Pulmonary Sarcomatoid Carcinoma
Images

Case Summary
An elderly patient with a history of smoking presented with shortness of breath, fatigue, generalized weakness, and unintentional weight loss. The physical exam revealed a palpable right flank mass but was otherwise unremarkable. The laboratory workup demonstrated an elevated white blood cell count of 48,000 but was otherwise normal. A chest radiograph appeared abnormal, prompting computed tomography (CT) imaging of the chest.
Imaging Findings
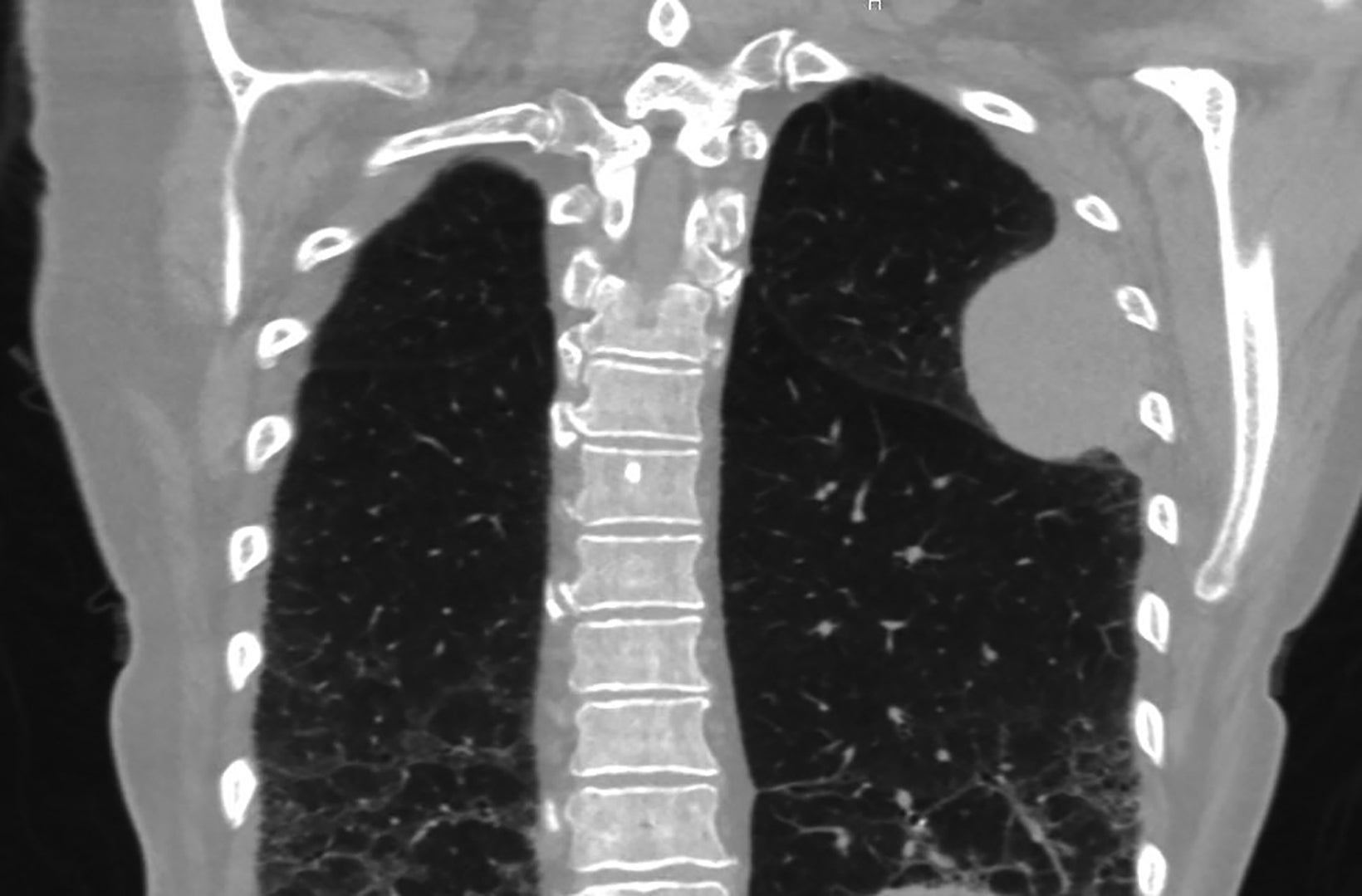
Initial CT chest revealed a left upper lobe mass measuring up to 6.3 cm, abutting the pleural surface and invading the thoracic wall involving the left fourth rib (Figure 1). Additional findings included chronic interstitial and emphysematous changes and mediastinal lymphadenopathy.
