Shoulder Effusion as Ultrasound Mimic of Axillary Lymphadenopathy
Images
Case Summary
A woman with biopsy-proven invasive ductal carcinoma in the left breast and a metastatic left axillary lymph node presented following presurgical neoadjuvant chemotherapy for placement of an axillary localization device. During pre-procedural ultrasound (US) imaging, the axillary mass, initially queried as the metastatic lymph node, was characterized as a benign shoulder effusion. In this case, we discuss common axillary ultrasound findings and distinguishing characteristics.
Imaging Findings
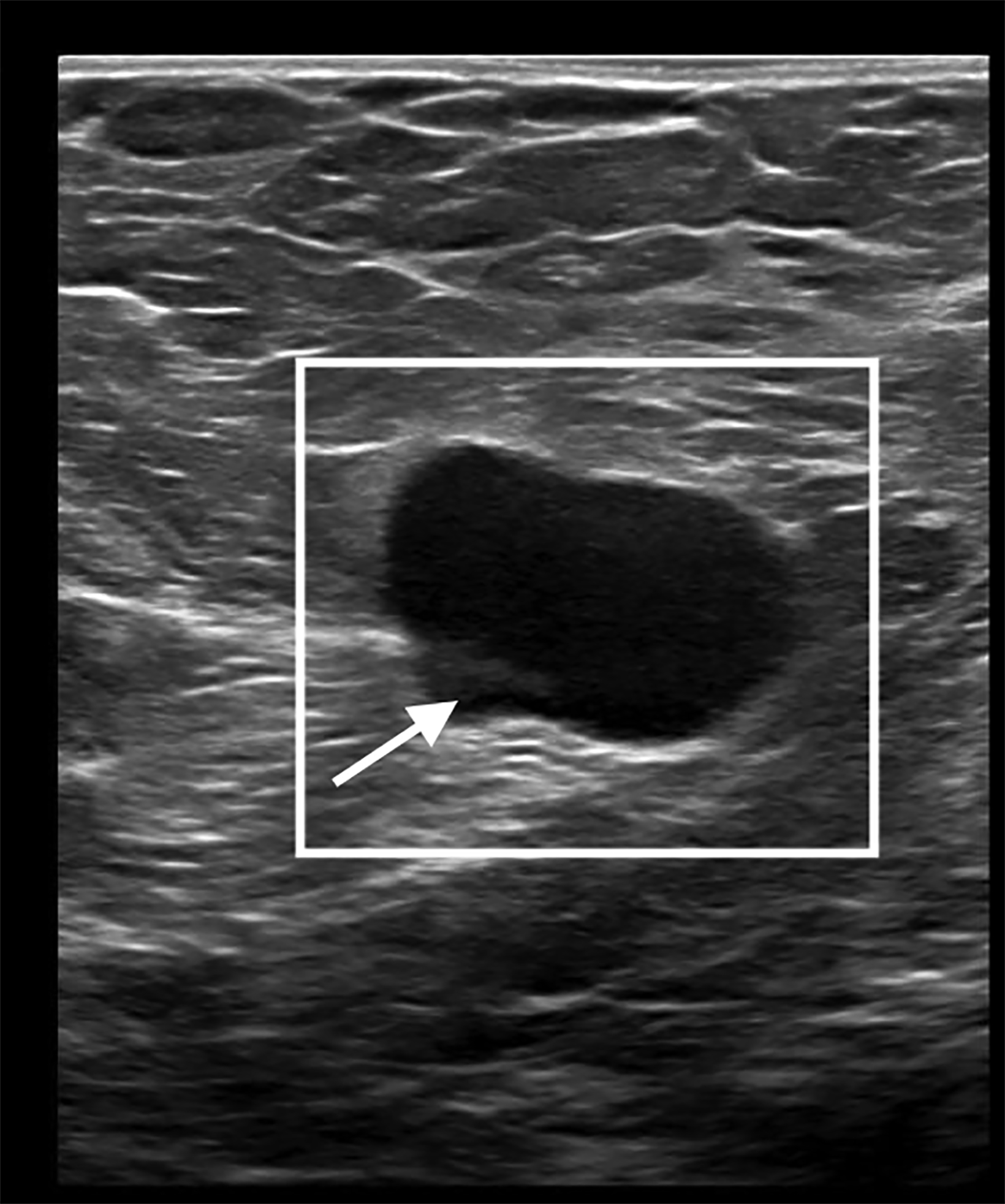
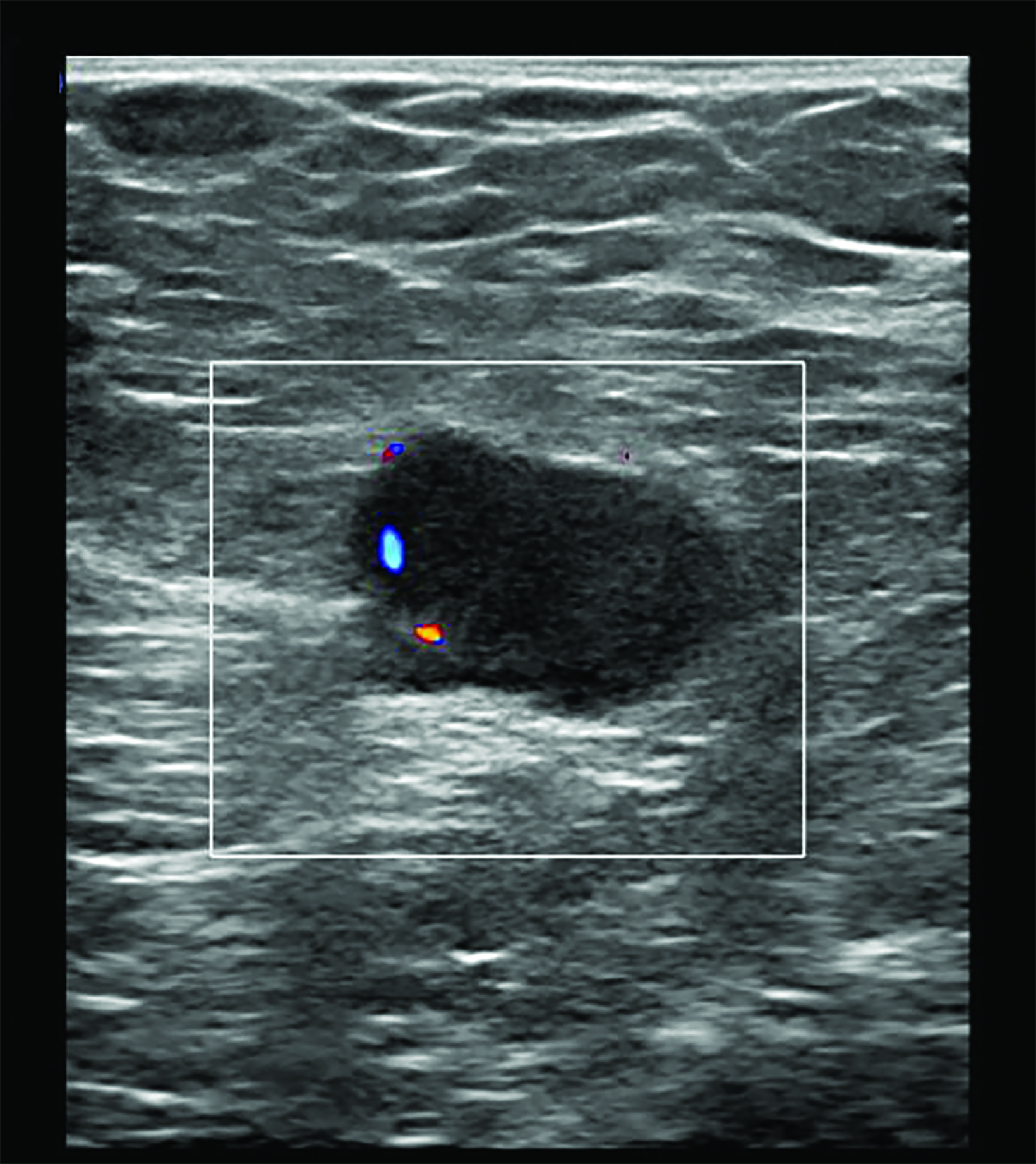
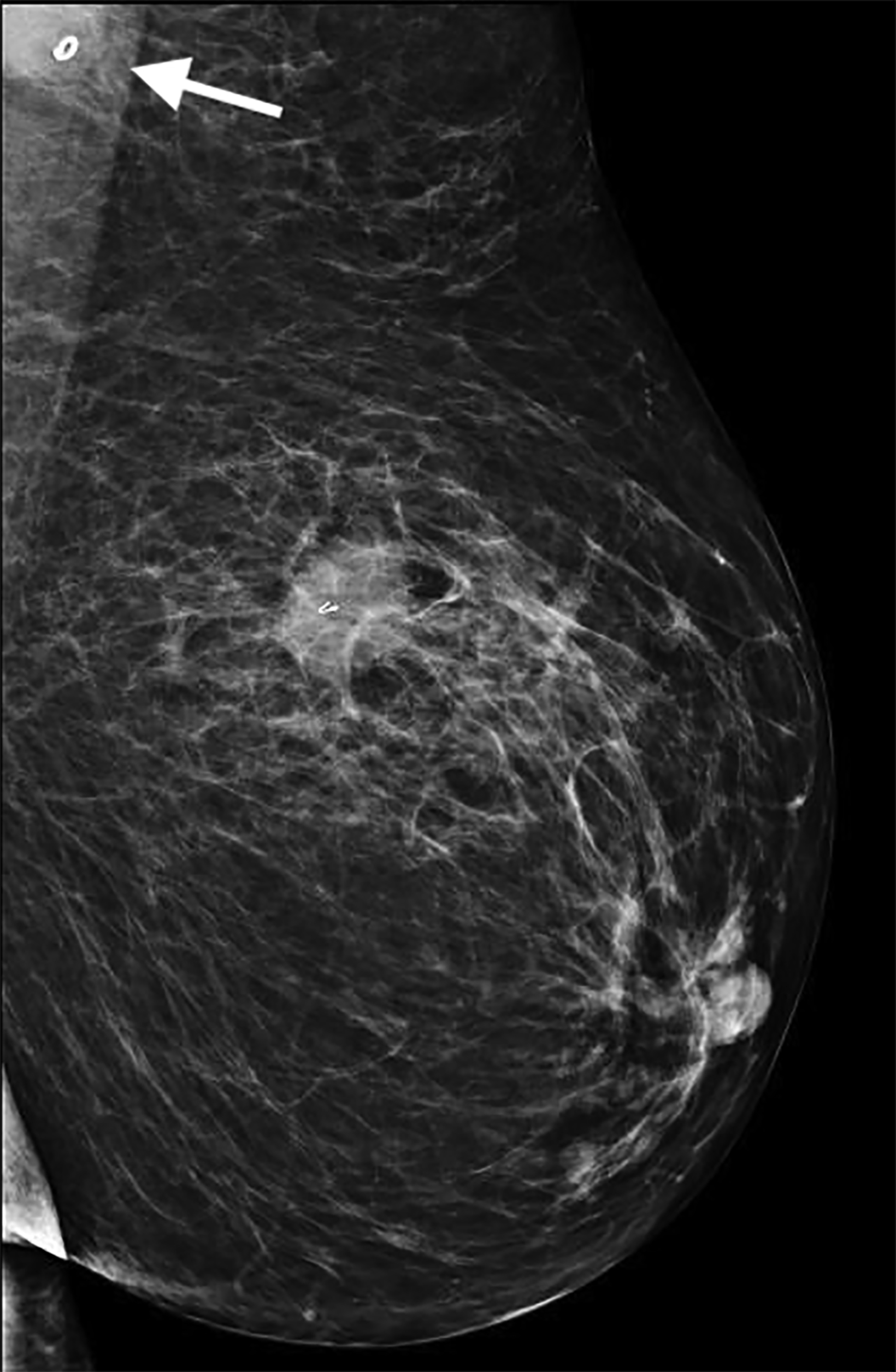
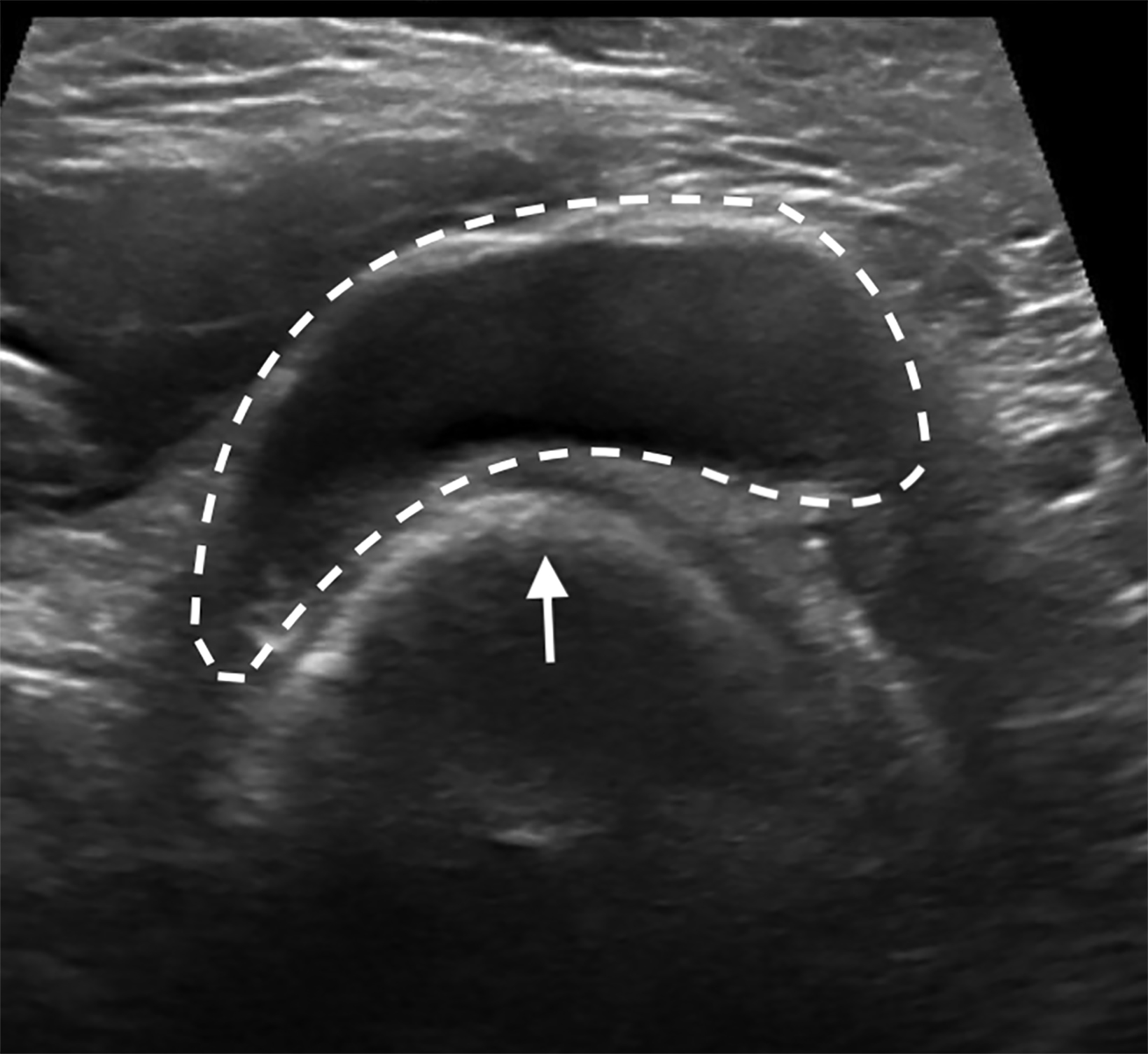
Initial US evaluation (Figure 1) obtained 6 months prior to surgery demonstrated an enlarged left axillary lymph node with abnor- mal cortical thickening and internal vascularity. This was subsequently biopsied, with pathology demonstrating metastatic breast cancer. A post-biopsy mammogram (Figure 1) demonstrated an appropriately placed biopsy clip within the lymph node.
