Part 2: Classic signs in gastrointestinal radiology
By Baldwin M, Genant J, Braver J, Mortele KJ













This is the second part of a 3-part article by Drs. Baldwin, Genant, Braver, and Mortele.
Dr. Baldwin is a Radiologist at South Shore Hospital, Weymouth, MA; Dr. Genant is an Associate Professor of Radiology at San Francisco Medical Center, San Francisco, CA; Dr. Braver is the Director of Gastrointestinal Radiology at Brigham & Women’s Hospital and an Assistant Professor at Harvard Medical School, Boston, MA; and Dr. Mortele is the Director of the Division of Clinical MRI at Beth Israel Deaconess Medical Center, Boston, MA, and the Associate Professor of Radiology at Harvard Medical School, Boston, MA.
The names of many classic radiologic signs derive from analogues to objects commonly encountered in everyday life; eg, the “comb” sign. The use of familiar objects to describe visual findings enables radiologists both to arrive at a correct diagnosis and to effectively convey such diagnostic findings to clinicians.
Comb sign
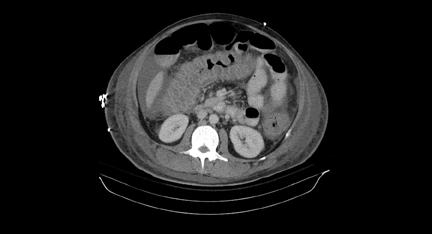
The “comb sign” is seen in the presence of Crohn’s disease. This sign is observed on contrast-enhanced CT or magnetic resonance imaging (MRI) scans. The teeth of the comb in this instance represent engorged small arteries, the vasa recta, perfusing the small bowel (Figure 14).37
The vasa recta of the small bowel seen in Crohn’s disease become tortuous and enlarged. They appear as prominent opacities on the mesenteric side of the small bowel. These small arteries become engorged due to increased blood flow to the inflamed small bowel and are accentuated due to the fibrofatty proliferation in the mesentery. The presence of the comb sign suggests an acute exacerbation of Crohn’s disease.37
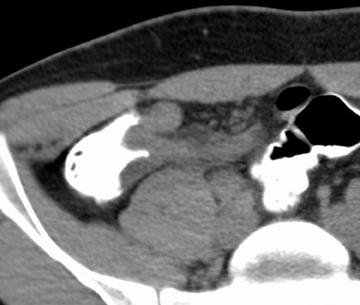
Target sign
The “target sign” represents an enhancement pattern of the bowel wall seen in various disease processes on contrast-enhanced CT or MRI scans. The target-like appearance is formed when a thickened bowel wall demonstrates alternating degrees of attenuation, with an inner and outer layer of higher attenuation and a middle layer of lower attenuation (Figure 15).38
The higher-attenuation inner and outer layers represent the mucosa and muscularis propria, respectively. The high attenuation of these layers is believed to be secondary to contrast enhancement from inflammation. The lower attenuation middle layer is thought to be due to submucosal bowel wall edema.39 Submucosal edema can be seen even on noncontrast-enhanced CT if severe.38,40
The target sign is classically seen in patients with Crohn’s disease. It can, however, be seen in many other conditions. This pattern of bowel wall enhancement has been observed in patients with radiation enteritis, GVHD, ischemic bowel, intramural hemorrhage, vasculitides such as Henoch-Schonlein purpura, and pseudomembranous colitis.41-44
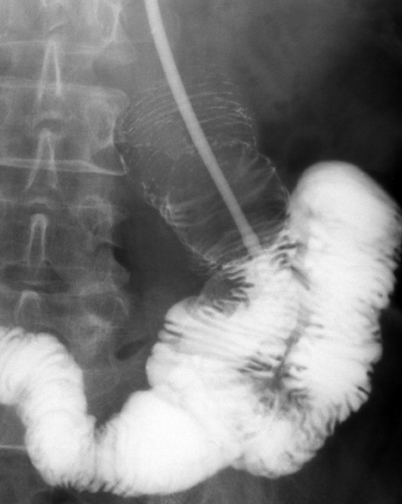
Coiled spring sign
In 1929, Artner was the first to describe concentric ring shadows in a barium-filled cecum with a central filling defect. He found that this appearance resulted from an inverted appendiceal stump protruding into the cecum.45
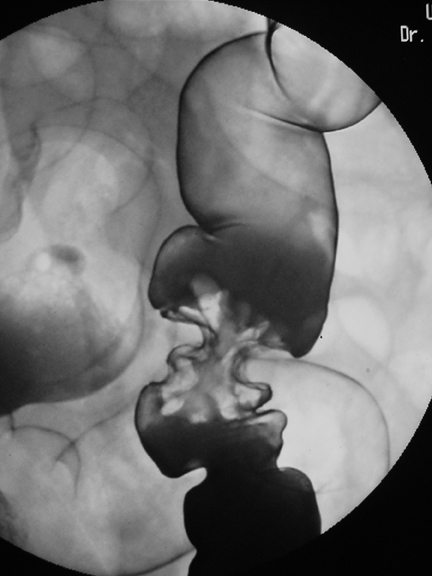
The “coiled spring” sign can be seen anywhere in the bowel where an intussusception has occurred. These ring shadows represent contrast reflux within the lumen between the walls of the intussusceptum and intussuscipiens (Figure 16).46