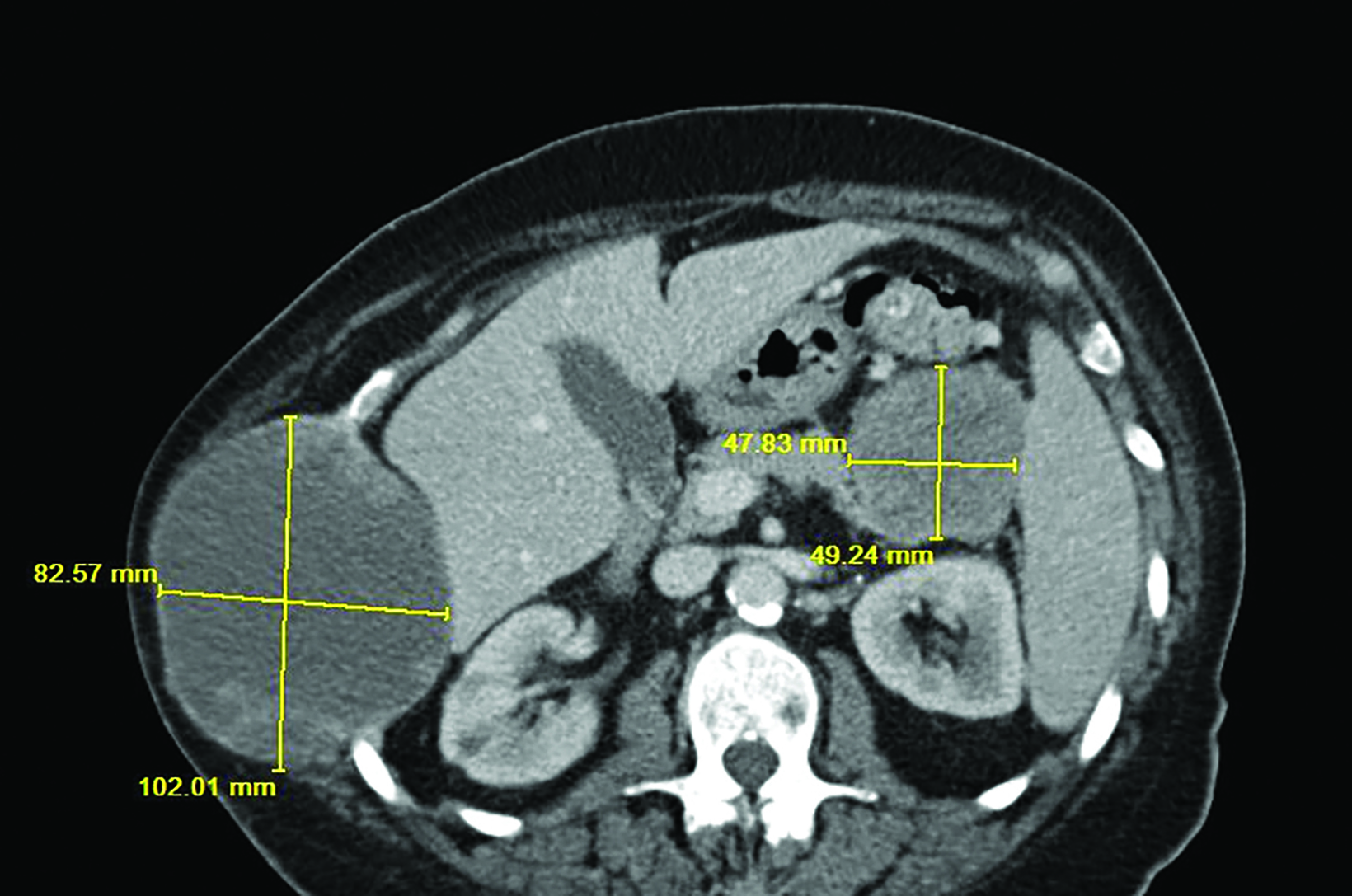
Contrast-enhanced CT of the abdomen and pelvis then demonstrated a heterogeneous, centrally necrotic, expansile mass involving the lateral aspect of the right tenth rib with invasion into the adjacent soft tissue and mass effect on the liver, measuring up to 10.2 cm (Figures 2,3). Additionally, a third centrally necrotic mass measuring up to 5.4 cm was seen arising from the tail of the pancreas (Figure 3).
The patient was referred to interventional radiology, where a CT-guided core biopsy of the right abdominal wall mass was performed.