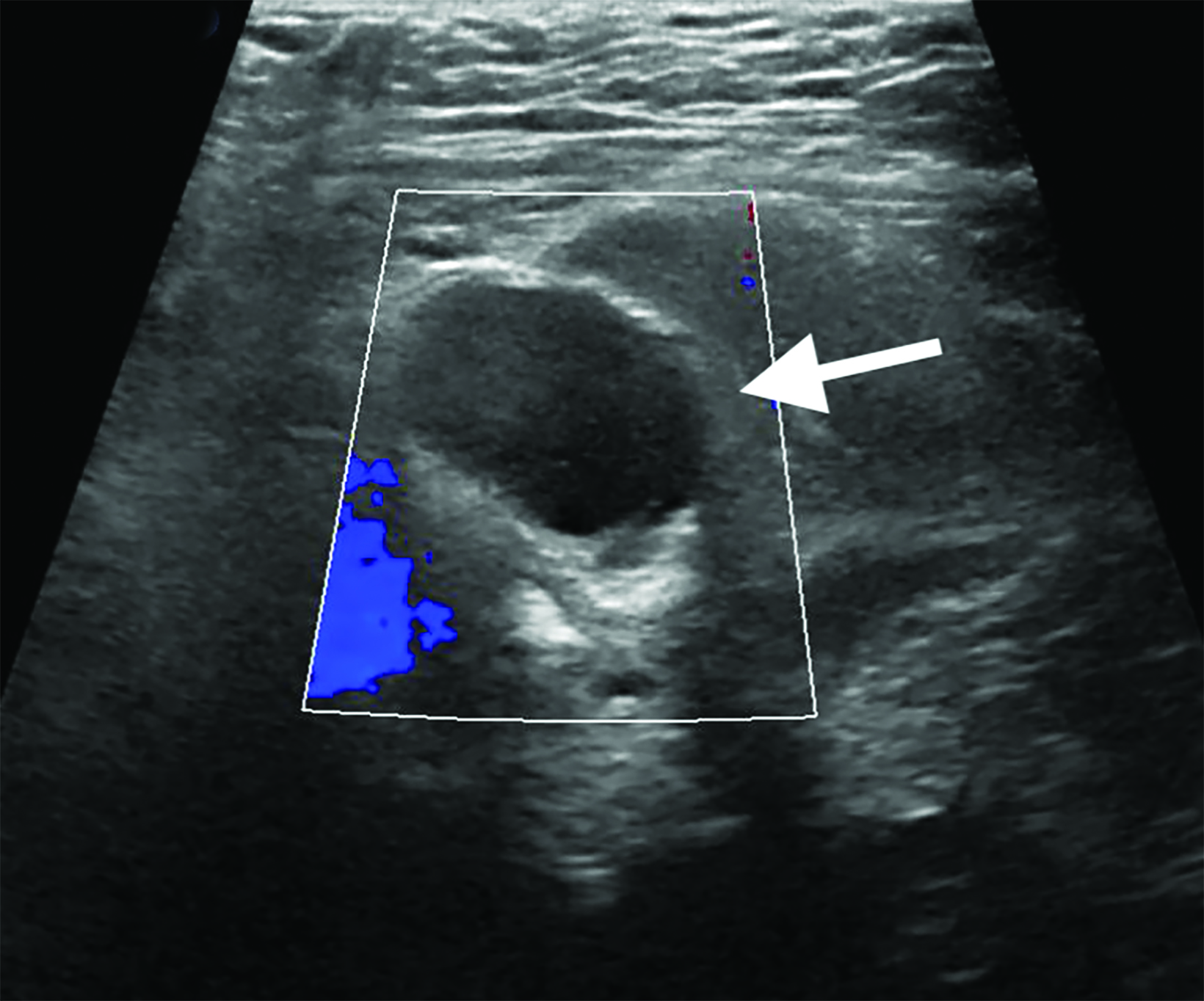
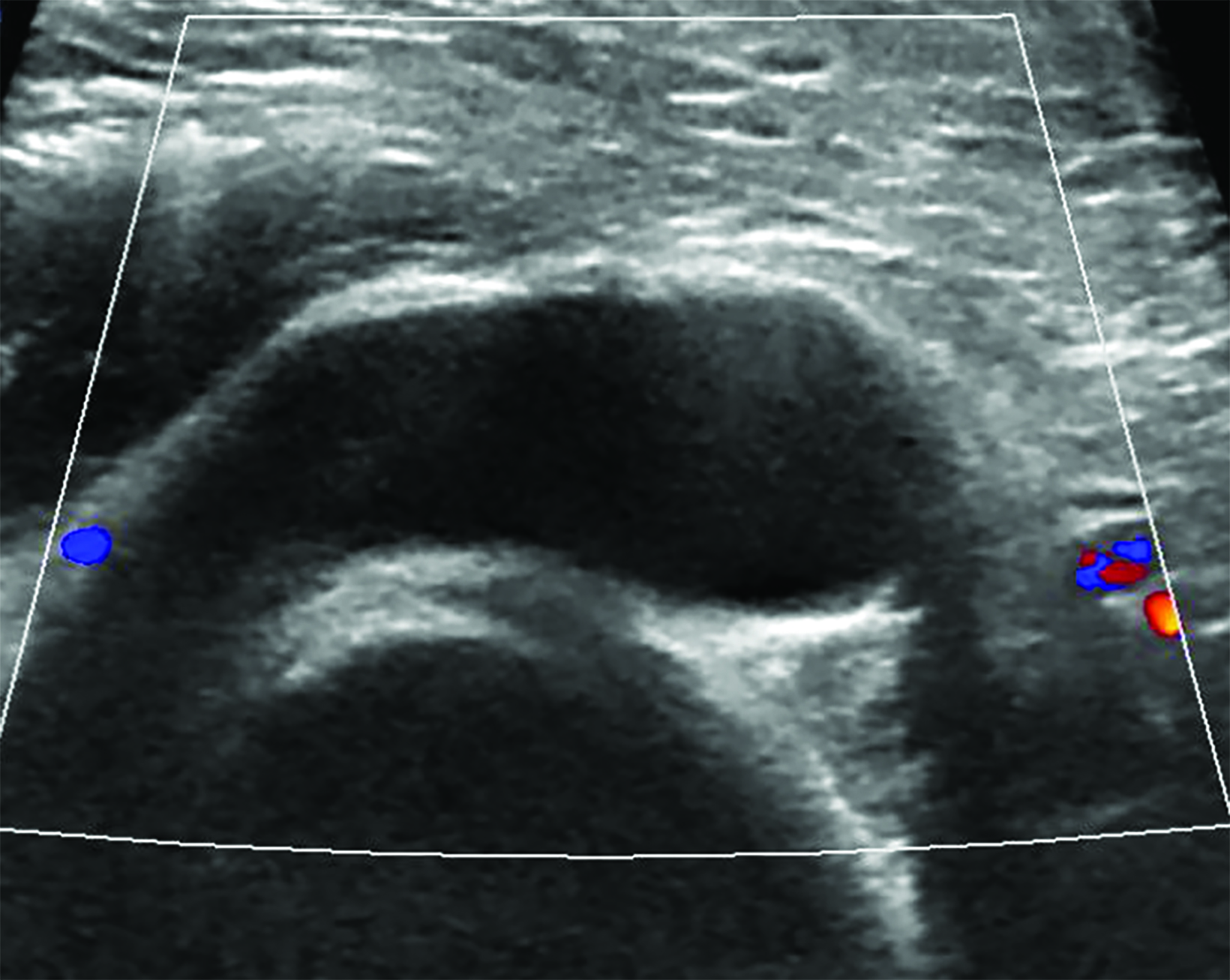
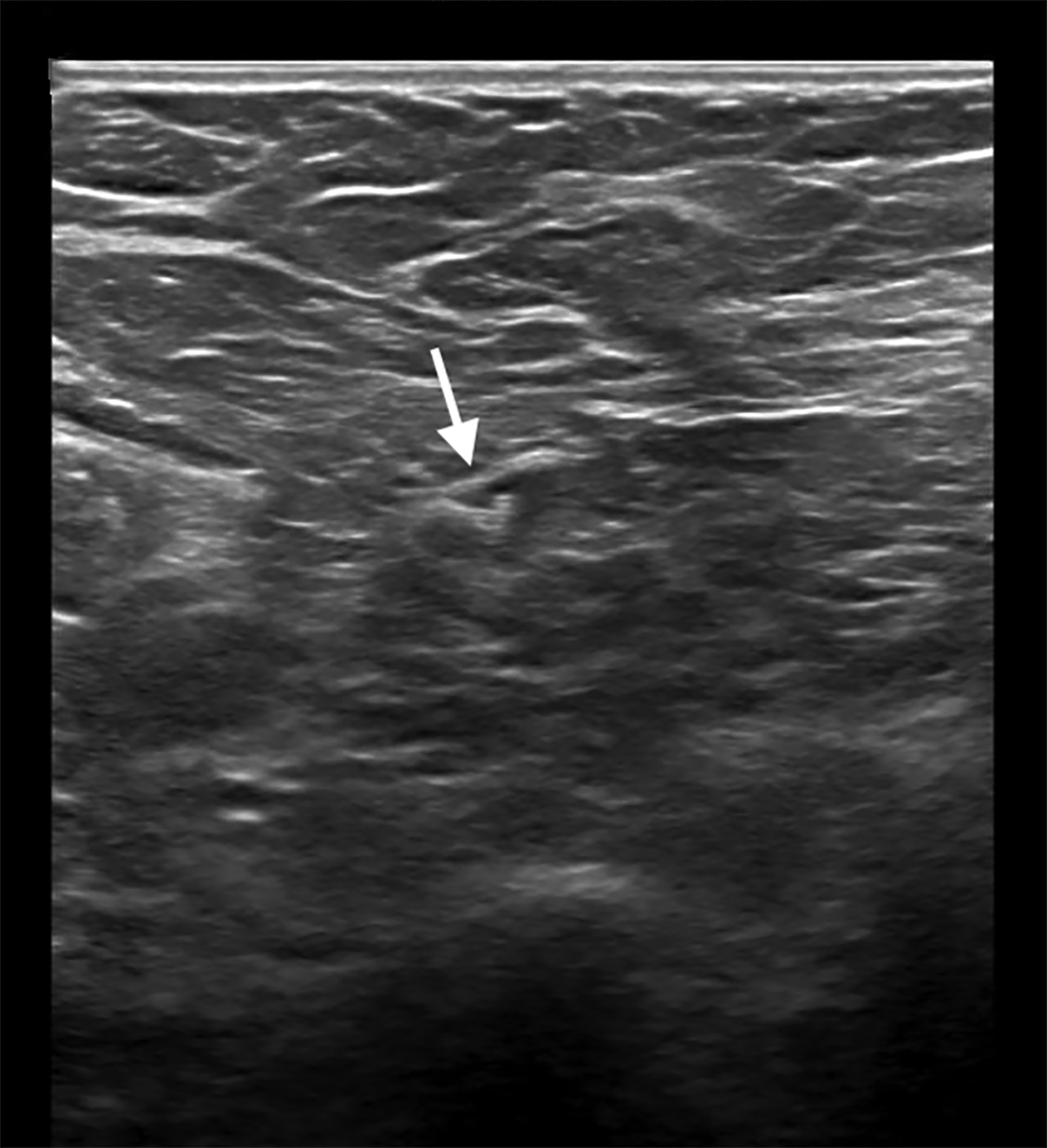
The patient underwent neoadjuvant chemotherapy for breast cancer prior to surgery. Pre-procedural US-guided localization of the metastatic node on the day of surgery (Figure 2) demonstrated a nearly anechoic, avascular oval mass in the left axilla with increased through transmission. Further imaging demonstrated its location adjacent to the humeral head with a tear-drop appearance and lack of internal vascularity. These findings are characteristic of a joint effusion. The prior biopsy site was later identified inferiorly in the axillary space as a normalized lymph node with central hyperechoic fatty hilum and cortical thickness measuring less than 3 millimeters. The echogenic biopsy clip was also visible in the node. This node was successfully localized and excised at surgery.
