Small Study Identifies Brain Region Where Breathing Failure Occurs After Seizure
Images
University of Iowa researchers supported by the National Institutes of Health has identified a part of the brain that may be associated with breathing failure following a seizure in people with severe epilepsy that cannot be controlled with medication. The condition, known as sudden unexpected death in epilepsy (SUDEP), is the leading cause of death in this patient population. The new findings, published in JCI Insight, may play a critical role in understanding SUDEP, for which causes are not well-explained.
Most cases of SUDEP are thought to be due to loss of breathing that occurs after a seizure ends, known as postictal apnea. The study found that individuals who experience postictal apnea lose a sense of “air hunger” – the primal urge to breathe – or alarm, suggesting that the brain may be unable to detect and respond to rising carbon dioxide (CO2) levels in the blood when the apnea occurs.
To examine this, researchers enrolled 12 adults and eight children with epilepsy that could not be controlled with medications, and who were undergoing intracranial electroencephalography (iEEG) in an attempt to control their seizures. iEEG involves placing electrodes inside the skull to record electrical activity from the brain and to locate where seizures are starting. Using direct electrical stimulation, the team induced seizures in the participants under medical supervision to examine forebrain control of breathing and apnea. They found that seizures that originate in the amygdala, a brain region primarily involved in processing emotion and fear, can cause postictal apnea and identified the amygdala subregion involved in prolonged breathing loss. Only five of the 20 participants developed postictal apnea, suggesting that some individuals with uncontrolled seizures may be more prone to the condition.
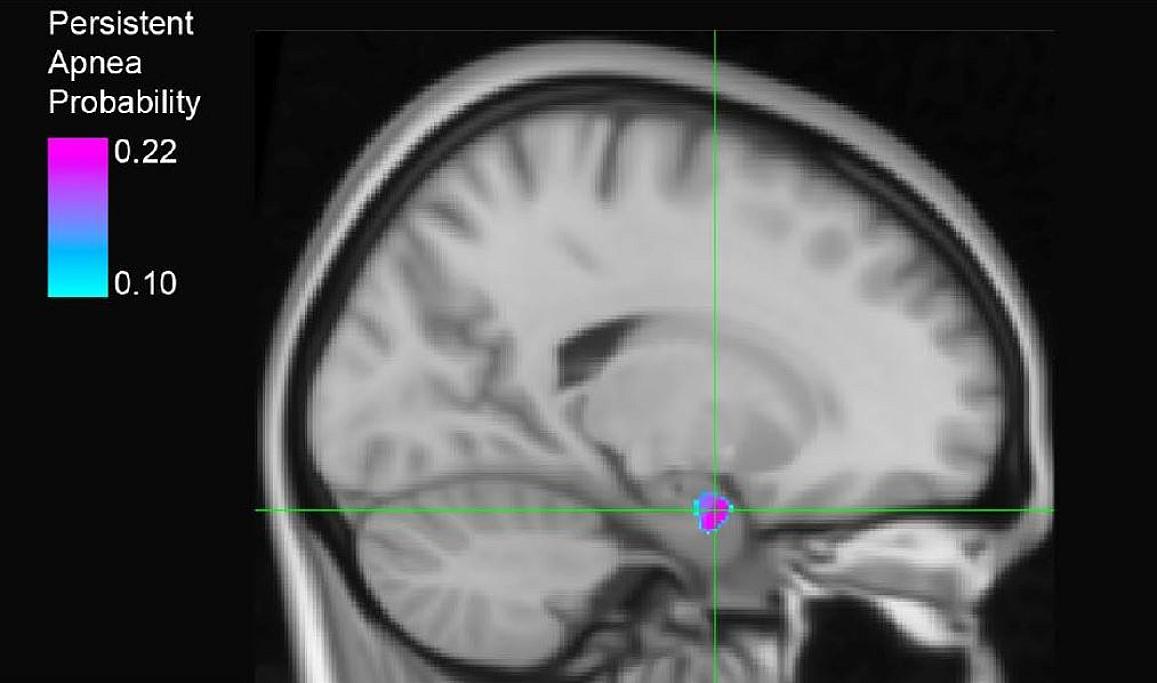
The scientists then used a technique combining electrical stimulation with functional MRI to identify novel connections between the amygdala site and the brainstem region critical for sensing changes in blood CO2 levels and controlling breathing. Taken together, the findings suggest that seizure activity in a subregion of the amygdala can suppress breathing and air hunger for prolonged periods of time following seizure. This is likely controlled via connections with the brainstem and other brain sites involved in sensing signals from the body. Additional studies are needed to confirm the role of the amygdala in breathing suppression and its involvement in SUDEP.
The findings further increase understanding of SUDEP and may help uncover preventative treatments and identify those most at risk. The study was funded in part by the National Institute of Neurological Disorders and Stroke (NINDS), part of NIH.
Related Articles
Citation
Small Study Identifies Brain Region Where Breathing Failure Occurs After Seizure. Appl Radiol.
October 9, 2023