Recurrent Respiratory Papillomatosis
Case Summary
An adolescent with a history of recurrent respiratory papillomatosis (RRP) and pulmonary involvement presented with progressive dyspnea on exertion.
Imaging Findings
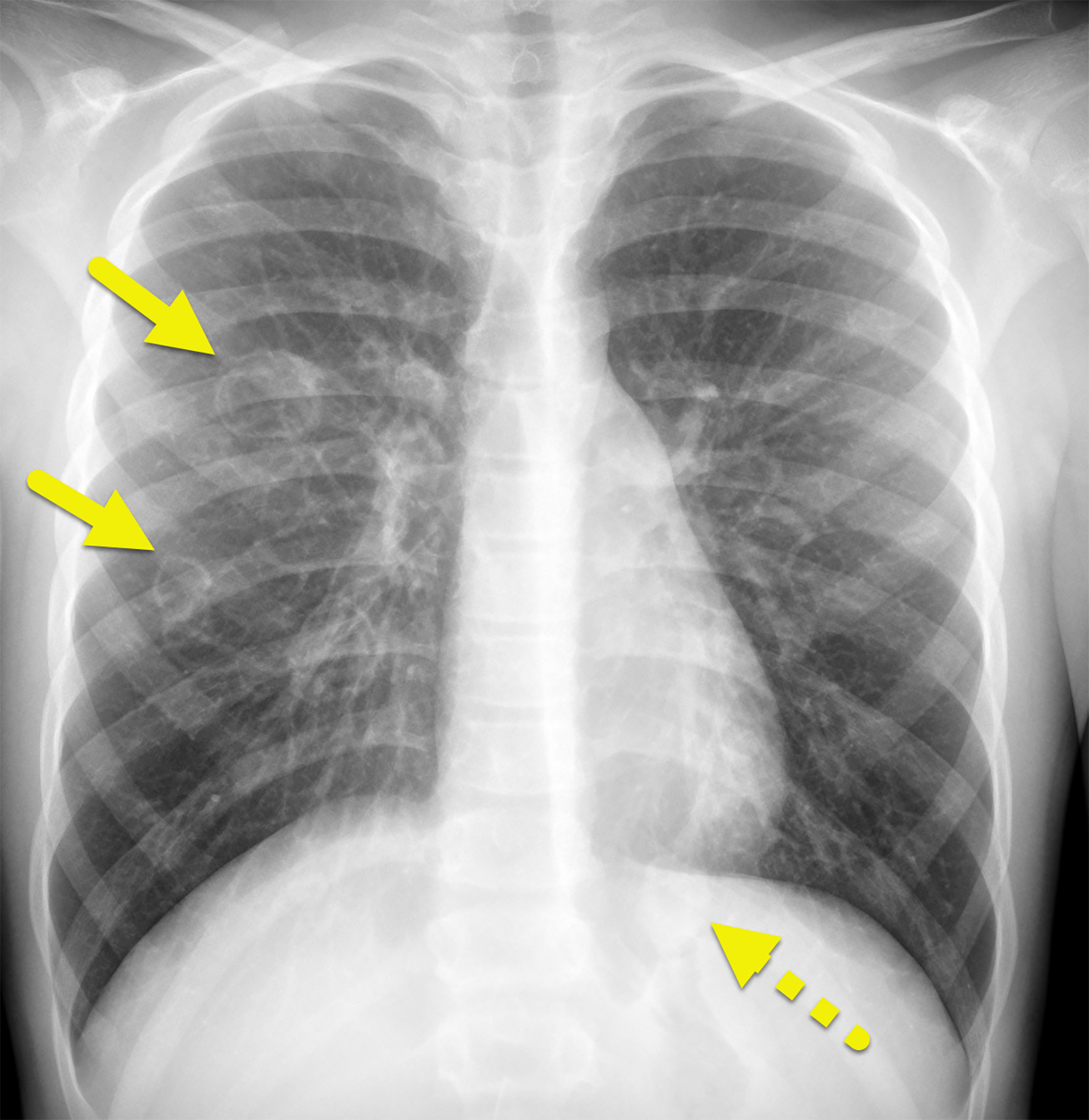
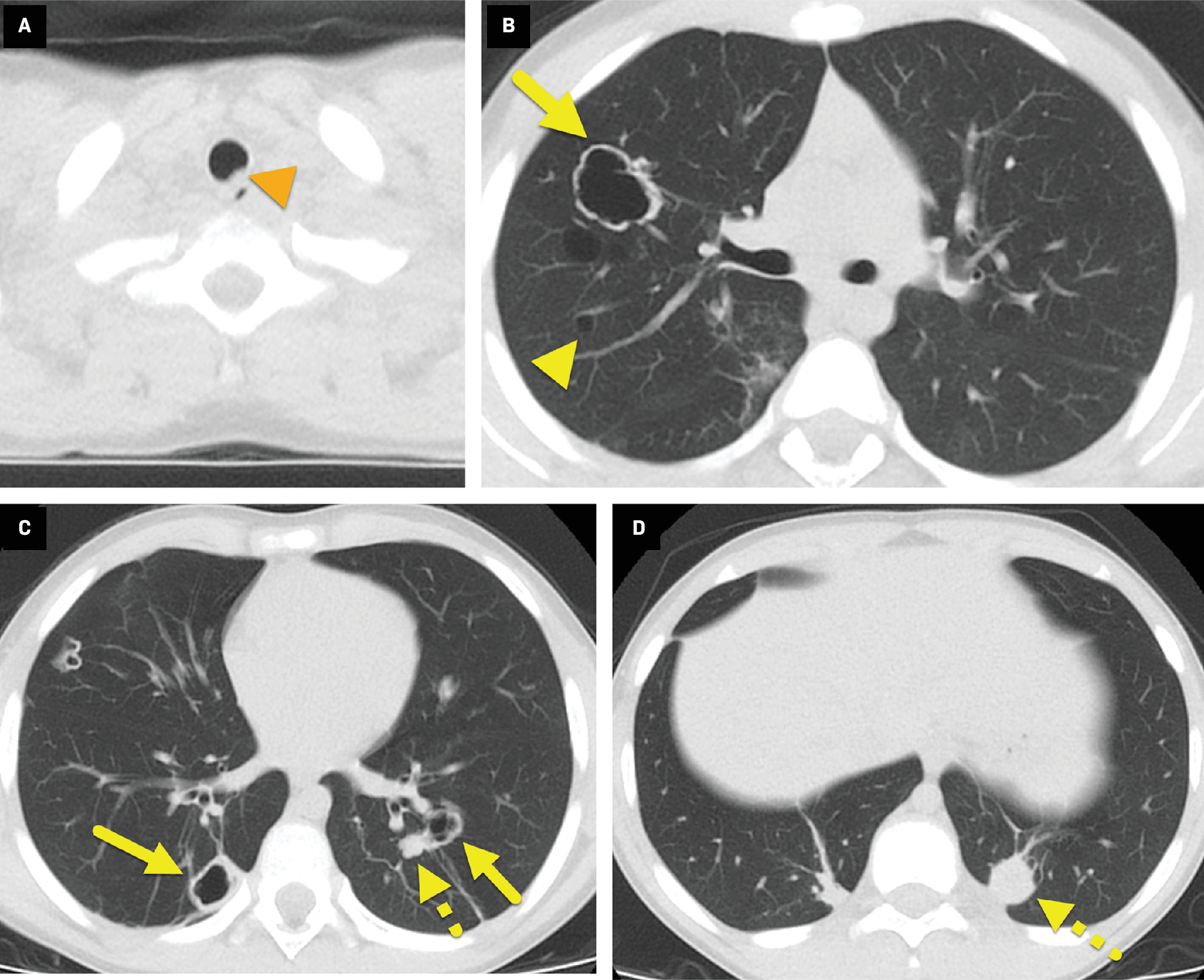
Chest radiograph ( Figure 1 ) and chest CT ( Figure 2 ) showed both cystic and solid lesions. The cystic lesions had a variable appearance: Some had a thick, irregular wall while others had a thin, nearly imperceptible wall. A small nodule was visible in the posterolateral trachea on CT.
Chest radiograph shows multiple cystic (solid arrows) and solid (dashed arrow) lesions in the lungs.
Chest CT through the trachea (A), subcarinal region (B), pulmonary vein insertion (C), and lung bases (D) shows multiple lesions in the airways. Some cystic lesions have a thick, irregular wall (arrows) while others have a barely perceptible wall (yellow arrowhead). Solid pulmonary nodules are also present (dashed arrows). A papilloma (orange arrowhead) is visible along the left posterolateral aspect of the trachea.
