Radiological Case: Intra-abdominal desmoid tumor
Images
CASE SUMMARY
A 72-year-old asymptomatic man, with a remote history of a gastrointestinal stromal tumor previously treated with Gleevec, complained of lower abdominal discomfort and bowel changes. A large mass was palpable on abdominal examination. Given the patient’s history, the possibility of GIST recurrence was considered, and a positron emission tomography/computed tomography (PET/CT) was performed. A biopsy of the pelvic mass was performed; microscopic pathologic examination demonstrated fibroblastic proliferation and collagen without evidence of mitosis or necrosis. Immunohistochemical stains showed the tumor cells to be focally positive for smooth muscle actin and negative for markers for epithelium. Cytomorphological features were suggestive of desmoid/fibromatosis tumor.
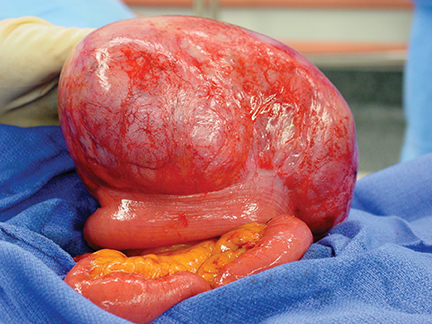
At laparotomy, the mass was smooth, glistening, and mobile, intimately attached to one loop of small bowel. The mass was excised with an en bloc small-bowel resection with wide margins of the mesentery (Figure 1). Upon gross and microscopic pathologic examination, the tumor was characterized as an abdominal fibromatosis (desmoid) involving the small bowel serosa and muscularis propria. There was no evidence of malignancy. Eleven adjacent lymph nodes were negative for tumor.
IMAGING FINDINGS
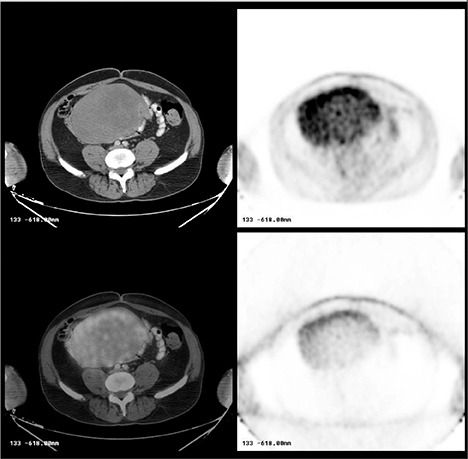
A CT scan revealed an elliptical mass in the mid-pelvis measuring 10.6 × 16 × 16 cm and exhibiting smooth margins. It was inseparable from adjacent loops of small bowel. There was no small-bowel dilatation or wall thickening. Minimal dilatation of the renal collecting systems and perinephric stranding stemming from external compression was seen bilaterally. The PET portion of the study demonstrated heterogeneous hypermetabolic activity within the pelvic mass. The mean standard uptake values (SUV) of this activity ranged from 2.2 to 3.4(Figure 2).
DIAGNOSIS
Intra-abdominal desmoid tumor (fibromatosis)
DISCUSSION
Desmoid tumors are rare and are most often located abdominally or intra-abdominally.1 They may also be found in the retroperitoneum,thorax, shoulder girdle, buttocks, and limbs. They are the most common primary mesenteric tumors.2 Women are more commonly affected than men by a 3:1 ratio.3 Approximately two-thirds of patients are between the ages of 20 and 40. Up to 75% of these tumors occur inpatients with a history of previous abdominal surgery.4 Other associated conditions include familial polyposis syndrome, Gardner’s syndrome,1 estrogen therapy and trauma.2 Desmoid tumors are multiple in 10% to 15% of cases.5
Though desmoid tumors rarely cause symptoms, large desmoids may cause symptoms by compression of adjacent structures or systems.A palpable mass is often present. Potential complications include gastrointestinal bleeding, small-bowel obstruction, and hydronephrosis,which was observed in our patient’s case.
