Periventricular Schwannoma
Images



Case Summary
A previously healthy child presented with left upper and lower extremity weakness and numbness.
Imaging Findings
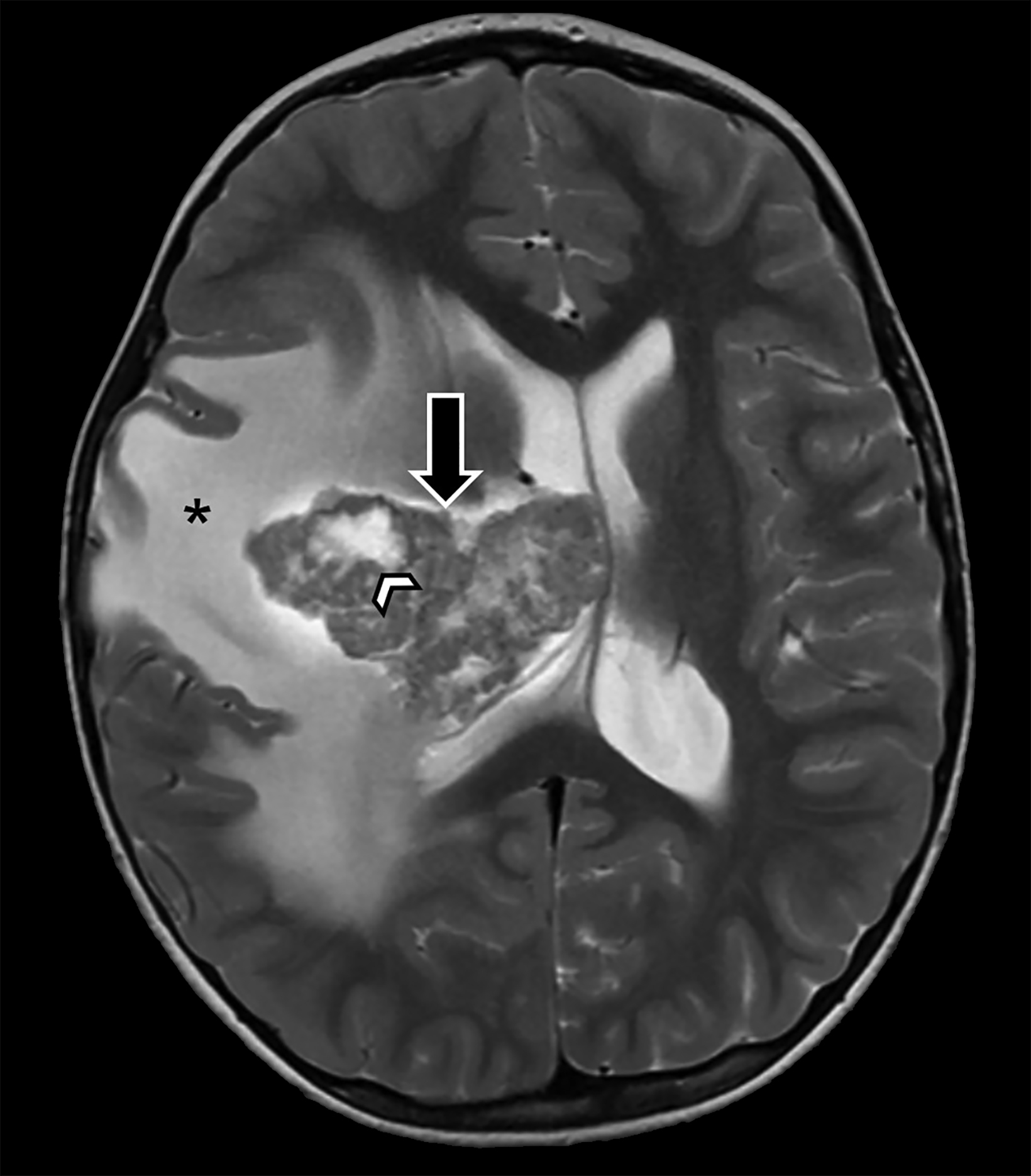
