Optimizing Monitoring of Pulmonary Airway Interventions With Digital Tomosynthesis
Introduction
With its wide availability, low cost, and low radiation dose, the chest radiograph remains the most performed radiographic procedure worldwide. Despite its ease of use, the chest radiograph has diagnostic limitations. The 2D planar acquisition of the chest radiograph limits the spatial delineation of the complex 3D structures within the thorax. The wide latitude and dynamic range of the chest radiograph can also preclude the differentiation of the complex tissue pathologies contained within the thorax.1
More recent advances in the detection of cardiothoracic disease have been made possible with the incorporation of flat-panel detector technology in chest radiography. The flat-panel detector enables several advances: it improves contrast independent of exposure level, the availability of image data in electronic form, and the ability to acquire multiple images in rapid sequence.1 Sequential image acquisition capability made possible with flat-panel detectors has enabled 2 important technologies in chest radiography: dual-energy subtraction radiography and digital tomosynthesis.
While first proposed as a technology in the 1950s, dual-energy radiography was only first performed in the 1980s.2 Early literature with dual-energy radiography demonstrated improved detection of lung nodules compared with conventional radiography.3 Utilizing flat-panel technology, dual-energy subtraction was enabled with a sequential dual exposure of high- and low-energy x-ray acquisitions.4 Dual-energy radiography has also been reported to better delineate calcified from noncalcified structures.5 This improved delineation has also enabled a better depiction of a large range of calcified cardiovascular structures.6
The rapid sequential acquisitions made possible with flat-panel technology have more recently enabled the adoption of another advanced imaging technique, digital tomosynthesis. This advanced application has demonstrated improved detection of breast cancer,7 orthopedic pathology,8 and urological imaging.9 In the thorax, digital tomosynthesis has demonstrated improved pulmonary nodule detection.10 Further reports have compared pulmonary nodule detection between conventional radiography, dual-energy radiography, and digital tomosynthesis. Digital tomosynthesis demonstrated clearly superior performance compared with dual-energy and conventional acquisitions.11 Simultaneously, chest tomosynthesis has the radiation dose equivalent of 2 posteroanterior and lateral x-rays; therefore, the average dose of a digital tomosynthesis examination is 0.3-0.4 mSv. Compared with a diagnostic chest CT, typically 4-8 mSv, the average chest digital tomosynthesis dose is 5%-10% that of a diagnostic chest CT.