Classically, this sign describes the appearance of the cecum in the presence of appendiceal intussusception, a rare entity. It is thought that the coiled-spring appearance results from intussusception of the cecal tip with the invaginated appendix acting as the lead point for variable amounts of cecocecal or cecocolic intussusception.47,48
Arrowhead sign
The “arrowhead” sign can be observed on CT images in the setting of acute appendicitis. This perceived arrowhead shape is secondary to focal, symmetric thickening of the cecal wall secondary to spreading inflammation from appendicitis (Figure 17). The cecal wall thickening causes funneling of oral or rectal contrast material within the upper cecum, which points to the obstructed appendiceal orifice.49
An air-arrowhead sign has also been described, which represents gas trapped in the thickened, inflamed cecum. The “arrowhead sign” represents a secondary sign of appendicitis and has been shown to have a sensitivity of roughly 30%.50
Thumbprint sign
The “thumbprint sign” was first described in 1963.51,52 This sign describes smooth, rounded impressions causing filling defects classically seen in barium studies of ischemic colitis.53 These nodular densities represent edema and hemorrhage into the wall of the colon most commonly secondary to ischemia (Figure 18).
This sign is seen in roughly 75% of cases of transient, nongangrenous ischemic colitis.54 These soft tissue densities resolve once the colon wall has been reperfused and healed. The thumbprint sign can also be seen on CT as nodular, soft-tissue thickening of the wall of the colon.55
Pseudomembranous colitis, ulcerative colitis, lymphoma, leukemia, and hemorrhage into the bowel wall from coagulopathies may also produce the thumbprint sign.56
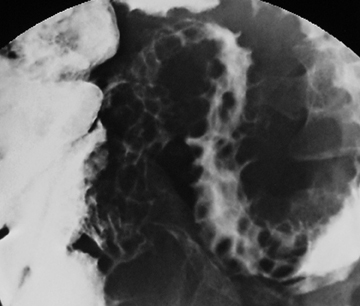
Cobblestone sign
The “cobblestone sign” is classically seen within the small and large bowel on fluoroscopic studies in the presence of active Crohn’s disease. The cobblestone appearance of the bowel wall is due to a combination of extensive, broad, linear transverse and longitudinal ulcerations within an inflamed mucosal surface. Only scattered islands of normal mucosa remain in this setting (Figure 19).57
The presence of scattered islands of relatively normal mucosa can lead to the misperception that the predominant ulcerated regions are the baseline mucosa and the normal mucosal islands are polyps. Thus, the differential diagnosis for cobblestoning is inflammatory polyposis in the setting of inflammatory bowel disease.57
Bowler hat sign
The “bowler-hat sign” represents the appearance of a sessile colonic polyp observed at an oblique angle on a double contrast barium enema. The bowler-hat sign is formed by a ring of barium adjacent to the base of the polyp surrounding a domed layer of barium coating the surface of the polyp (Figure 20).58
A colonic diverticulum can partially fill with barium and also produce a bowler hat appearance. The orientation of the dome of the bowler hat sign can help differentiate a polyp from a diverticulum. An intraluminal polyp will result in a bowler-hat sign with its dome pointed inward toward the lumen, while a diverticulum will produce a bowler hat sign pointed outward.59 Other intraluminal objects, such as stool or air bubbles, can also rarely create the bowler hat sign. However, entities can be differentiated from polyps due to their mobility.
Mexican hat sign
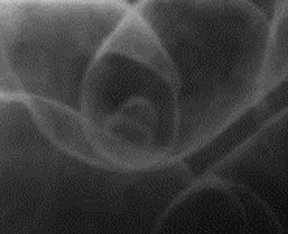
Pedunculated colonic polyps form the “Mexican hat sign.” These polyps possess discrete stalks and occasionally can be observed “en face” hanging from the nondependent wall of the colon on double contrast barium enemas.