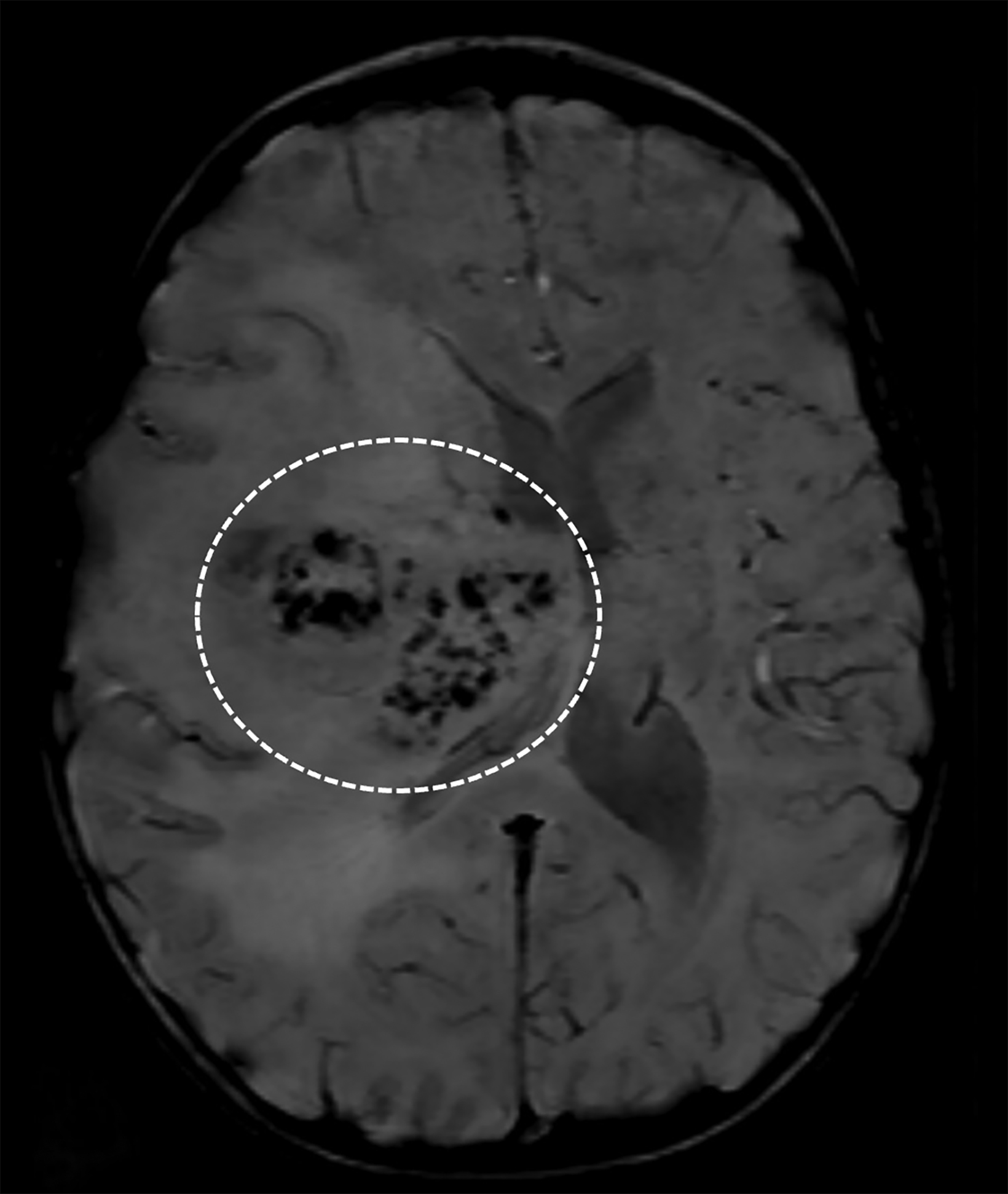
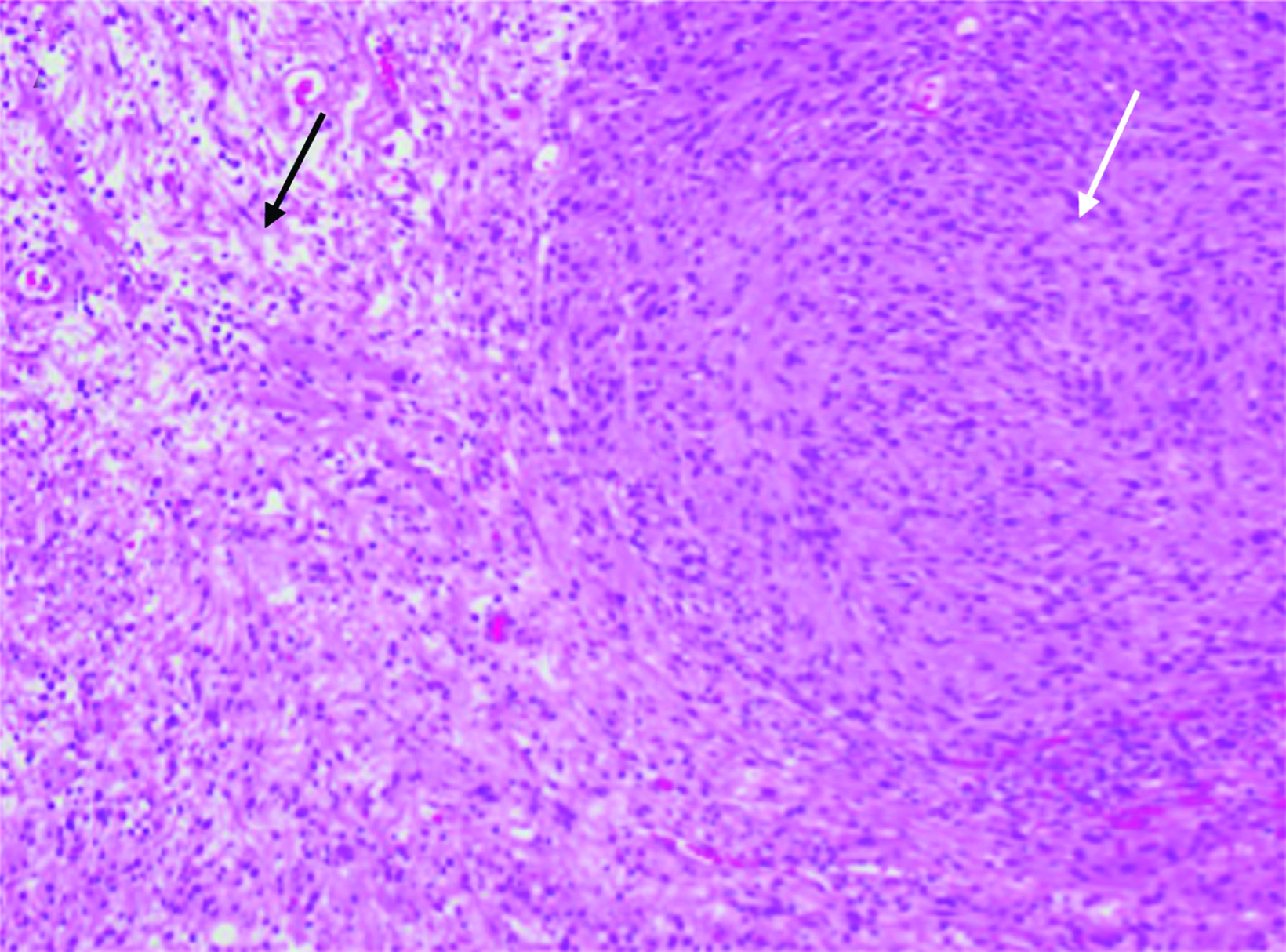
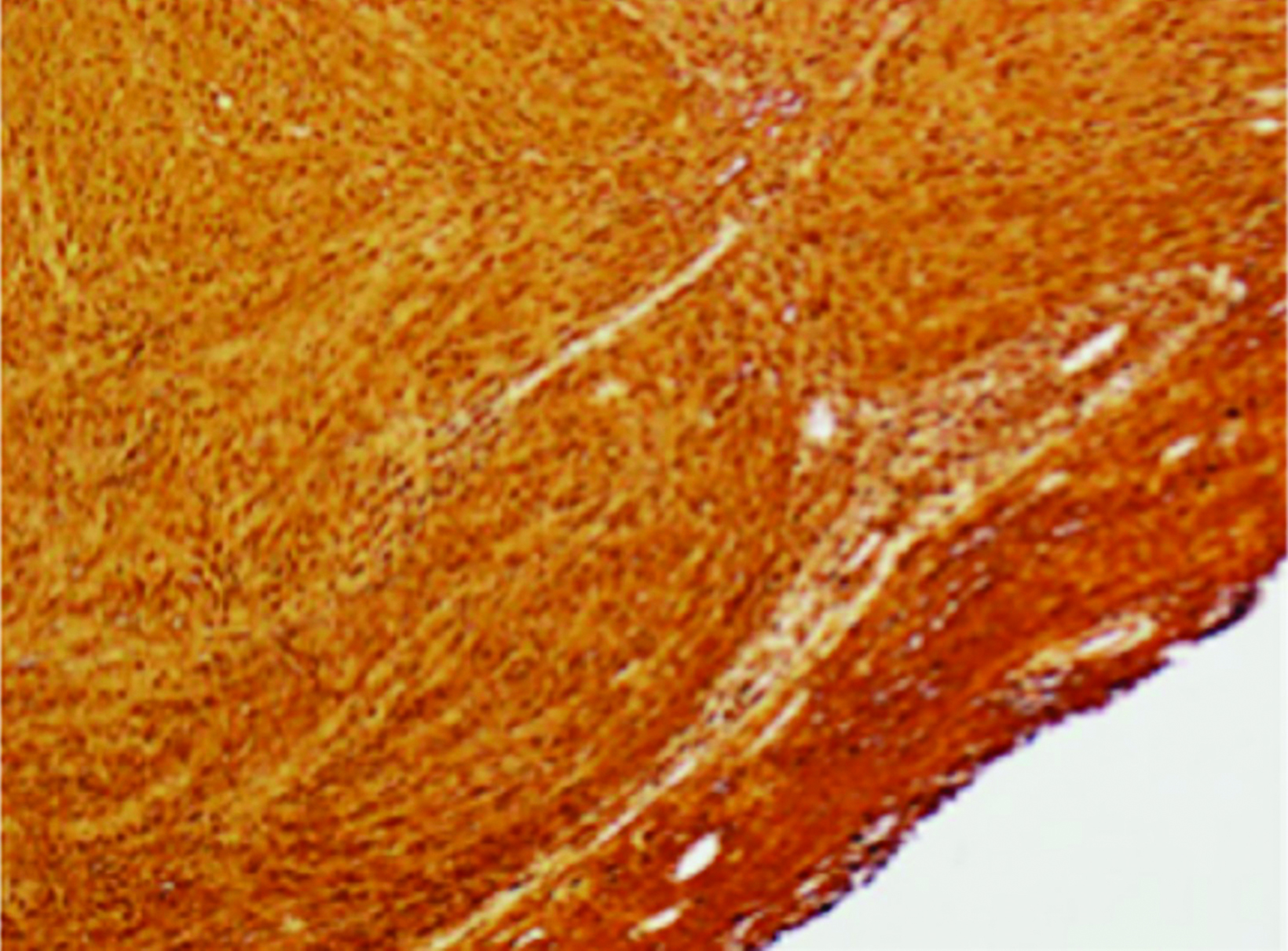
Brain MRI demonstrated a large, right periventricular mass protruding into the lateral ventricle, with surrounding vasogenic edema, producing mass effect and resulting in subfalcine herniation and midline shift (Figure 1). Histopathologic examination demonstrated a well-delineated tumor with nodules of spindle cells with Verocay bodies, hyalinized blood vessels, loose Antoni B and compact Antoni A regions, and diffusely positive S100 immunohistochemistry (Figure 2). Findings were consistent with a pathological diagnosis of schwannoma, grade I.