Advancements in dual-energy radiography and digital tomosynthesis have also further improved visualization and evaluation of the airways.12, 13 The focus of this review is the enhanced capabilities of digital tomosynthesis in the assessment of suspected airway disease. In addition to effectively detecting airway stenosis, digital tomosynthesis proves valuable in the evaluation and management of patients with suspected airway disease, including the improved detection of airway stents and endobronchial valves (EBV).
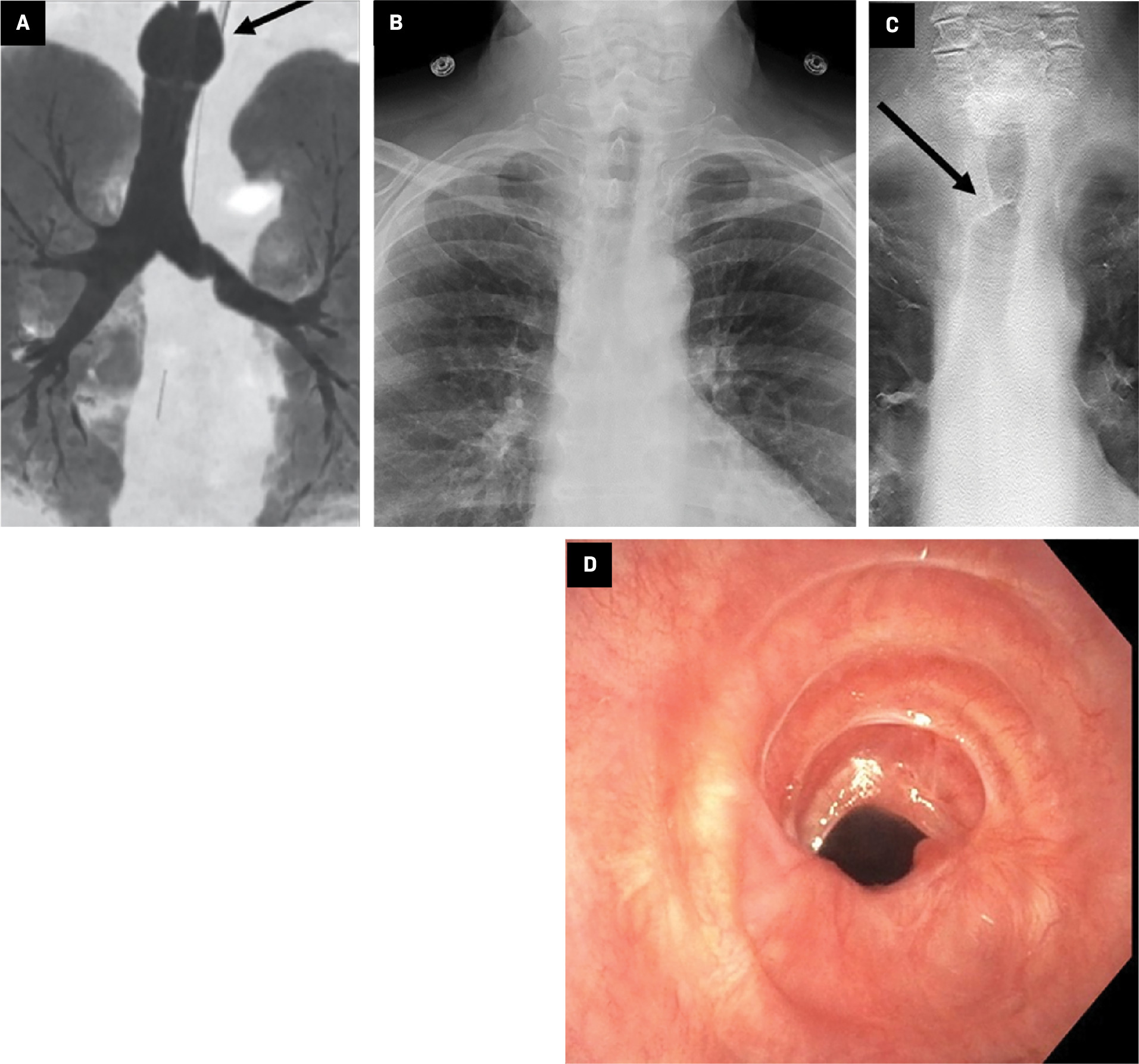
Postintubation Tracheal Stenosis
During the peak of the COVID-19 global pandemic, reports from regions that were more profoundly affected by COVID-19 found that up to 88% of critically ill patients with COVID-19 required endotracheal intubation for a median of 18 days.14 The complications of prolonged or repeated intubation and endotracheal cuff overinflation have been well documented, including tracheal ischemia, ulceration, and necrosis.15 Such tracheal injury can lead to tracheal stenosis, resulting in chronic or progressive respiratory symptoms after extubation. Treatment options for tracheal stenosis include endoscopic balloon dilation and open surgery with partial tracheal resection and anastomosis. Mattioli et al highlighted the advantage of balloon dilation in patients with COVID-19 over the more invasive approach of open surgery.16 After treatment, patients undergo serial endoscopic examinations to assess patency and integrity of their airways. Diagnostic imaging has a role in assessing the airway in the periprocedural setting, both for the detection of tracheal stenosis, preprocedural planning, and postprocedural follow-up. Cross-sectional imaging with CT is often used to assess the severity of tracheal stenosis and is complementary to the more definitive but invasive diagnostic approach of direct endoscopic evaluation. Additionally, the use of dynamic CT and MRI has been described for further characterizing tracheal stenosis.17 However, digital tomosynthesis can be valuable in this setting, particularly when cross-sectional imaging is not available ( Figure 1 ).
