Osteomyelitis with associated fracture in the toe as seen on high-resolution SPECT-CT
Images




Supplement to Applied Radiology December 2012, sponsored by Philips
Dr. Muzaffar is a Fellow and Dr. Osman is the Program Director of the Division of Nuclear Medicine, Department of Radiology, Saint Louis University Hospital, St. Louis, MO.
Case summary
A 16-year-old female presented to our outpatient clinic with complaints of pain in the right foot, lower back, right hand, and left knee. She had a history of recurrent cellulitis of the right foot. The most recent episode of active osteomyelitis was diagnosed in the right fourth phalanx by physical exam, magnetic resonance imaging (MRI) and plain films. She presented to us after finishing her course of antibiotics with continued pain to evaluate for multifocal osteomyelitis.
Imaging findings
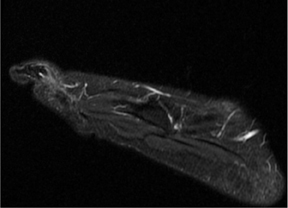
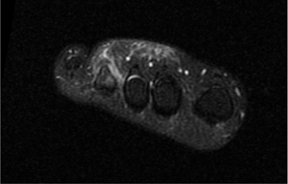
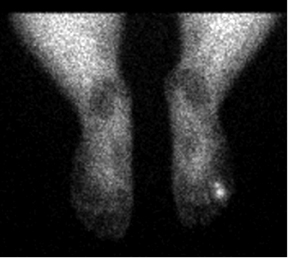
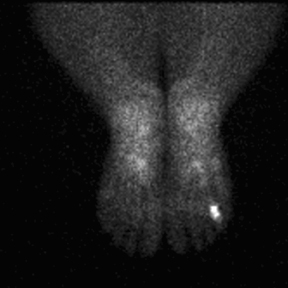
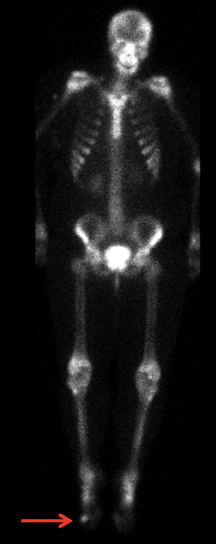
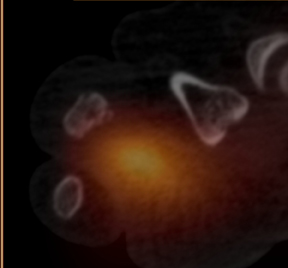
MRI of the right foot prior to bone scan demonstrated edematous soft tissue of the dorsal mid- to distal-foot extending to the soft tissue of the fourth toe (Figure 1). The proximal phalanx of the fourth toe as well as surrounding edema enhanced post-contrast. Findings were consistent with osteomyelitis with cellulitis. Plain films demonstrated normal bones, soft tissues, and joint spaces. A three-phase bone scan demonstrated hyperemia to the right forefoot with focal uptake on the delayed image (Figure 2). High-resolution single photon emission computed tomography and computed tomography (SPECT/CT) was then performed, demonstrating intense focal uptake in the proximal right fourth toe corresponding to a nondisplaced fracture in the distal aspect of the right fourth proximal phalanx (Figure 3).
Diagnosis
Osteomyelitis with associated nondisplaced fracture in right proximal phalanx
Discussion
Osteomyelitis is an infection of the bone and bone marrow. Pediatric osteomyelitis is generally considered rare. In the pediatric population, hematogenous route of infection is the most common route of infection.1 Imaging this infection can be problematic, particularly in the pediatric population. Multiple imaging modalities are being used in the workup of children with known or suspected osteomyelitis. Radiographs are often negative or inconclusive early in the development of the disease.2 Skeletal scintigraphy detects physiological changes as low as 5% in bone turnover, whereas x-ray requires a 30% to 50% loss of bone mineralization before morphological changes can be detected.2 Furthermore, skeletal scintigraphy is positive as early as the first 24 hours after the onset of symptoms.3 MRI typically has higher sensitivity than CT in detecting osteomyelitis and has the advantage of defining the extent of infection and associated soft-tissue changes. However, CT has the advantage of providing images with high spatial resolution and superb cortical bone details.4 In addition, MR imaging in pediatrics has additional limitations, including increased time for imaging and susceptibility to metal artifacts.5
Chronic recurrent multifocal osteomyelitis is a rare condition that affects multiple bones.6 The multifocal nature of such a condition requires whole-body imaging. Skeletal scintigraphy provides a whole-body evaluation with high sensitivity, but with variable specificity. In addition to the lack of anatomic localization, there is an inherent limitation to such a technique. Employing SPECT/CT is better than employing CT or SPECT alone. The CT component of the SPECT/CT is typically used for lesion localization and for attenuation correction. The high-resolution image acquisition feature of the BrightView SPECT/CT provides a unique opportunity and value to the field of musculoskeletal imaging. It provides a superb, sub-mm (0.33 mm) evaluation of skeletal anatomy. The availability of such technology may improve our ability to characterize lesions and may affect treatment decisions and patient management.
Conclusion
High-resolution SPECT/CT provides the additional information of bone detail, which may otherwise be unapparent in other imaging modalities. In this case, a fracture in the fourth toe was identified on SPECT/CT and not apparent on MRI or plain film. The detection of such fracture explained the patient’s right foot pain.
References
- Mader JT, Shirtliff M, Calhoun JH. The host and the skeletal infection: Classification and pathogenesis of acute bacterial bone and joint sepsis. Best Pract Res Clin Rheumatol. 1999;13:1-20.
- Saigal G, Azouz EM, Abdenour G. Imaging of osteomyelitis with special reference to children. Semin Musculoskelet Radiol. 2004;8:255-265.
- Maurer AH, Chen DCP, Camargo EE, Wong DF, et al. Utility of three-phase skeletal scintigraphy in suspected osteomyelitis: Concise communication. J Nucl Med. 1981;22:941-949.
- Pineda C, Vargas A, Rodríguez AV. Imaging of osteomyelitis: Current concepts. Infect Dis Clin North Am. 2006;20:789-825.
- Vijayanathan S, Butt S, Gnanasegaran G, Groves AM. Advantages and limitations of imaging the musculoskeletal system by conventional radiological, radionuclide, and hybrid modalities. Semin Nucl Med. 2009;39:357-368.
- Kothari NA, Pelchovitz DJ, Meyer JS. Imaging of musculoskeletal infections. Radiol Clin North Am. 2001;39:653-671.