Surgical excision with wide, pathologically-confirmed negative margins is generally the treatment of choice.6 Recurrence rates after surgical resection range from 39% to 79%,6 but is generally confined to the more aggressive lesions. Grossly, desmoid tumors are typically well-circumscribed, but may have irregular or infiltrating borders. They are dense and rubbery in consistency and do not have a definable capsule. On cut surface, the tumors are grayish-white in color and resemble scar tissue. Usually > 5 cm at the time of diagnosis, they may achieve sizes in excess of 15 cm.5
Histologically, desmoid tumors consist of spindle-shaped cells arranged in broad bundles within an abundant collagenous matrix. Infiltration of surrounding normal structures is usually demonstrated. There may be more cellularity peripherally compared to the central portions. Desmoids do not exhibit the cytologic features of malignancy. They are well-differentiated and lack increased mitotic figures and atypical, pleomorphic or hyperchromatic nuclei.7 Therefore, while these tumors are locally aggressive, metastases are rare.8
Desmoid tumors have been characterized extensively on multiple imaging modalities. Typical appearance of the abdominal desmoid tumor on CT is that of a well-circumscribed, solid, soft-tissue mass without calcification. On MRI, desmoids demonstrates low-signal intensity on T1-weighted images and variable T2-weighted images relative to muscle, owing to the fibrous nature of the tumor.9 At sonography, desmoids exhibit variable echogenicity, with smooth, well-defined margins.9 Usually, angiographic features are nonspecific. The lesion may appear as a soft-tissue mass with heterogeneous uptake of contrast, increased vascularity, and large arteries around its periphery or as arteriovenous shunting.10
CONCLUSION
Desmoid tumors are rare, solid tumors that may occur in various sites. Despite their low metastatic potential, abdominal desmoids may demonstrate hypermetabolic activity on FDG-PET, as this case demonstrates.
REFERENCES
- Einstein DM, Tagliabue, JR, Desai RK. Abdominal desmoids: CT findings in 25 patients. AJR. 1991;157:275-279.
- Burke AP, Sobin LH, Skekitha KM, Federspiel BH, Helwig EB. Intra-abdominal: A pathologic analysis of 130 tumors with comparison of clinical subgroups. Am J Surg Pathol. 1990;14:335-341.
- Stephens D., ed. Gastrointestinal Disease (Fourth Series) Test and Syllabus. Reston, Va.: The American College of Radiology; 1990.
- Brooks AP, Reznek RH, Nugent K, Farmer KC, Thomson JP, Phillips RK. CT appearances of desmoid tumors in familial adenomatous polyposis: Further observations. Clin Radiol. 1994; 49:601-607.
- Kempson RL, Fletcher CDM, Evans HL, Hendrickson MR, Sibley RK. Extra-abdominal fibromatosis (extra-abdominal desmoid fibromatosis). Atlas of tumor pathology. Tumors of the soft tissues. Washington, DC: Armed Forces Institute of Pathology, 2001:71-87.
- Ballo MT, Zagars GK, Pollack A, Pisters PW, Pollack RA. Desmoid tumor: Prognostic factors and outcome after surgery, radiation therapy, or combined surgery and radiation therapy. J Clin Oncol. 1999;17:158-167.
- Anthony T, Rodriguez-Bigas MA, Weber TK, Petrelli NJ. Desmoid tumors: Collective review. 1996;182:369-376.
- Lewis JJ, Boland BJ, Leung DH, Woodruff JM, Brennan MF. The enigma of desmoid tumors. Ann Surg. 1999;229: 866-873.
- Casillas J, Sais GJ, Greve JL, Ipparraguirre, Morillo G. Imaging of intra- and extra-abdominal desmoid tumors. Radiographics. 1991;11:959-968.
- Tottermann S, Reitamo JJ. Desmoid tumor: An angiographic study of five cases. Br J Radiol. 1979; 52:936-94.