Diagnosis
Shoulder effusion as a mimic of axillary lymphadenopathy. The differential diagnosis includes benign and malignant causes of axillary lymphadenopathy, soft-tissue masses, synovial hypertrophy, and post-procedural seroma.
Discussion
Axillary ultrasound is often performed during breast imaging workup for suspected axillary pathology such as lymphadenopathy or for a palpable mass. Commonly described etiologies of pathology in the axilla include benign and malignant causes of lymphadenopathy, soft-tissue masses, and postsurgical or posttraumatic fluid collections.1,2 Given the proximity of the axillary space to the shoulder, musculoskeletal pathology should be considered within this broad differential. Here, we present an uncommon mimic of axillary lymphadenopathy caused by a shoulder effusion.
Ultrasound imaging of the axilla may play an integral role in management of newly diagnosed breast cancer during initial staging assessment, image-guided biopsy of a suspicious abnormality, assessment of treatment response, and image-guided localization for surgery.2-4 Malignant lymph node involvement may be characterized by eccentric or diffuse cortical thickening, effacement of the normal central fatty hilum, and loss of the normal nodal contour with a uniformly hypoechoic echotexture. Considering morphologic criteria alone, US has a sensitivity of 26-76% and a specificity of 88-89% for the detection of nodal malignancy.4
In breast cancer, ipsilateral axillary lymphadenopathy is concerning for nodal metastasis. However, a broad differential diagnosis should be considered when approaching axillary space pathology. These include alternative etiologies for lymphadenopathy such as benign reactive hyperplasia from infection or vaccines, underlying connective tissue disease, granulomatous disease, or other malignancies such as lymphoma.
The appearance of other axillary masses may also be difficult to differentiate from lymphadenopathy. These include mesenchymal soft-tissue masses such as peripheral nerve sheath tumors, postsurgical or posttraumatic fluid collections such as seromas and hematomas, or breast masses like fibroadenomas arising from axillary breast tissue. Joint pathology associated with the shoulder may not readily be considered in the differential diagnosis of axillary findings identified during breast imaging.
The axillary space relevant to breast pathology begins below the glenohumeral joint to include the axillary lymph node stations defined in relation to the pectoralis minor muscle.5 In musculoskeletal imaging, an axillary sonographic approach is uncommon but can be used as an adjunct in assessing the shoulder.6 An axillary approach may be helpful in characterizing inferior shoulder pathology, including joint effusions, synovial hypertrophy, and adhesive capsulitis. Axillary ultrasound has been shown to have a sensitivity of 89% and a specificity of 76% in the detection of joint effusions.7
A shoulder joint effusion imaged with US characteristically appears as an anechoic, avascular structure adjacent to the humeral head, with posterior acoustic enhancement. These features can overlap with the appearance of a malignant lymph node, particularly if the shoulder effusion contains complicated fluid resulting in hypoechoic echogenicity which can be mistaken for solid tissue.
The key distinguishing feature of a joint effusion from lymphadenopathy or other axillary mass is its location adjacent to the humeral head. Care should be taken during patient and probe positioning to avoid imaging at or above the level of the glenohumeral joint, where musculoskeletal lesions may be more apparent. Joint effusions may also decrease in size when pressure is applied to the transducer, which can displace the joint fluid. These diagnostic characteristics can easily be demonstrated on US without requiring further imaging workup.
Conclusion
Accurate detection and diagnosis of axillary lymphadenopathy is important, particularly in the context of breast cancer. During breast imaging the proximity of the axillary space to the shoulder raises the possibility of detecting musculoskeletal pathology. This is illustrated in our case of a shoulder joint effusion as an uncommon mimic of malignant axillary lymphadenopathy. Key distinguishing features that can aid in correctly identifying a shoulder joint effusion include its characteristic location adjacent to the humeral head, lack of internal vascularity, and potential for displacement with application of transducer pressure.
References
Citation
K S, EL L.Shoulder Effusion as Ultrasound Mimic of Axillary Lymphadenopathy. Appl Radiol. 2023; (6):52-54.
November 3, 2023