The Mexican hat sign is formed by the appearance of 2 concentric rings; the outer ring represents the “en face” visualization of barium coating the surface of the head of a pedunculated polyp, while the inner ring represents a meniscus of barium surrounding the stalk of the polyp visualized through the head (Figure 21).58
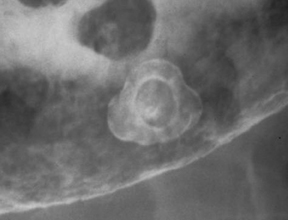
Collar button sign
“Collar button ulcers” are manifestations of inflammatory processes within the bowel. These deep ulcerations are classically seen in the colon associated with active ulcerative colitis. The collar button appearance is formed by mucosal ulceration with associated undermining of the ulcer’s edge by lateral submucosal extension (Figure 22). Vertical penetration into the bowel wall is limited due to the resistance of the underlying muscularis mucosa, thus resulting in the discoid collar button appearance of these ulcers.60 Collar button ulcers have also been observed in the setting of other inflammatory bowel processes, such as Crohn’s disease, ischemic colitis, and shigellosis.61,62
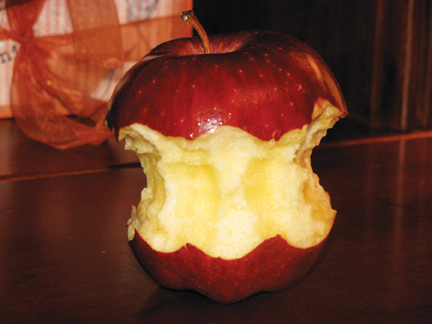
Apple core sign
The “apple core sign” was first described in barium enema examinations of the colon. The apple core appearance is the visual manifestation of an annular lesion of the bowel with irregular overhanging edges and shouldered margins (Figure 23). The apple core sign is classically seen in cases of colon carcinoma.
This appearance is most commonly located in the sigmoid colon as well as in the ascending, transverse, and descending colon. The apple core sign is not seen in the larger-caliber cecum.63 The differential diagnosis of a lesion with an apple core appearance is focal diverticulitis, ischemic colitis, ulcerative colitis, endometriosis, amebiasis, serosal metastatic implants, infectious colitis and, rarely, focal amyloidosis.64
Accordion sign
The “accordion sign” describes the appearance of colonic wall thickening in the setting of colitis. It was originally felt to be a specific CT finding for Clostridium difficile-induced pseudomembranous colitis, but it has also been described with colitides of differing etiologies.
This sign describes the appearance of alternating, edematous haustral folds that are due to transmural edema and are separated by transverse mucosal clefts filled with oral contrast (Figure 24).65 Oral contrast is trapped between thickened, edematous colonic folds and pseudomembranes in the setting of C. difficile-induced pseudomembranous colitis.66
The accordion sign has also been observed with colonic edema secondary to cirrhosis and in Crohn’s disease, ischemic colitis, lupus vasculitis, and infectious colitis.66,67
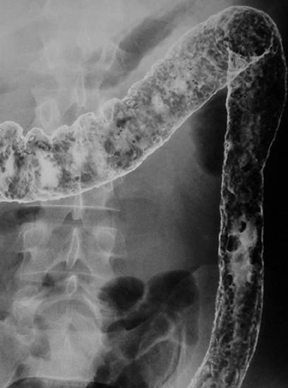
Lead pipe sign
The “lead pipe sign” was first demonstrated on barium examinations of the colon. The lead pipe appearance of the colon is classically seen with chronic, smoldering ulcerative colitis.68 The lead pipe appearance likely represents the visual manifestation of multiple pathophysiological processes. There is increased regeneration of the colonic mucosa in ulcerative colitis. This mucosal regeneration may lead to hypertrophy of the muscularis mucosae.69,70 Contraction of this hypertrophic muscle layer gives the colon the lead pipe-like narrowed, ahaustral, and foreshortened appearance (Figure 25).70,71 Luminal narrowing may also be caused by previously formed strictures and fat distribution within the submucosal layer of the bowel wall, particularly the rectum.69,71 Extramural fat proliferation, particularly in the perirectal region, can also play a role in luminal narrowing.72
The differential diagnosis for a lead pipe appearance of the colon includes Crohn’s disease, cathartic colon (which usually occurs in the descending colon and spares the rectum), tuberculosis, and, rarely, amebiasis.73
REFERENCES
- Madureira AJ. The comb sign. Radiology. 2004;230:783-784.
- Ahualli J. The target sign: Bowel wall. Radiology. 2005;234:549-550.
- Wittenberg J, Harisinghani MG, Jhaveri K, et al. Algorithmic approach to CT diagnosis of the abnormal bowel wall. Radiographics. 2002;22:1093-1109.
- Segatto E, Mortele KJ, Ji H, etal. Acute small bowel ischemia: CT imaging findings. Semin Ultrasound CT MR. 2003;24:364-376.
- Macari M, Balthazar EJ. CT of bowel wall thickening: Significance and pitfalls of interpretation. Am J Gastroenterol.2001;176:1105-1116.
- Balthazar EJ. CT of the gastrointestinal tract: Principles and interpretation. Am J Gastroenterol.1991;156:23-32.
