Polyorchidism with intermittent testicular torsion
By Sylvestre D, Brown AS, Conway D


CASE SUMMARY
A 55-year-old man with a history of seizure disorder and depression presented to the emergency department (ED) with scrotal swelling and testicular pain. The patient reported symptoms of incomplete bladder emptying, pain posterior to the scrotum, and pain with bowel movements. He also reported scrotal swelling over the last 3 years. He conveyed suspicion of a scrotal mass. On physical examination, the penis and epididymides were normal with no lesions, discharge, or palpable masses. There was no tenderness on palpation of the perineal region. Gonorrhea/chlamydia testing was negative. Testicular Doppler US of the scrotum and testicles demonstrated polyorchidism with suggestion of subacute/chronic testicular torsion. On re-examination, the patient was clinically stable with improvement of symptoms. He was discharged from the ED and advised to seek urology follow-up care.
IMAGING FINDINGS
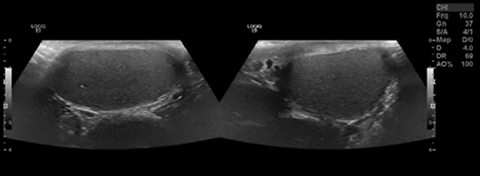
Gray-scale ultrasound of the left hemiscrotum demonstrated a 4.5 x 2.2 x 3.7 cm mass lateral to the left testis with homogenous hypoechogenicity and microcalcifications (Figure 1). Color Doppler ultrasound of the left hemiscrotum demonstrated absent vascular perfusion to the left lateral testicle (Figure 2). Color Doppler US of the right and left testes demonstrated normal vascular flow (Figure 3).
DIAGNOSIS
Polyorchidism with absent vascular flow in the left hemiscrotum suggesting subacute/chronic testicular torsion of the left lateral testicle.
DISCUSSION
This case reveals a rare and potentially first presentation of polyorchidism with subacute/chronic testicular torsion of the left lateral testicle in a male older than 50 years of age. The left and right testicles were normal in echogenicity on US with no apparent mass, cyst, or suspicious calcification. The testicles had normal vascular perfusion on color Doppler US with the additional left lateral testicle demonstrating an absence of vascular flow, leading to the diagnosis of polyorchidism with subacute/chronic torsion.
Polyorchidism is rare, with approximately 140 histologically confirmed cases in the literature.1 The most common presentation is triorchidism with intrascrotal left-sided predominance.1 Triorchidism originates from abnormal division of the genital ridge.1,2 The median age of diagnosis is 17 yo.1 The supernumerary testis is typically identified subsequent to symptomatic presentation of inguinal hernia, maldescended testis, testicular torsion, hydrocele, or varicocele.1,3 The differential diagnosis includes hydrocele, spermatocele, varicocele, Morgagnian cyst, and testicular neoplasm.1
US and MR can be used to support the diagnosis of polyorchidism.1,4 In a meta-analysis, US identified polyorchidism in 81% of confirmed cases.1 In the asymptomatic patient, the supernumerary testis echotexture, MR signal intensity, and vascular flow are similar to normal testes.3,5 MR can be used for confirmation if the US is equivocal.3,4,5 Polyorchidism can be managed conservatively with serial US if there is no evidence of malignancy.5
Testicular torsion is the result of spermatic cord twisting causing decreased perfusion to the testicle.6 Patients with torsion commonly have the anatomic variant of the tunica vaginalis joining high on the spermatic cord.6 Testicular torsion can be classified as acute or intermittent. Acute testicular torsion presents with severe scrotal pain, and it is a surgical emergency due to the risk of rapid testicular necrosis.7 Intermittent testicular torsion presents with recurrent scrotal pain of short duration that resolves spontaneously.8 Both acute and intermittent testicular torsion are less commonly diagnosed in adults.9 Scrotal swelling can be present on examination.8,9 Intermittent testicular torsion can be managed conservatively or with orchidopexy. Orchidopexy is often recommended to prevent testicular necrosis and relieve recurrent testicular pain.9
Imaging plays a key role in the diagnosis of torsion. MR T2-hypointensity indicates testicular torsion and hemorrhagic necrosis.2,10 While the US echogenicity may initially be unremarkable, necrosis later develops and is indicated by a heterogenous and hypoechoic appearance.7 Color Doppler US is frequently used for to evaluate acute scrotum, as it demonstrates reduced or absent perfusion of the affected testicle.2,6,7 However, color Doppler US does not always demonstrate compromised vascular flow in intermittent testicular torsion.8,9
CONCLUSION
Polyorchidism diagnosed in the setting of subacute/chronic testicular torsion is a rare and uncommon presentation. US and color Doppler US are the main imaging modalities used to support the diagnoses of polyorchidism and testicular torsion, respectively.
REFERENCES
- Bergholz R and Wenke K. Polyorchidism: a meta-analysis. Pediatric Urology. 2009;182(5):2422-2427.
- Kumar K, Das D, Shivaraj. Triorchidism with Torsion. Ann Med Health Sci Res. 2012;2(2): 199–201.
- Yalçınkaya S, Şahin C, Feyzullah Şahin A. Polyorchidism: sonographic and magnetic resonance imaging findings. Can Urol Assoc J. 2011;5(5):E84–E86.
- Bhogal R, Palit A, Prasad K. Conservative management of polyorchidism in a young man: a case report and review of literature. Pediatr Surg Int. 2007;23(7):689–691.
- Arslanoglu A, Tuncel SA, Hamarat M. Polyorchidism: color Doppler ultrasonography and magnetic resonance imaging findings. Clin Imaging. 2013;37(1):189-91.
- Aso C, Enríquez G, Fité, M, et al. Gray-scale and color doppler sonography of scrotal disorders in children: an update. Radiographics. 2005;25(5):1197-214.
- Agrawal AM, Tripathi PS, Shankhwar A, Naveen C. Role of Ultrasound with Color Doppler in Acute Scrotum Management. J Family Med Prim Care. 2014;3(4):409–412.
- Eaton SH, Cendron MA, Estrada CR, et al. Intermittent Testicular Torsion: diagnostic features and management outcomes. The Journal of Urology. 2005;174(4Pt2):1532-5.
- Al-Kandari AM, Kehinde EO, Khudair S, et al. Intermittent Testicular Torsion in Adults: An Overlooked Clinical Condition. Med Princ Pract. 2017;26(1):30-34.
- Watanabe Y, Nagayama M, Okumura A, et al. Imaging of testicular torsion: Features of testicular hemorrhagic necrosis and clinical outcomes. J Magn Reson Imaging. 2007;26(1):100–108.
Prepared by Ms. Sylvestre while a third-year Medical Student at Mercer University School of Medicine, Savannah, GA; and Dr. Brown while a PGY-4 Diagnostic Radiology Resident, and Dr. Conway while serving as Assistant Program Director of Diagnostic Radiology, at Memorial Health University Medical Center, Savannah, GA.
