiologist workload while either maintaining or improving accuracy (Scenario 1: AI replaced first reader; Scenario 2: AI replaced second reader; Scenario 3: AI replaced both for triaging of low and high-risk cases).
Results showed that replacing the first, second, or both radiologists with Lunit's AI could reduce reading volume by 48.8%, 48.7%, and 49.7%, respectively, while maintaining or improving cancer detection accuracy. Most notably, the AI triage scenario (Scenario 3) achieved higher sensitivity, positive and negative predictive values with a lower arbitration rate when compared to standard double reading. This result highlights that by utilizing Lunit INSIGHT MMG, healthcare systems can significantly reduce radiologists' burden without compromising the screening program's diagnostic performance quality, allowing them to focus on more complex cases and improving overall efficiency.
"These studies provide compelling evidence of our AI's potential to transform breast cancer screening," said Brandon Suh, CEO of Lunit. "In Norway, our AI identified future breast cancer risk up to 6 years ahead, providing women and healthcare providers valuable time for proactive interventions. The Danish study showed a 50% reduction in radiologist workload without sacrificing detection quality—a result that directly impacts radiology efficiency worldwide. These are not hypothetical improvements; they represent concrete benefits that healthcare providers and patients are experiencing today. Our focus is on ensuring these advancements translate directly to better outcomes for women undergoing breast cancer screening."