Diagnosis
Pulmonary sarcomatoid carcinoma
Discussion
Pulmonary sarcomatoid carcinoma (PSC) is a rare form of non-small cell lung cancer (NSCLC) that accounts for 0.4% of all lung cancers1 and has an especially poor prognosis compared with other NSCLCs. One study reported a median survival of 34 months for localized disease and 3 months for distant disease.1 Another study reported a median time to recurrence of 11.3 months.2 The rarity and rapid progression of PSC makes it difficult to study. This case highlights the aggressiveness of PSC and one of the various ways it can present.
Patients with PSC are more commonly male, smokers, and typically in their 60s at diagnosis. Signs and symptoms are nonspecific and depend on tumor location.3 This patient had relatively few pulmonary symptoms for such a large lesion.
PSC usually appears as a large, round, or bosselated tumor that is necrotic and hemorrhagic. It invades surrounding structures, including the thoracic wall.3 One study reported that PSC most commonly presents peripherally in the upper lobes, with most cases being diagnosed at an advanced stage.4 PSC demonstrates both hematologic and lymphatic spread.3 Metastases have been reported in the typical locations to
which NSCLCs metastasize: brain, bone, liver, and adrenal glands. However, metastasis to the esophagus, jejunum, rectum, heart, kidney, and pancreas has also been reported.3 Because metastasis to the contralateral abdominal wall was proven in this patient, the pancreatic mass was presumed to be a metastasis, giving this case two unique metastatic locations.
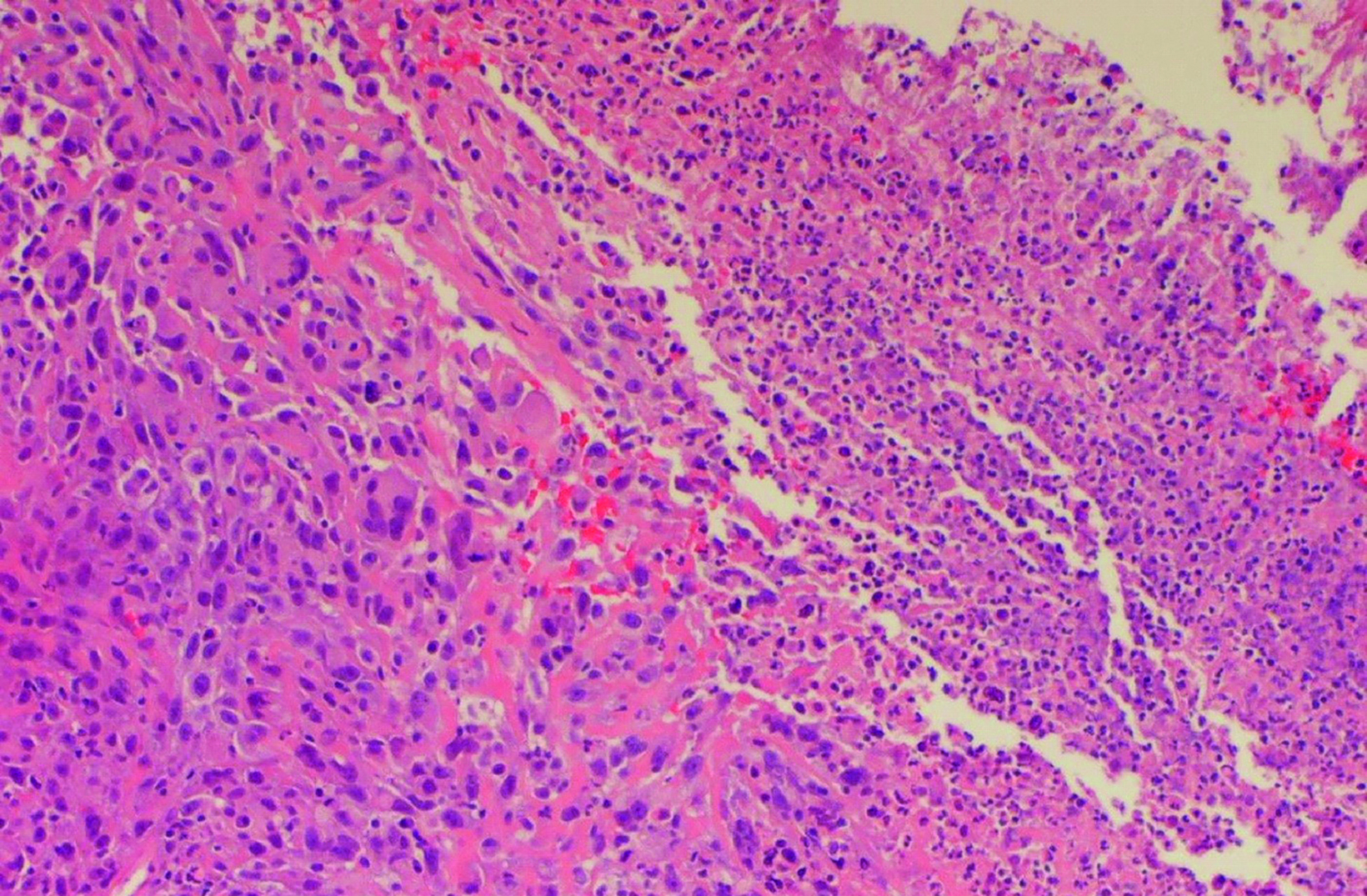
PSC contains both a poorly differentiated NSCLC component (adenocarcinoma, squamous cell carcinoma) and mesenchymal component (malignant spindle or giant cells).3 To be classified as PSC the mesenchymal component must be at least 10% based on WHO criteria. The tumor is categorized according to five subtypes based on its elements: pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and pulmonary blastoma.5
Pathology results in this case showed polygonal cells with large, pleomorphic, prominent nucleoli, readily identified mitosis (>20 per hpf), and abundant eosinophilic cytoplasm (Figure 4). The cells were surrounded by dense eosinophilic matrix. Abundant neutrophils were present, showing extensive necrosis. Given the morphology and corresponding radiologic features with oligometastatic disease, pathological results were classified as poorly differentiated and sarcomatoid lung carcinoma.