- Horton KM, Corl FM, Fishman EK. CT Evaluation of the colon: Inflammatory disease. Radiographics 2000;20:399-418.
- Macari M, Chandarana H, Balthazar EJ, Babb J. Intestinal ischemia versus intramural hemorrhage: CT evaluation. Am J Gastroenterol. 2003;180:177-184.
- Artner, H. Der status post appendectomiam im rontergenbilde. ROFO. 1929;39:609-615.
- Choi HC, Han JK, Kim SH, et al. Intussusception in adults: From stomach to rectum. Am J Gastroenterol.2004;183:691-698.
- Meyers MA, Abrams J. Intussusception of the appendix. Br J Radiol.1970;43:485-487.
- Levine MS, Trenker SW, Herlinger H, et al. Coiled-spring sign of appendiceal intussusception. Radiology. 1985;155:41-44.
- Rexroad JT. The CT arrowhead sign.Radiology. 2003;227:44-45.
- Rao PM, Wittenberg J, McDowell RK, et al. Appendicitis: Use of arrowhead sign for diagnosis at CT. Radiology. 1997;202:363-366.
- Schwartz S, Boley SJ, Lash J, Sternhill V. Roentgenologic aspects of reversible vascular occlusion of colon and its relationship to ulcerative colitis. Radiology. 1963;80:625-635.
- Boley SJ, Schwartz S, Lash J, Sternhill V. Reversible vascular occlusion of colon. Surg Gynecol Obstet. 1963;116:53-60.
- Wittenberg J, Athanasoulis CA, Williams LF, et al. Ischemic colitis. Radiology and pathophysiology. Am J Gastroenterol.1975;123:287-300.
- Iida M, Mitsuo MI, Matsui T, et al. Ischemic colitis: Serial changes in double-contrast barium enema examination. Radiology.1986;159:337-341.
- Alpern MB, Glazer GM, Francis IR. Ischemic or infarcted bowel: CT findings. Radiology. 1988;166:149-152.
- Ros PR, Buetow PC, Pantograg-Brown L, et al. Pseudomembranous colitis. Radiology. 1996;198:1-9.
- Buck JL, Dachman AH, Sobin LH. Polypoid and pseudopolypoid manifestations of inflammatory bowel disease. Radiographics. 1991;11:293-304.
- Miller WT, Levine MS, Rubesin SE, Laufer I. Bowler-hat sign: A simple principle for differentiating polyps from diverticula. Radiology. 1989;173:615-617.
- Levine MS, Rubesin SE, Laufer I, Herlinger H. Diagnosis of colorectal neoplasms at double-contrast barium enema examination. Radiology. 2000;216:11-18.
- Lichtenstein JE, Madewell JE, Feigin DS. The collar button ulcer. A radiologic-pathologic correlation. Gastrointest Radiol. 1979;4:79-84.
- Farman J, Rabinowitz JG, Meyers MA. Roentgenology of infectious colitis. Am J Roentgenol Radium Ther Nucl Med. 1973;119:375-381.
- McElfatrick RA, Wurtzebach LR. Collar-button ulcers of the colon in a case of shigellosis.Gastroenterology. 1973;65:303-307.
- McCarthy PA, Rubesin SE, Levine MS. Colon cancer: Morphology detected with barium enema examination versus histopathologic stage. Radiology. 1995;197:683-687.
- Simpkins KC, Young AC. The differential diagnosis of large bowel strictures. Clin Radiol. 1971;22:449-457.
- O’Sullivan SG. The accordion sign. Radiology. 1998;206:177-178.
- Macari M, Balthazar EJ, Megibow AJ. The accordion sign at CT: A nonspecific finding in patients with colonic edema. Radiology. 1999;211:743-746.
- Mountanos GI, Manolakakis IS. The accordion sign at CT: Report of a case of Crohn’s disease with diffuse colonic involvement. Eur Radiol. 2001;11:1433-1434.
- Roggeveen MJ, Tismenetsky M, Shapiro R. Best cases from the AFIP: Ulcerative colitis. Radiographics. 2006;26:947-951.
- Gore RM, Balthazar EJ, Ghahremani GG, Miller FH. CT features of ulcerative colitis and Crohn’s disease. AJR Am J Roentgenol.1996;167:3-15.
- Lichtenstein JE. Radiologic-pathologic correlation of inflammatory bowel disease. Radiol Clin North Am. 1987;25:3-24.
- Carucci LR, Levine MS. Radiographic imaging of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:93-117.
- Gore RM. CT of inflammatory bowel disease. Radiol Clin North Am. 1989;27:717-729.
- Kolawole TM, Lewis EA. Radiologic observations on intestinal amebiasis. Am J Roentgenol Radium Ther Nucl Med. 1974;122:257-265.
