Pediatric Pineoblastoma
Images

Brought to you by Guerbet.
Case Summary
An 8-year-old boy with no significant past medical history presented for neurosurgery consultation after a brain lesion was discovered on computed tomography (CT). He presented with 3 days of headache, emesis, lethargy, and right eye pain. The headaches began 6 weeks earlier and initially occurred once a week, and since increased in frequency. He showed no changes in gait or speech, no numbness or tingling, and no abnormal gaze or nystagmus. He denied photophobia and dizziness. After initial work-up, including CT, the patient underwent magnetic resonance imaging (MRI) of the brain with and without gadolinium-based contrast.
Imaging Findings
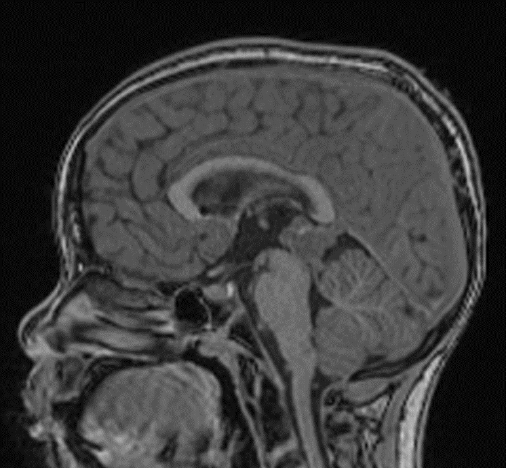
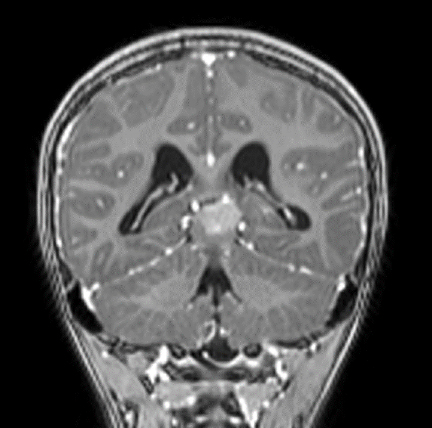
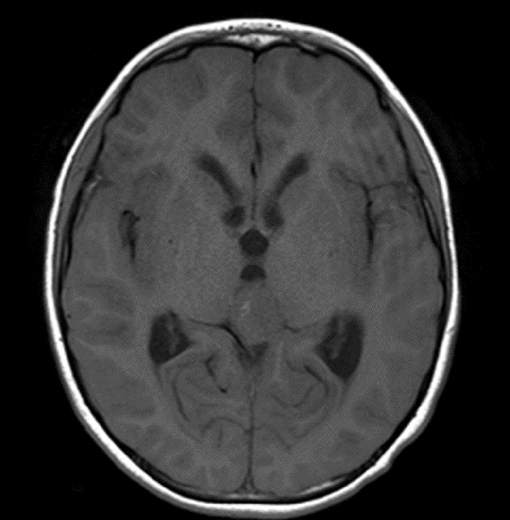
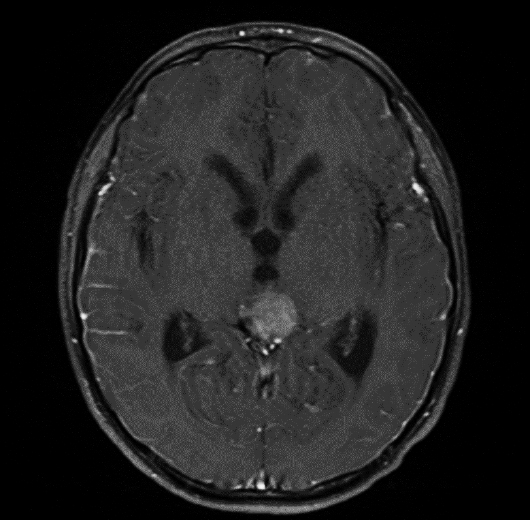
MRI with and without contrast demonstrated a 2.4 x 2.0 x 1.9 cm heterogeneously enhancing mass within the pineal recess. There was mass effect from this lesion at the level of the cerebral aqueduct, resulting in non-communicating hydrocephalus (Figure 1). A punctate focus of hyperintense T1 signal within the mass, which demonstrated signal loss on postcontrast fat-suppressed images, indicated partial fatty composition (Figure 2).
Diagnosis
Pineoblastoma
Discussion
Microscopic examination demonstrated a densely cellular proliferation of undifferentiated neoplastic cells, with sheet-like growth and small, round blue cells with hyperchromatic nuclei, high nuclear-cytoplasmic ratio, and indistinct cell borders. Tumor cells were positive for synaptophysin and showed high Ki-67 labeling index (>50%). The findings were consistent with pineoblastoma, WHO grade IV.