Malignant Bronchial Stenosis
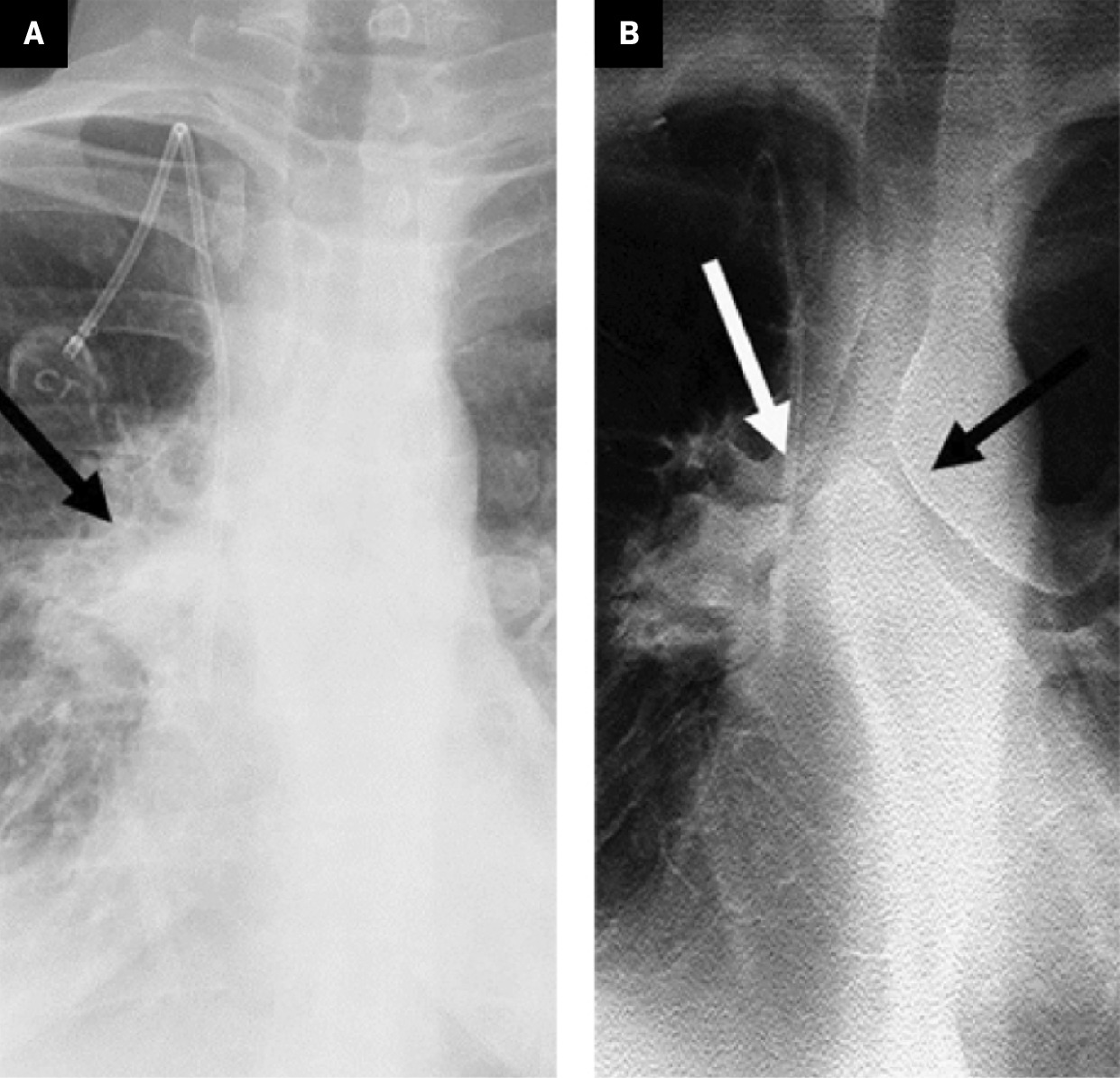
Central airway stenting is a common, minimally invasive interventional pulmonary procedure performed to maintain airway patency in patients with malignant airway pathologies, including tumor invasion into the airway lumen, as well as extrinsic mass compression of the airway.18 While not curative, airway stenting relieves symptoms and improves the quality of life for the patient. Conventional radiography is often the initial imaging requested to assess the thoracic anatomy. However, due to overlapping mediastinal anatomic structures, conventional radiographs have a relatively low sensitivity for detecting central airway pathology, often resulting in suboptimal evaluation of the airways.19 Digital tomosynthesis provides an alternative or intermediate step in detecting malignant airway stenosis and determining the integrity of the airways ( Figure 2 ). Studies evaluating inter-reader diagnostic performance found increased sensitivity and accuracy for detecting airway pathologies using digital tomosynthesis over conventional radiography.13
Adult with malignant bronchial stenosis. Chest radiograph (A) demonstrates an irregular, lobular, mass-like density projecting over the right perihilar region (arrow). Note the limited visualization of the mainstem and segmental bronchi secondary to underpenetration. Digital tomosynthesis (B) improves visualization of underlying severe stenosis of the right-sided tracheobronchial structures (white arrow). There is moderate stenosis of the left mainstem bronchus (black arrow).
