Researchers Use Macrophage-Adhering Gadolinium Micropatches to Visualize mTBIs
Images
Researchers have created a new brain imaging method that allows mild traumatic brain injuries (mTBIs) to be diagnosed, even when existing imaging techniques like MRI don’t show any structural abnormalities. The technique involves loading gadolinium, a standard MRI contrast agent, into hydrogel-based micropatches that are attached to immune cells called macrophages. mTBIs cause inflammation in the brain, which produces signals that attract macrophages to migrate there. Coupling the gadolinium contrast agent to these cells enables MRI to reveal brain inflammation in a pig model of mTBI, which, in the future, could increase the number of correctly diagnosed TBI cases and improve patient care. The method is described in a paper published in Science Translational Medicine.
“70-90% of reported TBI cases are categorized as ‘mild,’ yet as many as 90% of mTBI cases go undiagnosed, even though their effects can last for years and they are known to increase the risk of a host of neurological disorders including depression, dementia, and Parkinson’s disease,” said senior author Samir Mitragotri, PhD, in whose lab the research was performed. “Our cell-based imaging approach exploits immune cells’ innate ability to travel into the brain in response to inflammation, enabling us to identify mTBIs that standard MRI imaging would miss.”
Mitragotri is a Core Faculty member of the Wyss Institute at Harvard University and the Hiller Professor of Bioengineering and Hansjörg Wyss Professor of Biologically Inspired Engineering at Harvard’s John A. Paulson School of Engineering and Applied Sciences (SEAS).
Because the effects of mTBI are believed to be caused by “invisible” brain inflammation, members of the Mitragotri lab decided to leverage their experience with immune cells to create a better diagnostic. “Our previous projects have focused on controlling the behavior of immune cells or using them to deliver drugs to a specific tissue. We wanted to exploit another innate ability of immune cells – homing to sites of inflammation in the body – to carry imaging agents into the brain, where they can provide a visible detection signal for mTBI,” said first author Lily Li-Wen Wang, PhD. Wang is a former Research Fellow in the Mitragotri Lab at the Wyss Institute and SEAS who is now a scientist at Landmark Bio.
The team planned to use their cellular backpack technology to attach gadolinium molecules to macrophages, a type of white blood cell that is known to infiltrate the brain in response to inflammation. But right away, they ran into a problem: in order to function as a contrast agent for MRI scans, gadolinium needs to interact with water. Their original backpack microparticles are compost of a polymer called PLGA, which is hydrophobic (meaning it repels water). So Wang and her co-authors started developing a new backpack made out of a hydrogel material that could be manufactured at a large scale in the lab.
After years of hard work, they finally created a new hydrogel backpack that could produce a strong gadolinium-mediated MRI signal, attach stably to both mouse and pig macrophages, and maintain their cargo for a sustained period of time in vitro. They named their new microparticles M-GLAMs, short for “macrophage-hitchhiking Gd(III)-Loaded Anisotropic Micropatches.” Now, it was time to test them in a more realistic setting, for which they partnered with researchers and clinicians at Boston Children’s Hospital.
First, they injected mouse M-GLAMs macrophages into mice to see if they could visualize them in vivo. They were especially interested to see if they accumulated in the kidney, as existing gadolinium-based contrast agents like Gadavist can cause health risks for patients with kidney disease. Their M-GLAMs did not accumulate in the mice’s kidneys, but persisted in their bodies for over 24 hours with no negative side effects. In contrast, mice injected with Gadavist® showed substantial accumulation of the contrast agent in their kidneys within 15 minutes of injection, and the substance was fully cleared from their bodies within 24 hours.
