Neuroblastoma, Stage MS
Images
Case Summary
An infant was born at 35 weeks’ gestation after in utero imaging revealed a possible cystic lung lesion. On the second day of life, an abdominal ultrasound had shown a 3.1 cm right suprarenal mass that was interpreted as an intraabdominal extra-lobar pulmonary sequestration. After a surgical consult the patient was scheduled for follow-up at 2 months of age, but imaging was not performed at that time.
On physical exam at 4 months of age, the patient was noted to have an enlarged and firm liver and an ultrasound exam was performed.
Imaging Findings
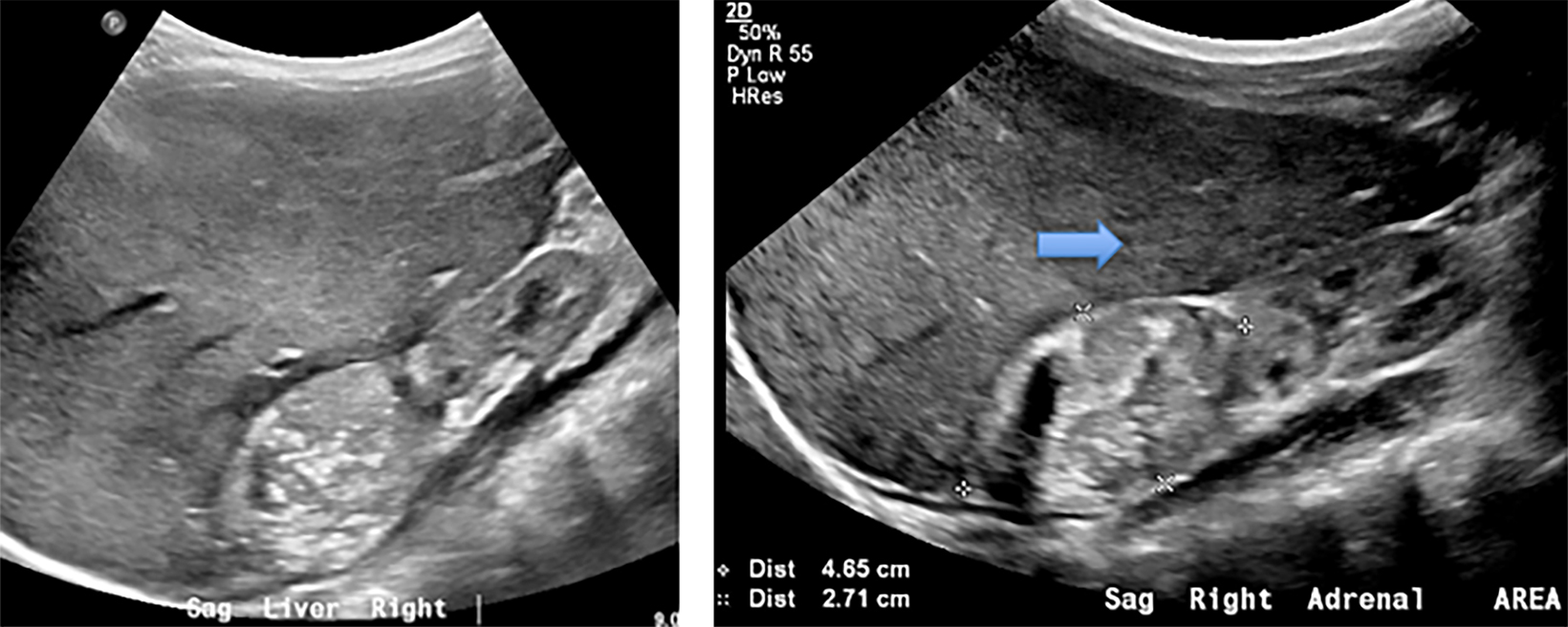
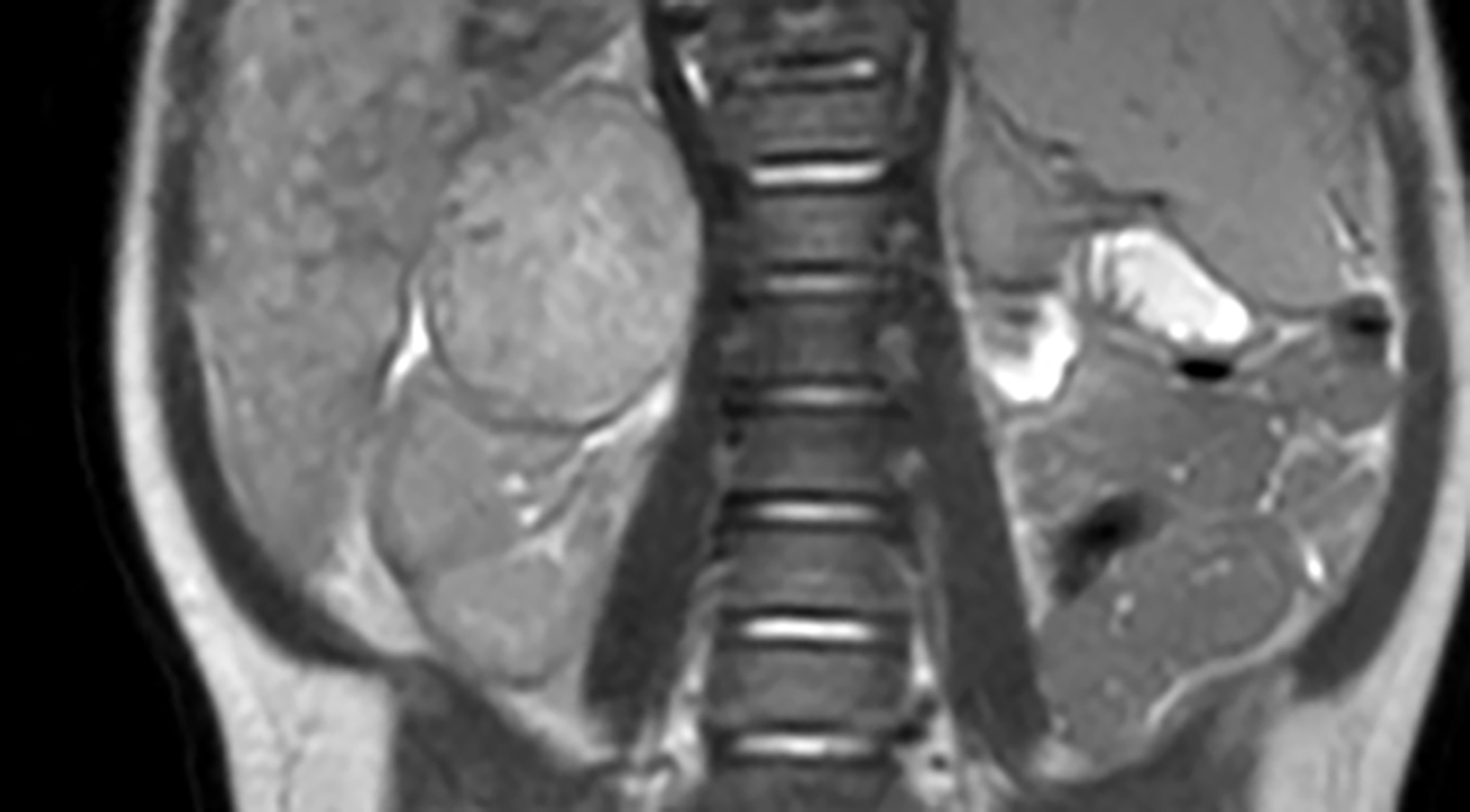
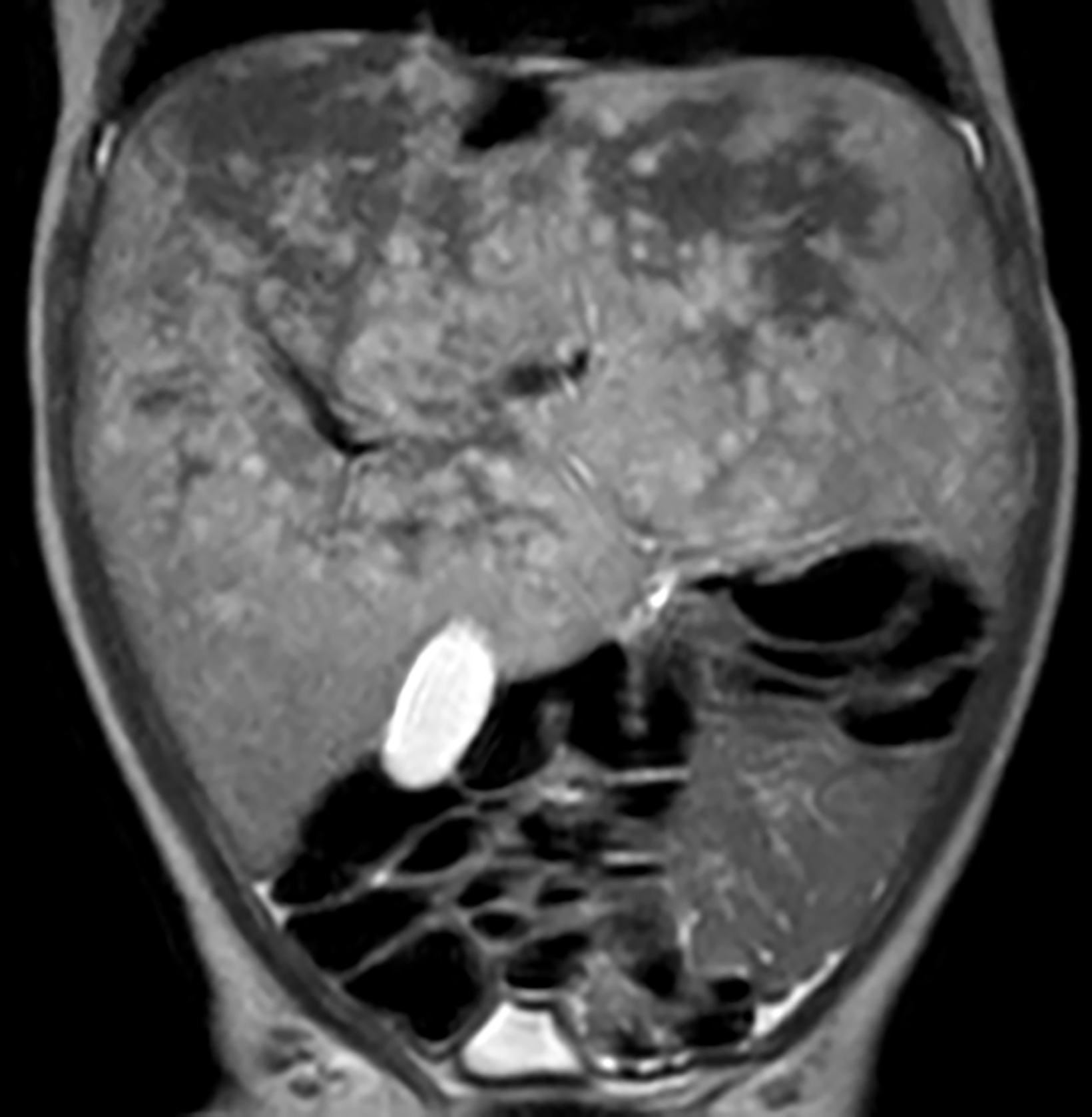
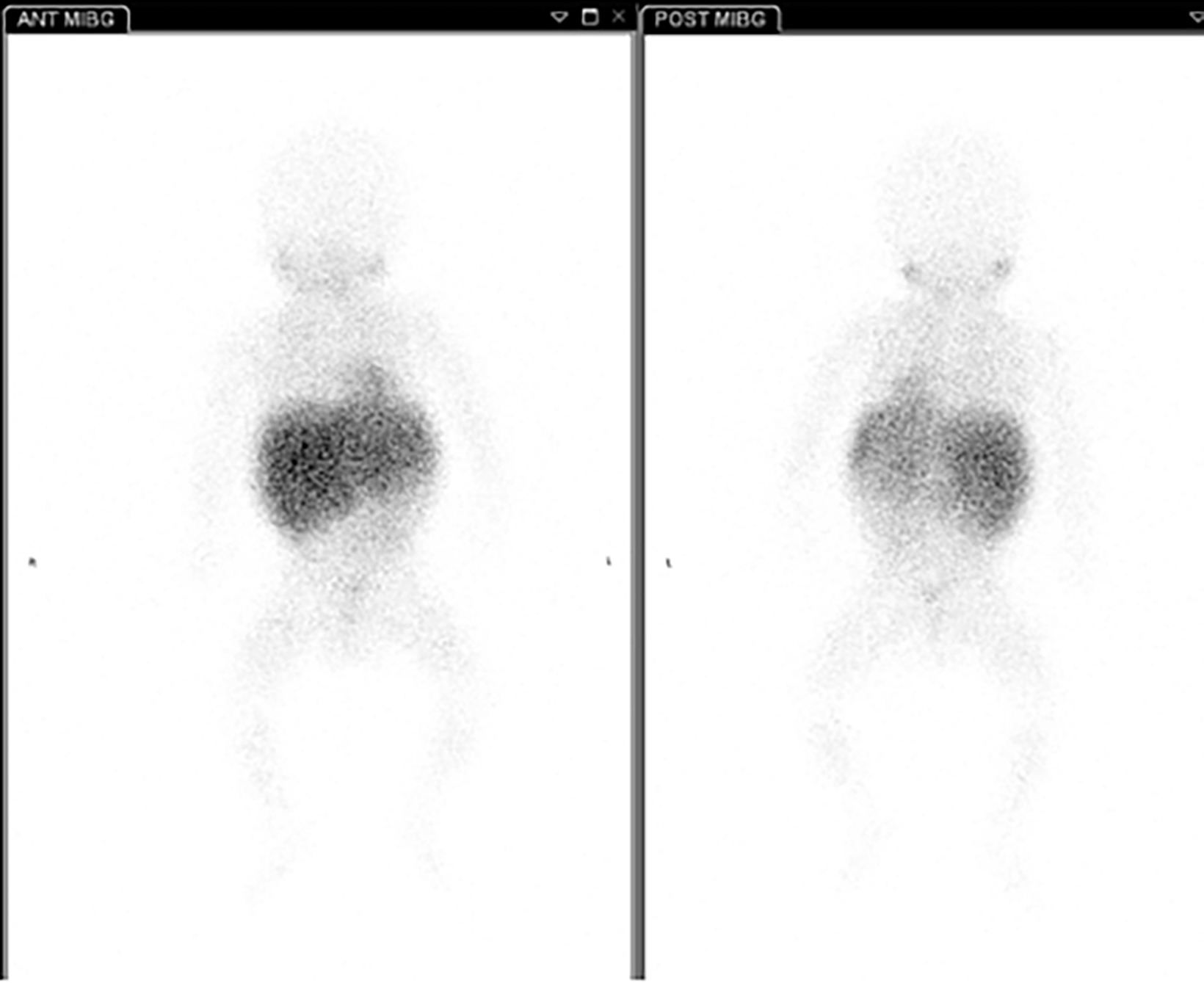