Diagnosis
Recurrent respiratory papillomatosis
Discussion
Recurrent respiratory papillomatosis is a rare disease characterized by recurrent benign papillomas that can occur anywhere along the respiratory tract, most commonly the larynx and vocal cords. Globally, the incidence of RRP is 4 per 100,000 children and 2 per 100,000 adults.1 Rates in the US have been steadily declining since the introduction of the human papillomavirus (HPV) vaccine in 2006.2 The current estimated incidence of RRP in children is 4 per 100,000 children and 2 per 100,000 in adults annually.3
Specific types of HPV, most commonly HPV 6 and HPV 11, are associated with the wart-like papilloma characteristic of RRP.3 HPV 11 is associated with more aggressive disease, often seen in children less than 5 years old.4
Recurrent respiratory papillomatosis has a trimodal age distribution, with age peaks at 7, 35, and 64 years,3 and is classified as juvenile- or adult-onset. Patients with juvenile-onset RRP present between 2 and 6 years old with more aggressive disease5 transmitted vertically either in utero or during passage through an infected birth canal. The etiology of adult-onset RRP is unclear, with some sources favoring transmition via oral-genital contact while others favor genetic susceptibility, including adult activation of vertically transmitted disease.6, 7, 8 Upon infection, the virus remains latent within the host cells, causing recurrences even after the elimination of the initial papilloma.
Papillomas are found primarily in the larynx, although they can occur anywhere in the airway, from the nasopharynx to the tracheobronchial tree and pulmonary parenchyma. Clinical presentation is nonspecific and dependent on the location of the lesions. Potential signs include voice changes, cough, dyspnea, wheezing, and stridor. In adults, hoarseness is the most common presenting sign. In children, presenting signs include progressive hoarseness, stridor, and breathing difficulties.5 Owing to the nonspecific signs, children are often treated for pharyngitis, asthma, or bronchitis, resulting in delayed diagnosis and potential for progression to respiratory distress.
Disease course is highly variable, ranging from spontaneous remission to malignant transformation. Squamous cell carcinoma resulting from RRP is rare but has a poor prognosis. Malignant transformation is more commonly associated with HPV 16 and 18, smoking, and radiation therapy.9 Disease recurrence is associated with diminished lymphocyte response, although it remains unclear whether this is causative or a result of infection.10
Recurrent respiratory papillomatosis is rarely diagnosed via chest radiograph, although it can be visualized as solid or cavitated pulmonary nodules if there is lung involvement. In severe cases, chest radiograph may demonstrate symptoms of bronchial obstruction such as atelectasis and bronchiectasis.4
CT is the preferred imaging modality and can demonstrate the tracheal and bronchial lesions characteristic of RRP. Nodular lesions can present on CT as focal or diffuse large airway narrowing. Lung lesions may be single or multiple, nodular or polypoid, and of varying size and distribution.4 In some cases, lesions can present as enlarged air-filled cysts, and superimposed infection can cause air-fluid levels. CT findings of airway obstruction include atelectasis and bronchiectasis.11
Diagnosis is confirmed via laryngoscopy and bronchoscopy, allowing direct visualization of the vocal cords and airways, as well as biopsy for histopathological examination. Papillomas are often visualized as pale polypoid lesions along the respiratory tract. Definitive diagnosis is made via histopathological examination, which shows well-differentiated squamous epithelium with a central fibrovascular core.12
Currently there is no cure for RPP. Papillomas are primarily treated surgically, with adjunct therapy recommended in approximately 20% of patients.4 Clinical criteria for adjunct therapy include greater than 4 surgical procedures per year, rapid regrowth with airway obstruction, or distal multisite spread.13 Adjunct therapy includes antiviral medications, COX-2 inhibitors, and chemotherapeutics.
Conclusion
Recurrent respiratory papillomatosis is a rare disorder of benign neoplasms of the respiratory tract, commonly located along the larynx and vocal cords. It is most commonly associated with HPV 6 and HPV 11 infection, and has a trimodal age distribution, with more aggressive disease in children. If left untreated, RRP can lead to significant respiratory distress and may lead to the development of squamous cell carcinoma. Although there is no cure, surgical excision improves symptoms. The HPV vaccine has helped decrease the incidence of RRP.
References
Citation
Koujah D, Towbin RB, Schaefer CM, Towbin AJ. Recurrent Respiratory Papillomatosis. Appl Radiol. 2024; (5):7 - 9.
doi:10.37549/AR-D-24-0019
October 1, 2024