Postoperative Airway Complications
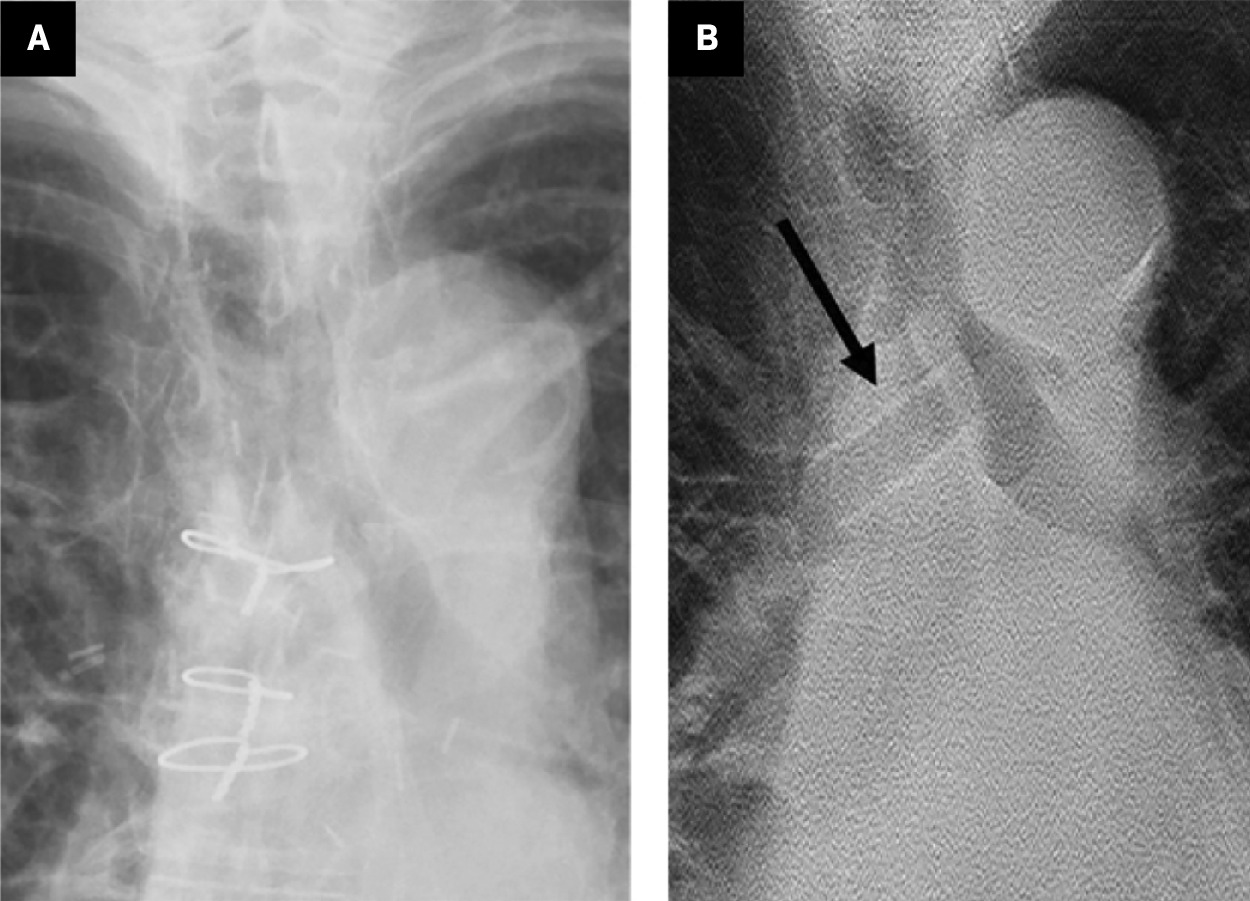
Lung Transplantation
Patients with end-stage lung disease undergo an extensive assessment of transplant eligibility prior to receiving a lung transplant. Radiologists are becoming increasingly more involved in the care of these patients both before and after transplantation. In addition to assessing post-transplant infection or sequelae of transplant rejection, assessing the airway anastomosis site is critical. Central airway stenosis at the anastomotic site between the donor and recipient mainstem bronchi is one of the common post-transplant complications.20 Placement of an airway stent is an important treatment option for post-transplant anastomotic strictures. However, complications may occur after the stent is placed, and follow-up imaging can help assess the possibility of stent migration and/or obstruction ( Figure 3 ). In 1 series, stent-related complications were seen in 23% to 34% of patients.21 In another study by Kim et al, evaluating patients undergoing airway stent placement, 47% required 2 or more procedures, with stent-related complications occurring in the first 2 to 3 months after the initial procedure.22 Digital tomosynthesis can change the treatment plan without the need for additional CT imaging.23
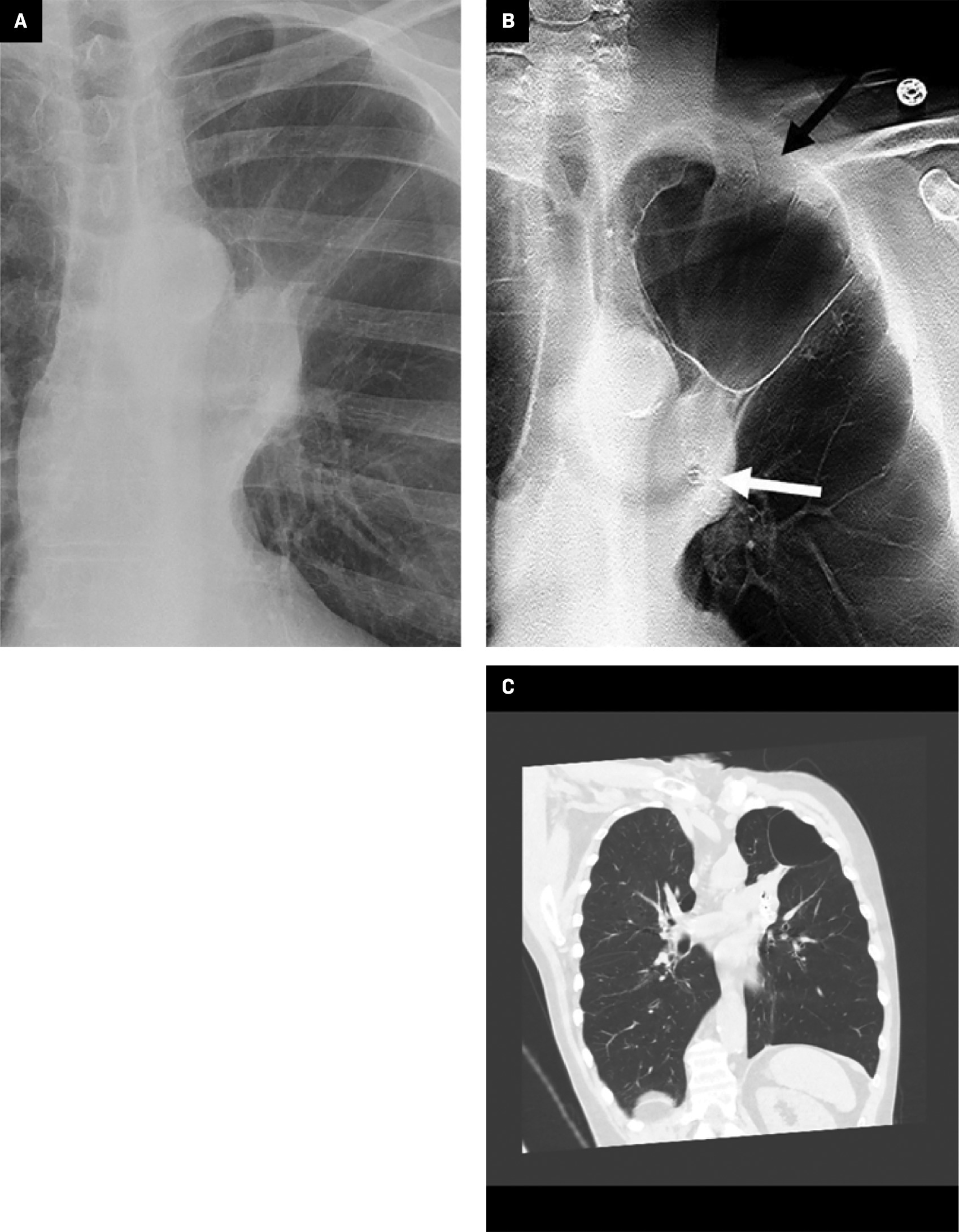
Endobronchial Valve Placement
