Pleomorphic Adenoma of the Parotid Gland
Images
Case Summary
A teenager with no significant past medical history presented with a firm, non-tender 3 x 4 cm subcutaneous mass in the left upper neck. On physical exam there were no overlying changes to the skin, drainage, or erythema.
Imaging Findings
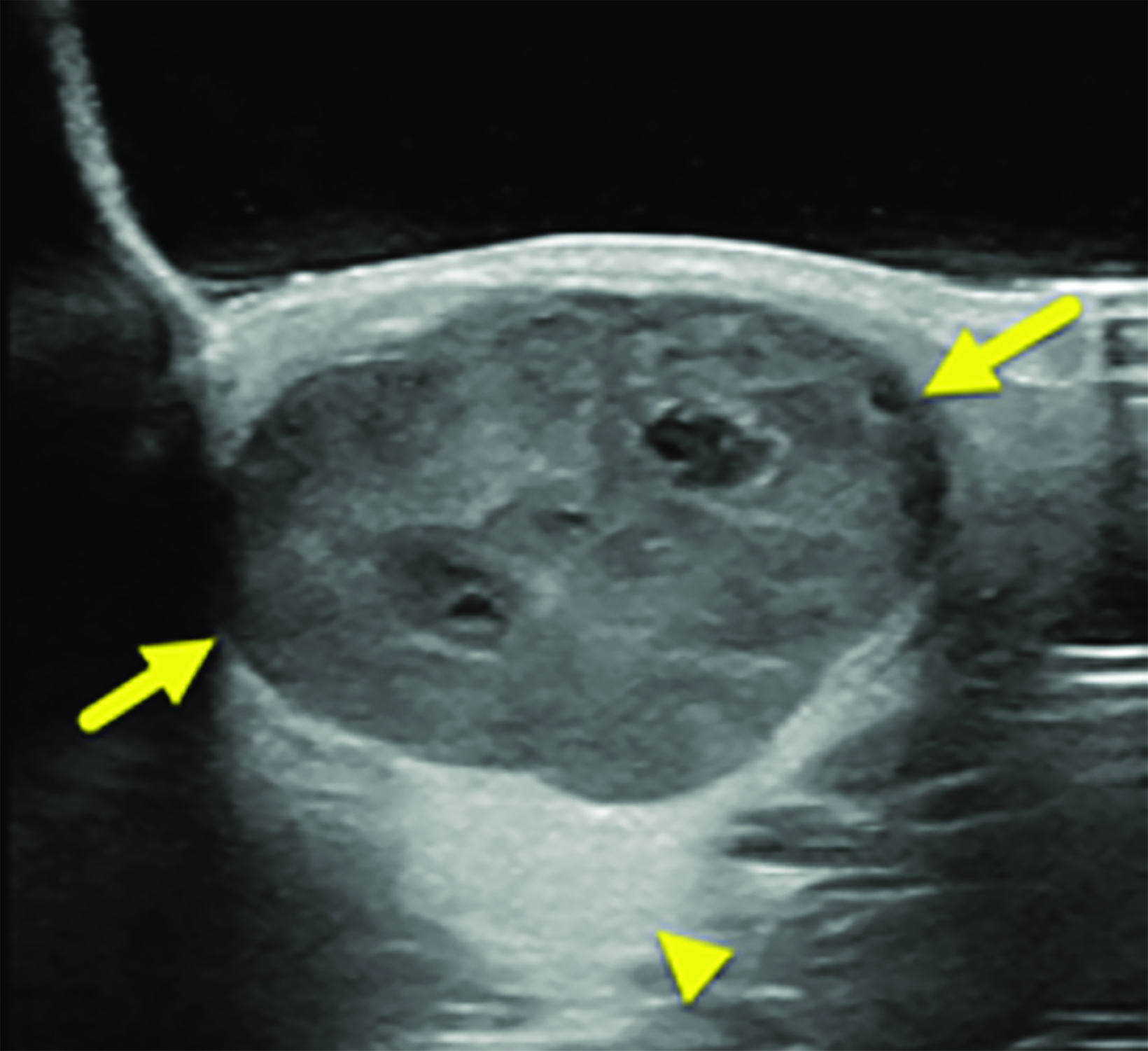
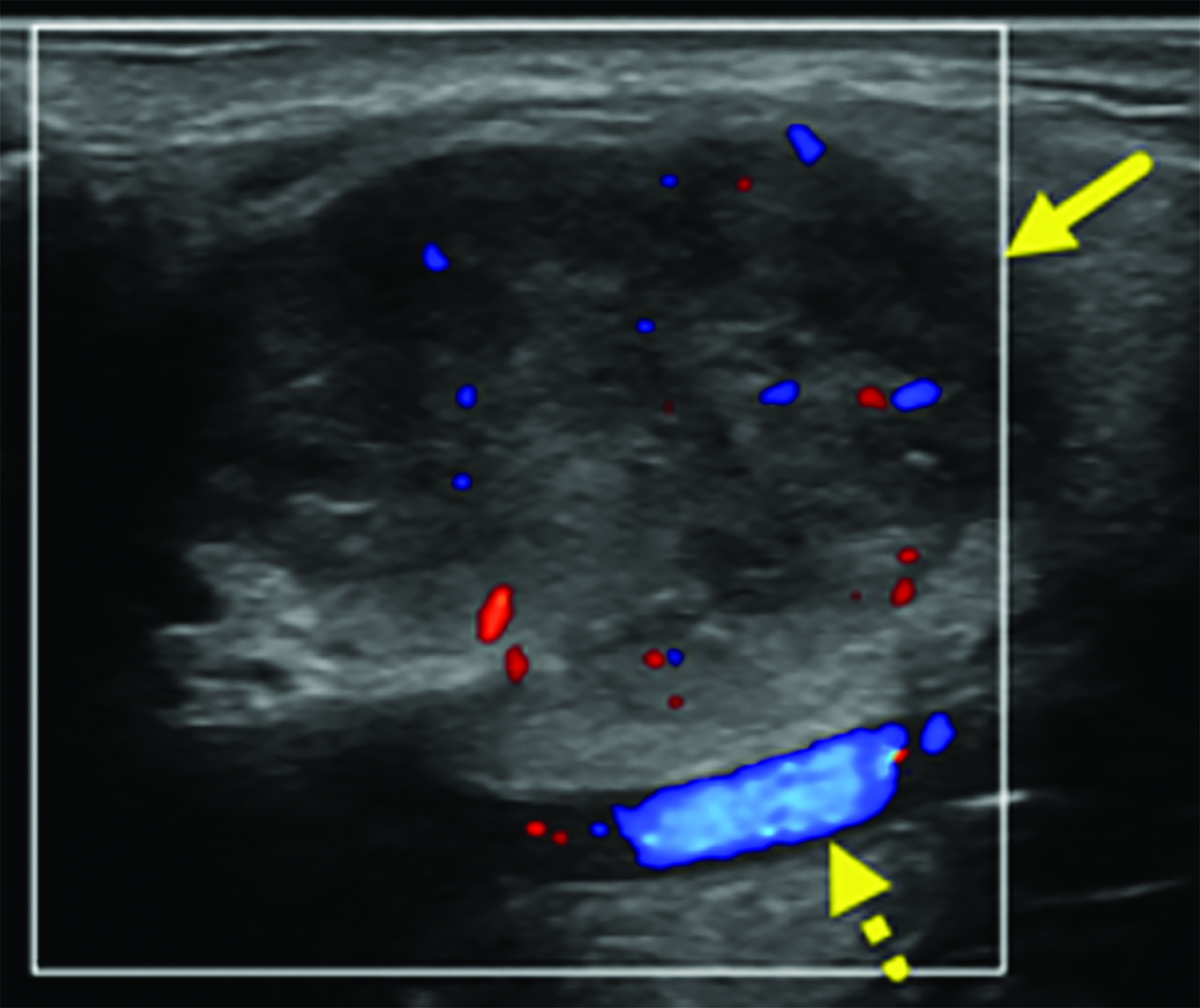
Initial ultrasound (Figure 1) of the upper neck showed a predominately solid lesion with internal cystic foci located at the angle of the left side of the mandible, within the parotid gland. A follow up ultrasound performed 6 months later showed interval growth of the mass. The appearance of the mass was unchanged, except that there was increased color flow with arterial waveforms.