Diagnosis
Periventricular schwannoma. Although schwannomas have characteristic imaging findings when arising from cranial nerves, this lesion posed a diagnostic challenge due to its atypical location. The differential diagnosis for large, supratentorial intraparenchymal masses in children include glioblastoma, pilocytic astrocytoma, ependymoma, and atypical teratoid rhabdoid tumor.
Discussion
Schwannomas are benign, slow-growing nerve sheath tumors derived from Schwann cells forming the myelin sheath of peripheral nerves.1 These tumors make up 8% of all primary intracranial tumors in adults and most often arise from cranial nerve VIII.2,3 About 90% of schwannomas are solitary and sporadic; however, multiple tumors are associated with syndromic conditions such as neurofibromatosis type 2, schwannomatosis, and Carney complex. 4
Schwannomas located in the periventricular region are rare and, unlike extra-axial schwannomas, they usually present in younger individuals.
Schwann cells are normally only found outside the pia mater surrounding the nerve sheath. They do not exist in the brain parenchyma or ventricles, thus making periventricular schwannomas a rare entity.5,6 Intraoperative gross examination of this lesion demonstrated a mass originating near the lining of the lateral ventricle with intraparenchymal extension.
It has been hypothesized that a failure in neural crest cell migration during embryogenesis can result in Schwann cell remnants in the parenchyma and lining the ventricles; these cells can undergo neoplastic transformation.7 Additional theories suggest that perivascular nerve plexi may give rise to schwannomas or that the presence of multipotential mesenchymal progenitor cells in the ventricular walls may differentiate into Schwann cells.8-10
Clinical manifestations of intracranial schwannomas vary depending on location and tumor size. Rare cases of periventricular schwannomas have been reported in the literature, manifesting with nonspecific symptoms such as nausea, vomiting, headache, focal neurological deficit, and/or seizure, depending on their location and extent. They have been reported to arise from any portion of the ventricular system, most commonly the right lateral ventricle.5,11
On CT, periventricular schwannomas will appear as isodense masses and may contain cystic degeneration and calcification. On MRI, findings are nonspecific with the mass being T1 hypo-to-isointense and T2 heterogeneously hyperintense. Contrast enhancement is typically avid but heterogeneous; cyst formation may be present. Associated perilesional edema is common; however the etiology remains uncertain in this low-grade lesion.12,13 The lack of restricted diffusion may help differentiate these masses from highly cellular tumors and regions of susceptibility effect may be seen when the tumor contains calcifications and/or hemorrhagic foci.
Histopathologically, schwannomas show S100 positive cells, compact Antoni A regions, loose Antoni B regions, Verocay bodies, and hyalinized vessels.1,2
Surgical resection of periventricular schwannomas is recommended for symptomatic tumors. A very good prognosis and no recurrences have been identified at 24-month follow-up. Postoperative hydrocephalus is the most common complication. Adjuvant therapy is currently not indicated as regrowth recurrence, and/or malignant transformation of periventricular schwannomas are rare. 5,13
Conclusion
We present a rare case of periventricular schwannoma. Owing to lesion’s uncommon location, imaging-based diagnosis can be challenging, requiring histopathological diagnosis. Although the etiology of this tumor remains unproven, recent research suggests an origin from neural crest cells or multipotent mesenchymal progenitor cells along the ventricles.
Citation
R H, C K, A R, K K, S B, P H, MN S, M B, R R,. Periventricular Schwannoma. Appl Radiol. 2023;(5):38-40.
September 12, 2023