The pathogenesis of PSC is being investigated. Epithelial-mesenchymal transition (EMT) is the proposed mechanism.6 During EMT, biochemical changes occur in an epithelial cell that give it mesenchymal cell characteristics. These characteristics allow it to migrate from its basement membrane, invade, and resist apoptosis.7 This may explain the aggressiveness of PSC. Additional genetic studies on PSC are finding novel genetic mutations, suggesting potential future treatment options.8
Treatment for PSC is limited. In one study, surgery provided the best overall survival, while systemic chemotherapy alone provided no improvement in overall survival.5 Another study, however, showed partial response and improvement in overall survival with platinum-based chemotherapy.9 Additional treatment options such as EGFR-targeted therapies are being explored.10
Conclusion
PSC is a rare lung cancer with a very poor prognosis and low prevalence that makes it difficult to study. Early recognition, prompt biopsy, and awareness of the aggressiveness of PSC play an integral role in diagnosis and patient prognosis.
References
- Yendamuri S, Caty L, Pine M, et al. Outcomes of sarcomatoid carcinoma of the lung: a surveillance, epidemiology, and end results database analysis. Surgery. 2012;152(3):397-402.
- Martin, LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007 Sep;84(3):973-980.
- Pelosi G, Sonzongni A, De Pas T, et al. Pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol.2010 Apr;18(2):103-120. https://journals.sagepub.com/doi/ abs/10.1177/1066896908330049. Accessed July 18, 2019.
- Sim JK, Chung SM, Choi JH, et al. Clinical and molecular characteristics of pulmonary sarcomatoid carcinoma. Korean J Intern Med.2018;33(4):737-744. https://doi. org/10.3904/kjim.2017.245. Accessed July 15 2019.
- Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10(9):1243-1260.
- Karim NA, Schuster J, Eldessouki I, et al. Pulmonary sarcomatoid carcinoma: University of Cincinnati experience. Oncotarget. 2017;9(3): 4102–4108. https://doi.org/10.18632/ oncotarget.23468. Accessed July 16, 2019.
- Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119(6):1420-1428.
- Liu X, Jia Y, Stoopler MB, et al. Next-generation sequencing of pulmonary sarcomatoid carcinoma reveals high frequency of actionable MET gene mutations. J Clin Oncol. 2016;34(8):794-802. https://ascopubs.org/doi/full/10.1200/JCO.2015.62.0674. Accessed July 16, 2019.
- Vieira T, Girard N, Ung M, et al. Efficacy of first-line chemotherapy in patients with advanced lung sarcomatoid carcinoma. J Thorac Oncol. 2013;8:1574-1577.
- Italiano, A, Cortot AB, Ilie M, et al. EGFR and KRAS status of primary sarcomatoid carcinomas of the lung: implications for anti-EGFR treatment of a rare lung malignancy. Int J Cancer. 2009;125(10):2479-2482.
References
Citation
F G, H S, N M, J P, L R, A P, A K, M J,. Pulmonary Sarcomatoid Carcinoma. Appl Radiol. 2022;(2):48A-48C.
March 4, 2022