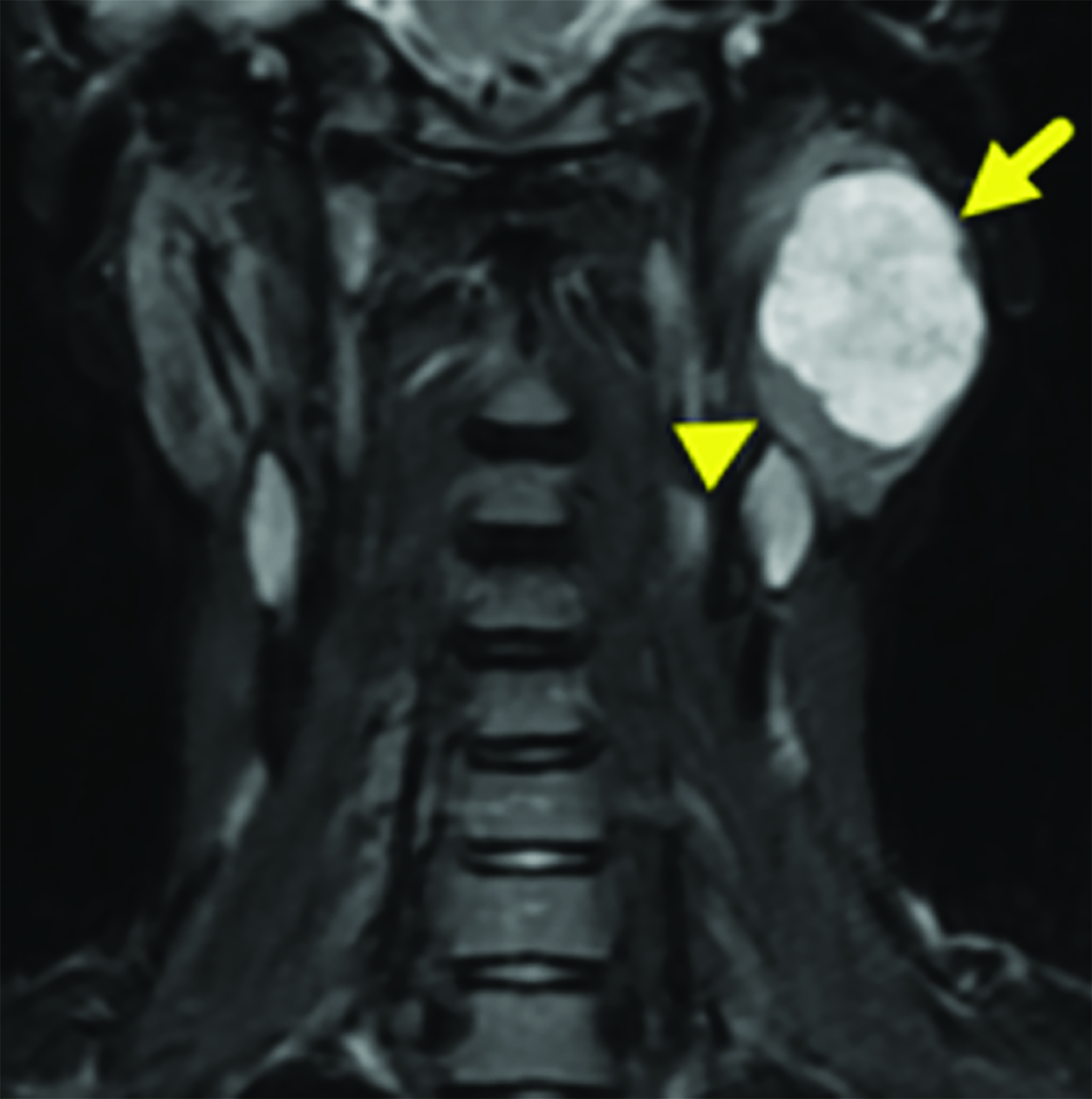
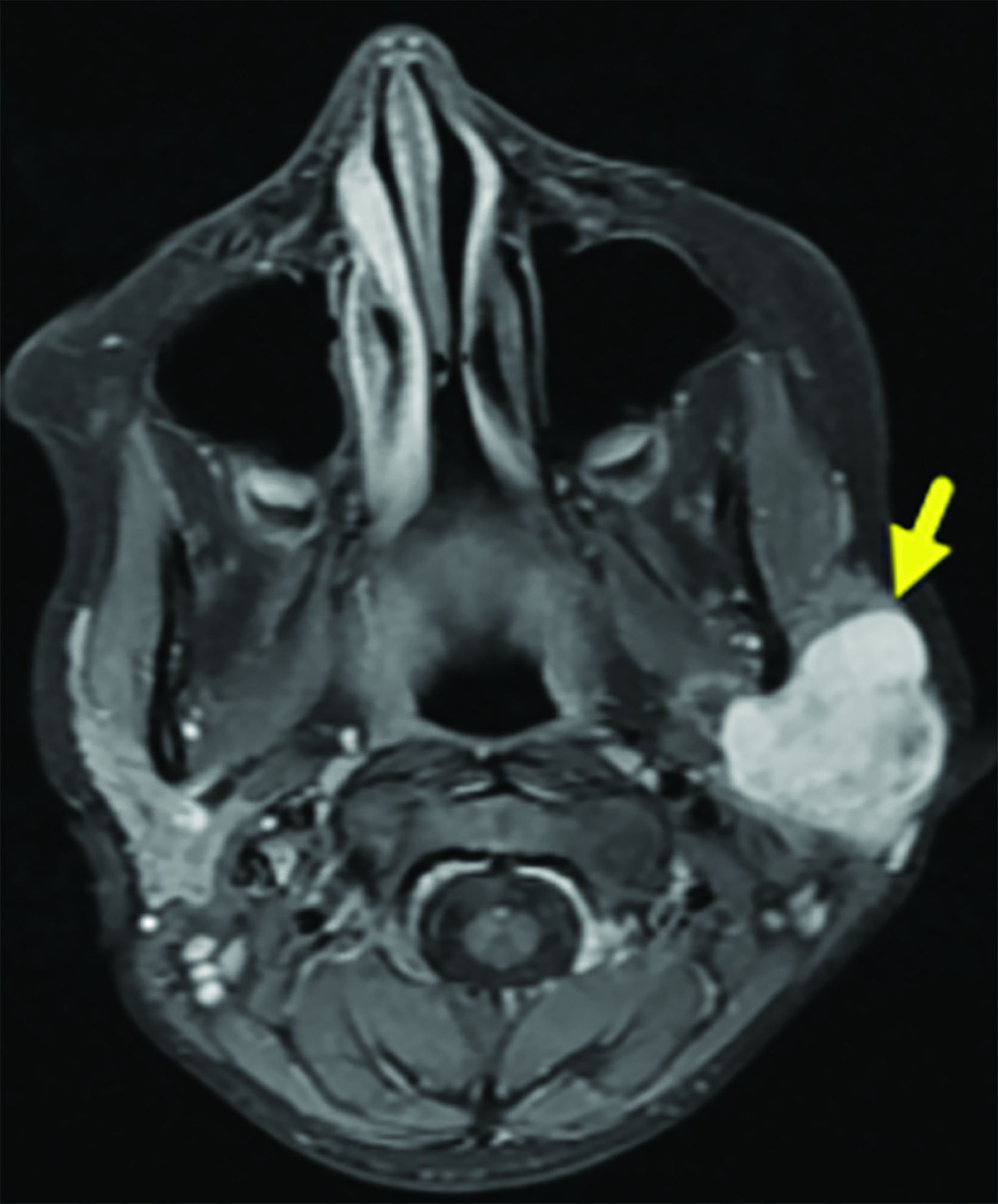
Subsequently, magnetic resonance imaging (MRI) showed a T1 hypointense, T2 hyperintense, homogeneously contrast-enhancing mass within the left parotid gland (Figure 2). The deep margin of the mass was located lateral to the carotid sheath, and a prominent arterial structure was found along the deep margin, posterior to the pterygoid muscles.
