Osteopoikilosis
Images




CASE SUMMARY
An 11-year-old girl with a medical history of eczema and myopia presented for imaging with a primary complaint of right hand pain and hypothenar swelling. The patient stated that she did not have any recent trauma to her hand.
IMAGING FINDINGS
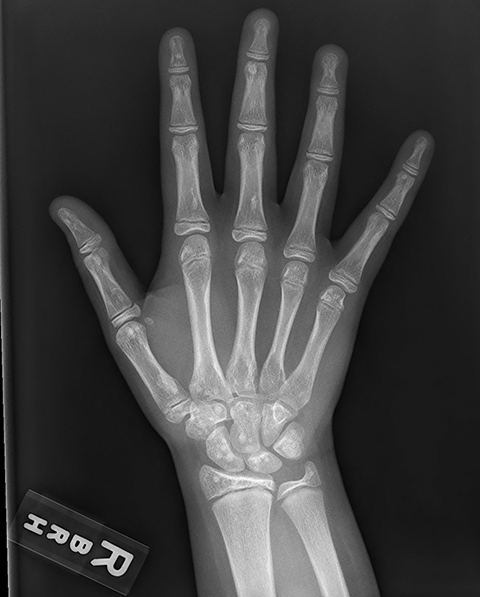
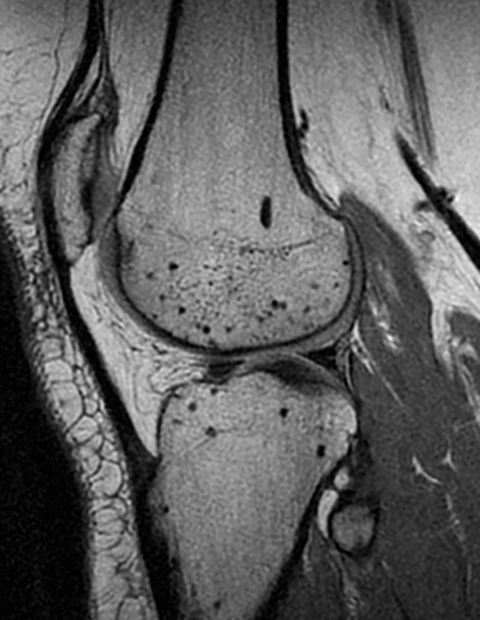
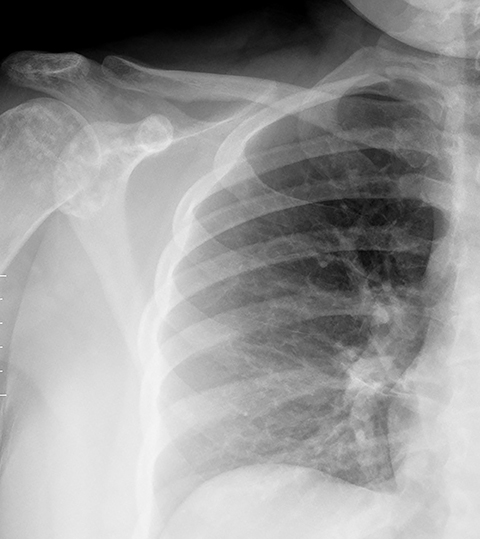
Radiography of the right hand demonstrated multiple, small sclerotic lesions distributed throughout the bones of the right hand. These lesions were concentrated in the carpal bones, the metacarpals and the phalanges as well as in the epiphysis of the radius and ulna. Follow-up MRI revealed similar lesions that were dark on T1- and T2-weighted images. A radiograph of the right ankle was obtained two years later and showed numerous round and oval small sclerotic foci throughout the visualized bones, like those seen on the prior hand radiograph. Subsequent radiographs of the left knee (performed five years after the original diagnosis) and chest (performed seven years after the original diagnosis) showed innumerable tiny sclerotic foci throughout many of the imaged bones. However, the vertebral bodies and ribs were not noted to have any lesions.
DIAGNOSIS
>Osteopoikilosis. The differential diagnosis includes osteoblastic bone metastasis, tuberous sclerosis, mastocytosis, melorheostosis, and osteopathia striata.
