Radiological Case: Hepatic infarction
Images




CASE SUMMARY
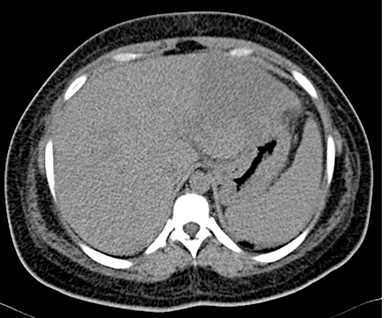
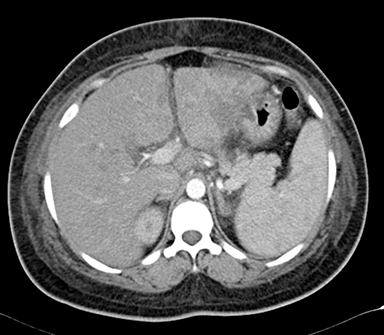
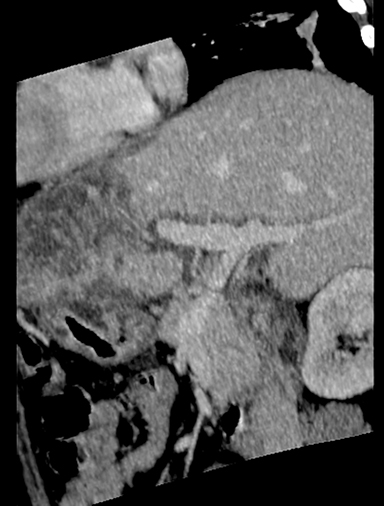
A 26-year-old woman, third gravida (G3P1L0A2), with a history of recurrent fetal loss, presented with complaints of epigastric pain, nausea and vomiting. Laboratory investigation revealed thrombocytopenia (41,000/cumm), raised SGPT (140 IU/L), SGOT (224 IU/L) and S.ALP (113 IU/L). Prothrombin time was normal. S.APLA and S.ANA were negative. Infectious screen was negative. USG abdomen was suggestive of mild hepatosplenomegaly with an ill-defined inhomogenous echo pattern in the left lobe of liver, small-volume ascites and right pleural effusion (Figure 1). USG obstetric scan revealed intrauterine fetal demise. Delivery, induced with prostaglandin E2, was uneventful and the patient was discharged with stable vital signs. The patient was readmitted 3 days post-discharge with abdominal pain and fever. Blood investigations showed leucocytosis and thrombocytopenia. A contrast-enhanced CT scan of the abdomen and pelvis was done with provisional clinical diagnosis of hepatic abscess. The scan revealed mild to moderate ascites with mild bilateral pleural effusion with passive atelectasis of underlying lung parenchyma (Figures 2-6). Follow-up ultrasound abdomen was performed after 6 months, showing normal hepatic parenchymal echotexture (Figure 7). The patient was advised to get her protein C, protein S and antithrombin III levels checked.
IMAGING FINDINGS
The MDCT abdominal scan revealed mild hepatomegaly with multiple round, central and irregular, wedge-shaped peripheral hypodense areas in segments II, III, IV B, V and VIII of liver. There was poor opacification of segmental branches of left portal vein in segment II and III. Mild to moderate ascites with mild bilateral pleural effusion with passive atelectasis of underlying lung parenchyma (Figures 2-6).
DIAGNOSIS
Hepatic infarction
DISCUSSION
Hepatic infarction is defined as areas of coagulative necrosis from hepatocyte cell death caused by local ischemia which, in turn, results from the obstruction of circulation to the affected area, most commonly by a thrombus or embolus.
Hepatic infarction is uncommon due to the dual blood supply from the hepatic artery and portal vein as well as extensive collateral vessels. It may be iatrogenic, post-traumatic, post-liver transplant, secondary to hypercoagulability, vasculitis or infection. Hepatic infarcts appear as peripheral, wedge-shaped, rounded or irregularly shaped tubular areas of low attenuation paralleling bile ducts on unenhanced CT scans. On contrast-enhanced scans, they appear as perfusion defects and are distributed in geographical or segmental pattern with patchy and heterogenous enhancement due to undisplaced vessels in infarcted areas.1
CT is the method of choice in diagnosing hepatic infarction, providing useful information regarding site, morphology and extent of the lesion. Further, it is able to suggest the possible etiology and guide appropriate management.2 On ultrasound, geographic areas of decreased echogenicity with preservation of portal tracts are early signs of hepatic ischemia and may resolve completely or progress to true infarction. Calcification may also occur quite rapidly. Biliary strictures, bilomas and abscess formation are later complications.3
Hepatic infarcts can occur at all stages of pregnancy from the 7th week to postpartum. Hepatic infarcts in pregnancy are mostly secondary to APS (Anti-Phospholipid Syndrome), HELLP syndrome (hemolysis, elevated liver enzymes, low platelets) and preeclampsia. Both hepatic arteries and portal veins may be involved in APS. Arterial thromboses of both large and small hepatic arteries are seen.
CONCLUSION
Intrahepatic haemorrhages/infarctions develop in pre-eclampsia/HELLP syndrome, typically in the late third trimester or postpartum interval in 1 per 45,000-2 per 25,000 pregnancies with a maternal mortality of 50% . Associated factors include multiparity, advanced maternal age, simultaneous pre-eclampsia and Anti-Phospholipid Syndrome. Signs and symptoms appear before significant laboratory changes appear. Hepatic rupture and shock can occur rarely within 48 hours of symptom onset.4
The differential diagnoses of intra hepatic infarction include intrahepatic abscess, acute fatty liver of pregnancy, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, ruptured hepatic adenoma, hepatocellular carcinoma and hemangioma.
Preservation of portal tracts helps in differentiating infarction from other causes of hypo-attenuating lesions in the liver. Laboratory findings include anemia, thrombocytopenia, leucocytosis, marked aminotransferase elevation and azotemia. Changes are typically found in right lobe. Treatment includes urgent delivery. Patients with infarct can be managed conservatively and transfused. They are at risk of intrahepatic infection.
REFERENCES
- Torabi M, Hosseinzadeah K, Federle M. MDCT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics. 2008;28:1967-1982.
- Giovine S1, Pinto A, Crispano S, Lassandro F, Romano L. Retrospective study of 23 cases of hepatic infarction: CT findings and pathological correlation. Radiol Med. 2006;111(1):11-21.
- Cook GJ, Crofton ME. Hepatic artery thrombosis and infarction: Evolution of the ultrasound appearances in liver transplant recipients. Br J Radiol. 1997 Mar;70:248-251.
- Joshi D, James A, et al. Liver disease in pregnancy. Lancet. 2010;375: 594-605.
Citation
. Radiological Case: Hepatic infarction. Appl Radiol.
February 12, 2015