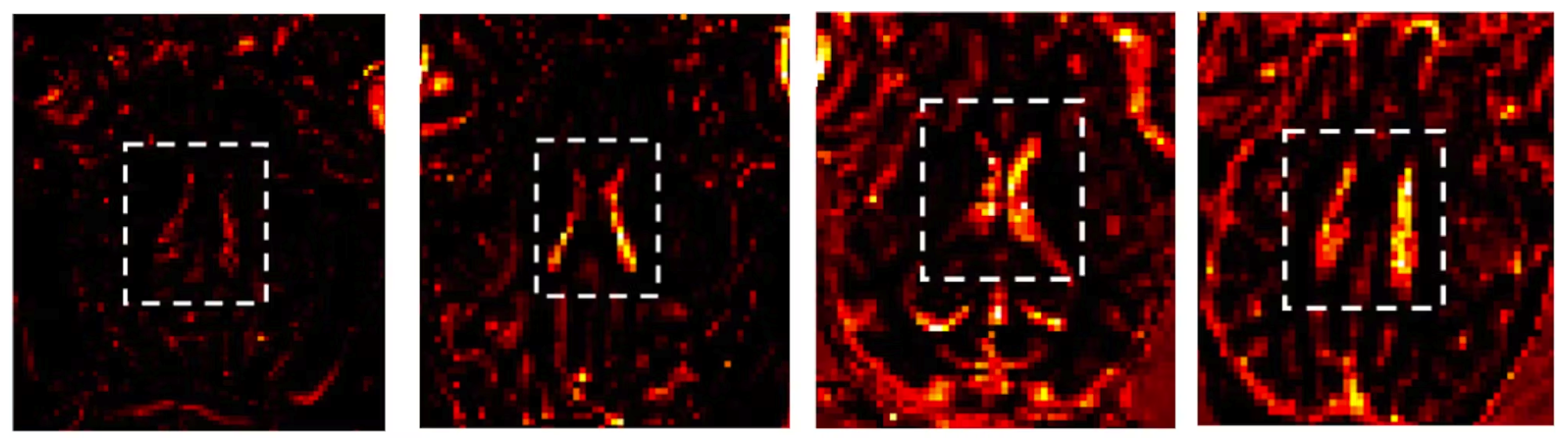
Then, they tested porcine M-GLAMs in a pig model of mTBI. They injected the M-GLAMs into the animals’ blood two days after a mock mTBI, then used MRI to evaluate the concentration of gadolinium in the brain. They focused on a small region called the choroid plexus, which is known as a major conduit of immune cells into the brain. Pigs that received the M-GLAMs displayed a significant increase in the intensity of gadolinium present in the choroid plexus, while those injected with Gadavist did not, despite confirmation of increased inflammation macrophage density in the brains of both groups. The animals showed no toxicity in any of their major organs following administration of the treatments.
“Another important aspect of our M-GLAMs is that we are able to achieve better imaging at a much lower dose of gadolinium than current contrast agents – 500-1000-fold lower in the case of Gadavist®,” said Wang. “This could allow the use of MRI for patients who are currently unable to tolerate existing contrast agents, including those who have existing kidney problems.”
The authors note that while M-GLAMs can indicate the presence of inflammation in the brain via the high concentration of macrophages entering it through the choroid plexus, their technique cannot pinpoint the exact location of injuries or inflammatory responses in brain tissue. However, if coupled with new treatment modalities like one they developed in another recently published paper, M-GLAMS could offer a more rapid and effective way to identify and reduce inflammation in mTBI patients to minimize damage and speed their recovery.
The researchers have submitted a patent application for their technology, and hope to be able to bring it to the market in the near future. They are currently exploring collaborations with biotech and pharmaceutical companies to accelerate it to clinical trials.
“This work demonstrates just how much potential is waiting to be unlocked within the human body for a variety of functions: monitoring health, diagnosing problems, treating diseases, and preventing their recurrence. I’m impressed with this team’s ingenuity in leveraging immune cells to improve medical imaging, and hope to see it in clinicians’ hands soon,” said Wyss Founding Director Donald Ingber, MD, PhD Ingber is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital, and the Hansjörg Wyss Professor of Bioinspired Engineering at SEAS.