Patients with refractory chronic obstructive pulmonary disease (COPD) owing to severe lung hyperinflation and air trapping may benefit from minimally invasive procedures, which aim to selectively reduce lung volume, improve lung function, and relieve symptoms. In fact, the placement of an EBV is a standard-of-care treatment option for advanced COPD in many countries.24 After placement of an EBV, serial imaging follow-up is necessary to assess lung volume changes in addition to postprocedural complications. A pneumothorax is a common complication, with some reporting a 15% to 25% occurrence rate.24 However, making the distinction between a bulla or pneumatocele, which has been shown to resolve on its own,25 and a pneumothorax, for which the valves may need to be removed, may impact the patient’s clinical and treatment course. Conventional radiography may not have the resolution to definitively visualize the thin-walled cyst of a pneumatocele.26 However, by scrolling through slices provided by digital tomosynthesis, the outline of the pneumatocele can be better appreciated ( Figure 4 ).
Adult with chronic obstructive pulmonary disease following left upper lobe EBV placement. Conventional chest radiograph (A) following left upper lobe EBV placement. Postprocedural digital tomosynthesis image (B) following EBV placement enhances demonstration of left apical lucency consistent with postprocedural pneumatocele (black arrow). Note improved visualization of the EBV within the left upper lobe airways (white arrow). Coronal chest CT reformation (C) following EBV placement confirms the digital tomosynthesis diagnosis of postprocedural pneumatocele.
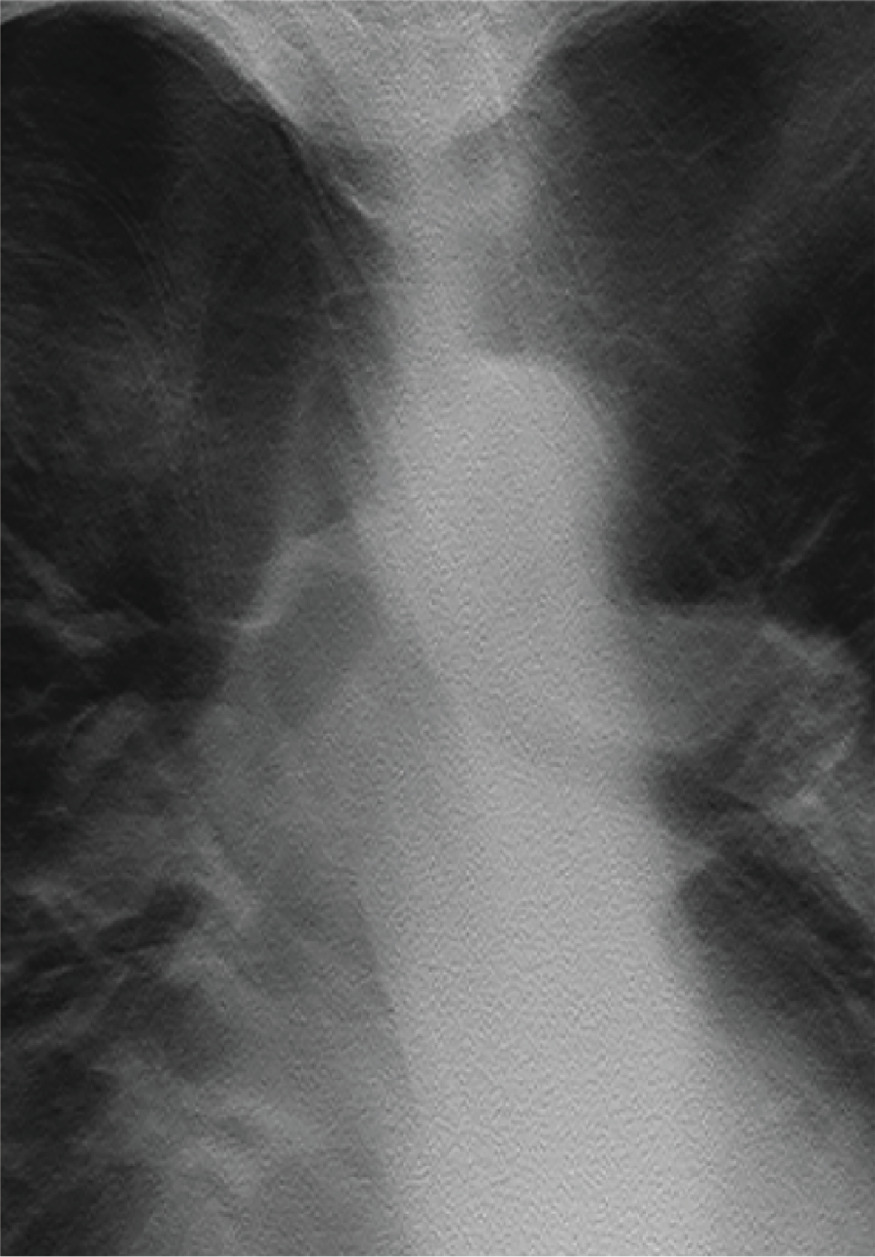
Limitations of Digital Tomosynthesis in Thoracic Imaging
