PRRT Most Effective Option for Treating Metastatic Neuroendocrine Tumors
Images
Peptide receptor radionuclide therapy (PRRT) is the most effective and least toxic among treatments for metastatic neuroendocrine tumors, according to new research published in the September issue of The Journal of Nuclear Medicine. Compared to treatment with everolimus, PRRT offered a higher objective response rate and longer progression-free survival, making it ideal for frail populations or when an objective response is needed.
Metastatic neuroendocrine tumors are most common in the small intestine and in the pancreas but can also occur in the lungs. With treatment, the overall survival rate after five years is higher than or close to 50%. While various treatments are available for metastatic neuroendocrine tumors, including PRRT and everolimus, no studies have been performed to determine which is most effective.
“Real-world data with long-term follow-up reporting information on both PRRT and everolimus is important to improve our knowledge with regard to effectiveness and risks of cumulative toxicities,” said Thomas Walter, MD, PhD, professor in the medical oncology department of Hospices Civils de Lyon and Cancer Research Center of Lyon
(Gastroenterology and Technology for Health) in Lyon, France. “As these two treatments are often both given to patients, it’s also important to understand what therapy is most beneficial to administer first.”
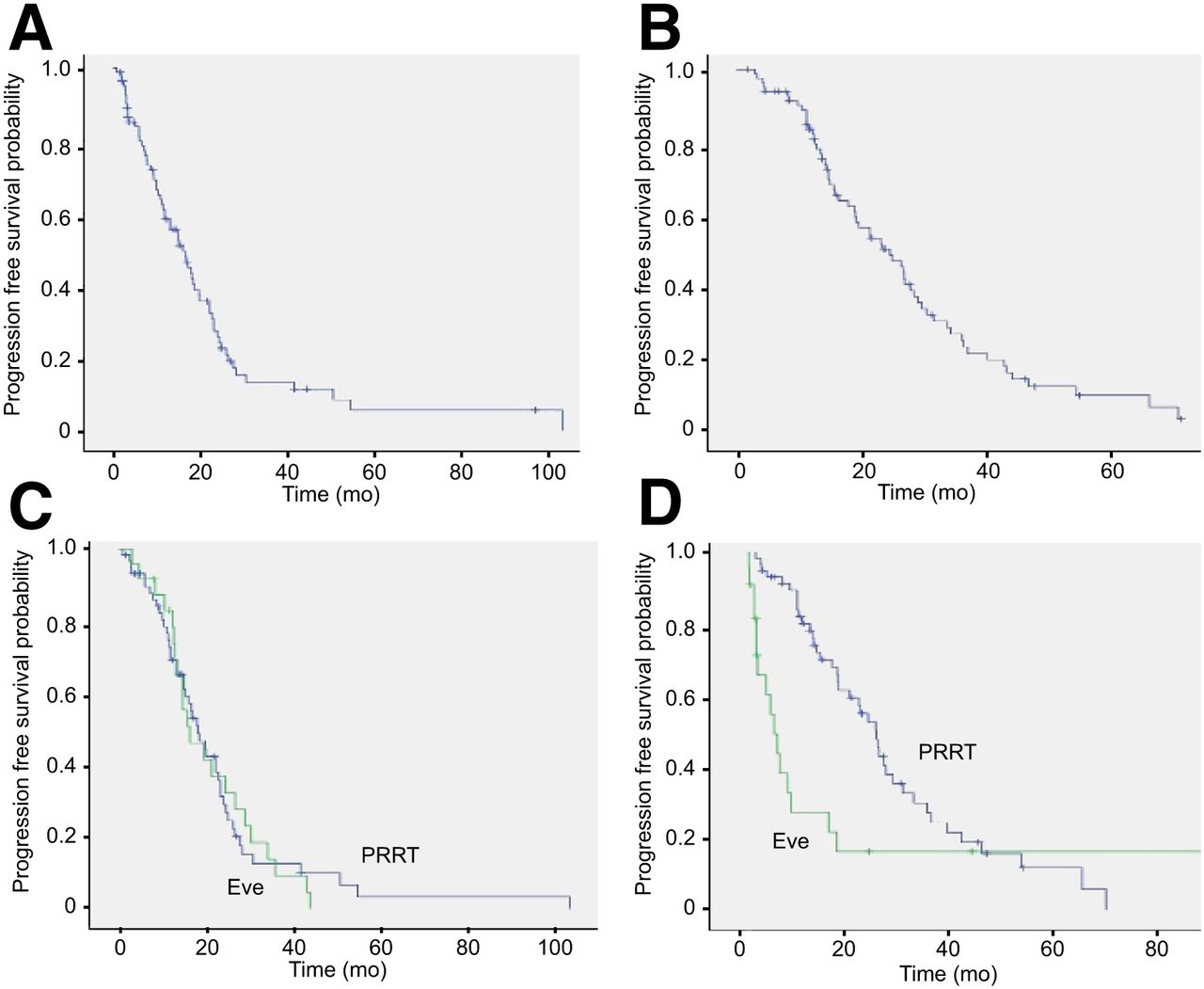
The study sought to compare PRRT and everolimus in terms of efficacy and safety, as well as evaluate the sequences (everolimus followed by PRRT or PRRT followed by everolimus) based on overall progression-free survival. In the retrospective, multicenter study, 84 patients who received both treatments were identified; 60 started with everolimus and 24 started with PRRT. The objective response rate and median progression-free survival were compared, and the safety profile of both treatments were analyzed.
The objective response rate and median progression-free survival was 6% and 16.1 months, respectively, for everolimus and 22.6% and 24.5 months, respectively, for PRRT. Fewer adverse everts were observed with PRRT as compared to everolimus. In addition, the overall progression-free survival was not statistically different whether the patients started their treatment sequence with everolimus or PRRT.
“This study provides information for doctors who need to explain the different therapeutic options to patients with metastatic neuroendocrine tumors,” noted Walter. “The administration of these two treatments is very different, as are their advantages and disadvantages. The choice of the first treatment to be administered must be discussed on a case-by-case basis."