Pineal gland tumors are uncommon, accounting for ~1% of all central nervous system (CNS) tumors in adults and 3% in children.1-2 The tumors can be classified into three major categories: germ cell tumors (GCTs), the most common pineal tumors; pineal parenchymal tumors (PPTs), and gliomas. The WHO classification of CNS tumors divides pineal tumors into four groups: pineocytomas (Grade I), pineal parenchymal tumors of intermediate differentiation (Grade II or III), papillary tumor of the pineal region (Grade II or III), and pineoblastoma (Grade IV).3
Highly malignant and aggressive, pineoblastomas are considered primary neuroectodermal tumors (PNETs) of the pineal region.4 They hold a poor prognosis and can metastasize locally and throughout the neuroaxis.1
Contrast-enhanced magnetic resonance imaging (CEMRI) is the modality of choice for diagnosing pineoblastomas; computed tomography (CT) cannot differentiate between (PPT) and (GCT).1 On MRI, pineoblastomas are isointense on T1- weighted images and have vivid heterogeneous enhancement compared to GCTs and PPTs, which enhance homogenously. Given the disease’s predilection to spread along the neuroaxis, MRI of the brain and spine with and without contrast is important for disease recognition and quantification, and is therefore recommended1,5-6.
Clinical manifestations of pineoblastomas are similar to those of other pineal tumors. They are commonly associated with obstructive hydrocephalus, resulting in elevation of intracranial pressure. This elevation typically causes headaches, nausea/vomiting, vision abnormalities, and reduced levels of consciousness.1 In addition, compression of the tectal plate may manifest as Parinaud syndrome, which includes upward gaze palsy, convergence nystagmus, and pupillary light-near dissociation. Focal neurological deficits (FNDs) may also be prominent.7
Treatment generally begins with the management of hydrocephalus, including cerebrospinal fluid (CSF) diversion, commonly achieved by either ventriculoperitoneal (VP) shunt or endoscopic third ventriculostomy (EVP).7,8 Gross total resection of pineoblastoma has been associated with prolonged survival and better outcomes. The addition of postoperative adjuvant radiotherapy is generally recommended while the inclusion of chemotherapy as part of multimodality therapy is controversial8.
This patient underwent gross total resection and adjuvant radiotherapy; MRI surveillance demonstrated no appreciable disease for two years. The patient later showed signs of recurrence and further CEMRI studies detected metastatic lesions in the frontal lobes to help guide therapy.
Conclusion
We report a case of pineoblastoma, a highly malignant form of pineal gland tumors. Because pineoblastoma is extremely aggressive it warrants a comprehensive work-up and therapy. Contrast-enhanced MRI is essential to diagnosing this neoplasm and helps to guide disease management.
References
- Dhall G, Khatua S, Finlay JL. Pineal region tumors in children. Curr Opin Neurol. 2010;23(6):576-582. doi:10.1097/WCO.0b013e3283404ef1
- Ramasubramanian A, Kytasty C, Meadows AT, Shields JA, Leahey A, Shields CL. Incidence of pineal gland cyst and pineoblastoma in children with retinoblastoma during the chemoreduction era. Am J Ophthalmol. 2013;156(4):825-829. doi:10.1016/j.ajo.2013.05.023
- Brat DJ, Parisi JE, Kleinschmidt-DeMasters BK, et al. Surgical neuropathology update: a review of changes introduced by the WHO classification of tumours of the central nervous system, 4th edition. Arch Pathol Lab Med. 2008;132(6):993-1007. doi:10.1043/1543-2165(2008)132[993:SNUARO]2.0.CO;2
- Borit A, Blackwood W, Mair WG. The separation of pineocytoma from pineoblastoma. Cancer. 1980;45(6):1408-1418. doi:10.1002/1097-0142(19800315)45: 6<1408::aid-cncr2820450619>3.0.co;2-0
- Pham TT, Siebert E, Asbach P, Willerding G, Erb-Eigner K. Magnetic resonance imaging based morphologic evaluation of the pineal gland for suspected pineoblastoma in retinoblastoma patients and age-matched controls. J Neurol Sci. 2015 Dec 15;359(1-2):185-92. doi: 10.1016/j.jns.2015.10.046. Epub 2015 Oct 28. PMID: 26671110.
- Galluzzi P, de Jong MC, Sirin S, et al. MRI-based assessment of the pineal gland in a large population of children aged 0-5 years and comparison with pineoblastoma: part I, the solid gland. Neuroradiology. 2016;58(7):705-712. doi:10.1007/s00234-016-1684-z
- Tate MC, Rutkowski MJ, Parsa AT. Contemporary management of pineoblastoma. Neurosurg Clin N Am. 2011;22(3):409-ix. doi: 10.1016/j.nec.2011.05.001
- Tate M, Sughrue ME, Rutkowski MJ, Kane AJ, Aranda D, McClinton L, McClinton L, Barani IJ, Parsa AT. The long-term postsurgical prognosis of patients with pineoblastoma. Cancer. 2012 Jan 1;118(1):173-9. doi: 10.1002/cncr.26300. Epub 2011 Jun 29. PMID: 21717450.