DISCUSSION
Osteopoikilosis is an autosomal dominant sclerosing bone dysplasia that results in focal deposits of thickened lamellar bone in the spongiosa.1 Albers-Schonberg and Ledoux-Lebard initially characterized osteopoikilosis in 1915. Since then it has been found to have an estimated incidence of 1:50,000.2 Although the pathophysiologic mechanism has not yet been identified, it is believed to be multifactorial in nature and possibly related to a loss-of-function mutation in the LEMD3 gene (also known as MAN1 gene).3 This gene is responsible for encoding an inner nuclear membrane protein and regulating two cellular pathways, including the transforming growth factor beta (TGF-β) pathway and the bone morphogenic protein (BMP) pathway.3 Both the TGF-β and BMP pathway are known to be involved in the growth of new bone.3 In addition to osteopoikilosis, researchers have shown that the LEMD3 mutation has been associated with other sclerosing bone diseases, including Buschke-Ollendorff syndrome and melorheostosis.3
Osteopoikilosis is typically discovered late in childhood or puberty and most of the time persists for the remainder of a patient’s life. Patients are usually asymptomatic at initial presentation and have an unremarkable clinical exam. However, studies have found that in 15-20% of cases patients have mild joint pain and even joint effusions; whether these symptoms are secondary to the actual disease process or prior injury is not yet understood.
Imaging plays a vital role in the identification and diagnosis of osteopoikilosis and typical findings are similar to the ones presented in this case. On plain radiograph and CT, images show reveal multiple small (2-10mm), round, ovoid, and linear sclerotic lesions that are concentrated around the physis, both in the epiphysis and the metaphysis.5 Osteopoikilosis lesions often occur symmetrically throughout the appendicular skeleton and pelvis and typically spare the vertebral column, ribs, and skull, while the metacarpal bones of the hands are always involved.5 The lack of lesions within the vertebral bodies helps to differentiate osteopoikilosis from the multiple sclerotic bone lesions seen in tuberous sclerosis.6
On MRI, these lesions are small and dark on both T1- and T2-weighted images, as they are composed of dense cortical bone.5 In order to distinguish between osteopoikilosis and osteoblastic metastasis, skeletal scintigraphy with technetium-99m is occasionally performed. While osteopoikilotic lesions normally do not demonstrate any uptake of radiotracer, osteoblastic metastasis produce “hot spots” on bone scans.5 However, given the typical imaging appearance of this disorder, no additional imaging is typically required unless the patient has a known primary tumor.
Although biopsying lesions is rarely needed in the diagnosis of osteopoikilosis, it is occasionally performed to rule out any other potential diagnoses. When performed, histology reveals foci of thickened trabeculae of lamellar bone with evidence of normal functioning osteoblasts and osteoclasts.7
Osteopoikilosis itself is a benign disease process but it has been associated with multiple skeletal and dermatologic diseases including spinal stenosis, cleft palate, dwarfism, scleroderma and syndactyly.8 In addition, numerous complications have been reported in patients with osteopoikilosis, including hip fracture and malignant transformation into osteosarcoma, giant cell tumor and chondrosarcoma.8 Management for osteopoikilosis is limited to pain control, if needed, with non-steroidal anti-inflammatory drugs.9
CONCLUSION
Osteopoikilosis is a rare bone disorder diagnosed at imaging. Because of its characteristic imaging appearance, it is considered a skeletal “don’t touch” lesion. In certain patients with a known osteoblastic tumor, it may be difficult to differentiate osteopoikilosis from osteoblastic metastasis.
REFERENCES
- Boulet C, Madani H, Lenchik L, et al. Sclerosing bone dysplasias: genetic, clinical and radiology update of hereditary and non-hereditary disorders. Br J Radiol. 2016;89(1062):20150349.
- Drouin CA, Grenon H. The association of Busckhe-Ollendorf syndrome and nail-patella syndrome. J Am Acad Dermatol. 2002; 46:621–625.
- Hellemans J, Preobrazhenska O, Willaert A, et al. Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet. 2004;36(11):1213-1218.
- Borman P, Ozoran K, Aydoğ S, Coşkun S. Osteopoikilosis: report of a clinical case and review of the literature. Joint Bone Spine. 2002;69(2):230-233.
- Gaillard, Frank. “Osteopoikilosis.” Radiopaedia.org, Apr. 2017, radiopaedia.org/articles/osteopoikilosis-2.
- Boronat S, Barber I, Thiele EA. Sclerotic bone lesions in tuberous sclerosis complex: A genotype-phenotype study. Am J Med Genet A. 2017 May 9. doi: 10.1002/ajmg.a.38260. [Epub ahead of print].
- Hellemans J, Debeer P, Wright M, et al. Germline LEMD3 mutations are rare in sporadic patients with isolated melorheostosis. Hum Mutat. 2006;27(3):290.
- Carpintero P, Abad JA, Serrano P, Serrano JA, Rodríguez P, Castro L. Clinical features of ten cases of osteopoikilosis. Clin Rheumatol. 2004;23(6):505-508.
- Mahbouba J, Mondher G, Amira M, Walid M, Naceur B. Osteopoikilosis: A rare cause of bone pain. Caspian J Intern Med. 2015;6(3):177-179.
Citation
S W, RB T, AJ T. Osteopoikilosis. Appl Radiol. 2019;(2):40-41.
March 28, 2019