The diagnostic value and added benefit of digital tomosynthesis in the monitoring of patients with a variety of airway pathologies and airway interventions are clear. However, digital tomosynthesis technology has limitations. Current digital tomosynthesis platforms are not portable, precluding their use in the intensive care unit setting. Additionally, blurring artifact may occur in patients who have difficulty cooperating with the examination, given that the acquisition requires a 10-second breath hold ( Figure 5 ); however, we are not aware of specific literature indicating a significant rate of nondiagnostic digital tomosynthesis examinations.
Limitations of digital tomosynthesis. Digital tomosynthesis centered over the trachea and central airways shows blurring artifact owing to patient motion during the acquisition. As a result, there is poor delineation of the contour and luminal integrity of the trachea and central airways.
Conclusion
The expanding scope and advances in the field of interventional pulmonology have paralleled the growth of advanced imaging techniques to better evaluate the results of interventions, including removable silicone stents,27 balloon/laser ablation,28 and EBV therapy,29 and have increased the opportunity for accurate, noninvasive monitoring of these interventions.
These technological advances are not without their own complexities, and patients undergoing airway intervention commonly return for follow-up evaluation for complications. Due to the inherent limitations of standard film-screen and digital radiographic techniques, CT has been used to monitor the preprocedural and postoperative appearance of interventional pulmonology techniques.30 While the rapid acquisition and advanced 3D capabilities of modern-day CT have clear advantages, digital radiographic technologies, with significantly lower cost and radiation dose, offer a potentially attractive alternative for the patient with suspected airway disease.13, 31
In patients undergoing silicon stent placement, digital tomosynthesis demonstrated clear superiority to conventional radiography in the detection of these stents and associated complications.22 Recent experience demonstrates the significant diagnostic value of digital tomosynthesis in the post-lung transplant patient with endobronchial stents.
Additional opportunities for therapy monitoring with digital tomosynthesis exist in patients undergoing EBV therapy. Well-recognized complications in patients include postprocedural pneumothoraces, EBV migration, and airway granulation/stenosis.32 Early results suggest digital tomosynthesis may also improve pneumothorax detection in patients undergoing EBV therapy.33
Digital tomosynthesis has advantages over plain radiography in the detection of airway disease, and its role in the effective, low-cost and low-radiation-dose monitoring of these therapies. Future advances in pulmonary intervention will continue to define the important role of digital tomosynthesis in this growing population.
References
Citation
L H, S S, B Y, NS H, L Y, K T, J S, V U, R G, A G,. Optimizing Monitoring of Pulmonary Airway Interventions With Digital Tomosynthesis. Appl Radiol. 2024;(4):20 - 26.
doi:10.37549/AR-D-24-0024
August 1, 2024