Diagnosis
Pleomorphic adenoma. The differential diagnoses for solid, intraparotid tumors in a teenager include Warthin tumor, facial nerve schwannoma, adenoma, papillary cyst adenoma, oncocytoma, lipoma, neurofibroma (solitary or plexiform types), hamartoma, lymphoepithelial tumors, acinic cell carcinoma, mucoepidermoid carcinoma, and rhabdomyosarcoma.1,2
Discussion
Pleomorphic adenomas (PA) are salivary gland tumors that often occur in the parotid gland.3 They are more common in adults, with the mean age of diagnosis ranging from 40 to 50 years of age. While pleomorphic adenomas are benign, they have the potential for malignant transformation and, because the tumor invades normal glandular tissue with pseudopodia like projections, they frequently recur after surgical resection.4
Initial evaluation of parotid gland tumors in children often begins with ultrasound. Ultrasound has high sensitivity for abnormalities in salivary glands and has the advantage of not utilizing ionizing radiation or requiring sedation.2 If ultrasound identifies a solid mass, MRI would be indicated as it allows for more complete lesion characterization, determination of lesion extent, and regional nodal assessment. On MRI PA appears as a well-circumscribed rounded mass that is bright on T2WI with homogeneous enhancement. On CT examination, PA usually appears as smooth or lobulated, homogeneous soft tissue density mass. In large masses, necrosis may be present. Occasional calcifications are common. Smaller tumors show early homogenous enhancement while in larger tumors enhancement is less prominent and can be delayed.5
Surgical resection of parotid pleomorphic adenomas is associated with a risk of injury to the facial nerve. As there are no widely agreed-upon guidelines describing the best approach to the management pleomorphic adenomas, surgical intervention is personalized based on the imaging features and risk profile of the patient. For some patients, a radical parotidectomy may be offered, while others may benefit more from localized excision or extracapsular dissection with a superficial parotidectomy.6 In our patient, a left superficial parotidectomy was performed, preserving the facial nerve.
Identification of the relationship of the tumor to the facial nerve is essential during the initial evaluation and treatment of the tumor to minimize the risk of nerve injury. Tumors located in the deep lobe or within both lobes of the parotid gland place the patient at higher risk of facial paralysis.7 Despite permanent facial paralysis being rare, careful dissection and nerve stimulation can help to identify the branches of the nerve and lessen the risks. If the tumor recurs, scar tissue from previous surgery makes dissection more challenging and increases the risk of nerve injury.7
Conclusion
Pleomorphic adenomas are benign salivary gland tumors that are rare in children. Given their high risk of recurrence and the potential for damage of the facial nerve when arising in the parotid gland, initial surgical intervention requires careful dissection of the tumor to ensure negative margins and protect the nerve. Recurrences are more common in younger patients; thus, postoperative monitoring is necessary.
References
- Jagadishkumar K, Anilkumar MG, Krishna Kumar HC, Maggad R. Pleomorphic adenoma of the cheek in a child: A case report. Dent Res J (Isfahan). 2014 Jul;11(4):522-4. PMID: 25225569; PMCID: PMC4163834.
- Sodhi KS, Bartlett M, Prabhu NK. Role of high-resolution ultrasound in parotid lesions in children. Int J Pediatr Otorhinolaryngol. 2011;75(11):1353-1358. doi:10.1016/j.ijporl.2011.07.005
- Erickson LA. Pleomorphic adenoma in the parotid gland. Mayo Clin Proc. 2017;92(3):e55-e56. doi:10.1016/j.mayocp.2017.01.006
- Aro K, Valle J, Tarkkanen J, Mäkitie A, Atula T. Repeatedly recurring pleomorphic adenoma: a therapeutic challenge. Acta Otorhinolaryngol Ital. 2019;39(3):156- 161. doi:10.14639/0392-100X-2307
- Bokhari MR, Greene J. Pleomorphic Adenoma. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430829/
- Kanatas A, Ho MWS, Mücke T. Current thinking about the management of recurrent pleomorphic adenoma of the parotid: A structured review. Br J Oral Maxillofac Surg. 2018;56(4):243-248. doi:10.1016/j.bjoms.2018.01.021
- Kuriyama T, Kawata R, Higashino M, et al. Recurrent benign pleomorphic adenoma of the parotid gland: Facial nerve identification and risk factors for facial nerve paralysis at re-operation. Auris Nasus Larynx. 2019;46(5):779-784. doi:10.1016/j.anl.2019.02.0
References
Citation
A VCWBTRSCLYT. Pleomorphic Adenoma of the Parotid Gland. Supplement to Applied Radiology. 2022;(5):14-16.
September 2, 2022