Abdominal ultrasound (Figure 1) performed at 4 months of age showed an enlarged and heterogeneous liver with a 4.7 cm heterogeneous, solid, suprarenal mass with internal echogenic foci consistent with calcifications. Subsequent MRI of the abdomen and pelvis (Figure 2) showed numerous liver metastases. The right adrenal mass had a heterogeneous but relatively hyperintense appearance on T2 weighted imaging but relatively hyperintense. An enlarged para-aortic lymph node was present. A metaiodobenzylguanidine (MIBG) scan (Figure 3) revealed heterogeneous radiotracer uptake in the liver but no uptake in the suprarenal mass and ultrasound-guided percutaneous biopsy was performed.
Diagnosis
Neuroblastoma, stage MS
Discussion
Neuroblastomas are a neoplastic proliferation of neural crest cells within the sympathetic chain. While they most commonly arise within the adrenal gland, they can occur anywhere along the sympathetic chain, including in the neck, chest, abdomen, and pelvis.1 Neuroblastomas are the most common extracranial solid malignancy in children, accounting for roughly 6-10% of cancers.2
The International Neuroblastoma Risk Group Staging System (INRGSS) provides a clinical staging of neuroblastoma.3 This staging system differs from the previously used International Neuroblastoma Staging System (INSS), which was a postsurgical staging system. The INRGSS uses image-defined risk factors (IDRFs) to determine whether the disease is localized without involving vital structures (L1) or if it is a locoregional tumor with the presence of IDRFs (L2). The presence of distant metastatic disease leads to a classification of stage M. There is a special stage of neuroblastoma termed MS. This represents metastatic disease in children younger than 18 months with metastatic disease confined to the skin, liver, and/or bone marrow.
Stage MS neuroblastomas, which account for 7-10% of neuroblastoma cases, often have favorable outcomes; survival rates are estimated to be 70-90%.4 This contrasts with stage M, which has a survival rate of 30-40%. This difference is likely due to spontaneous regression, a unique characteristic of stage MS neuroblastomas. Certain factors are associated with poorer outcomes with stage MS neuroblastomas. They include N-MYC amplification, chromosomal abnormalities (such as the loss of chromosome 1p), diploidy, age at diagnosis of less than two months.4
While the tumors regress in most patients with stage MS disease, some patients can experience rapid progression of liver metastases. This can cause life-threatening compression of the lungs, kidneys, intestines, and inferior vena cava.5 The tumor can progress to true stage M disease prior to regression. This phenomenon should be differentiated from late-onset recurrent disease.
Children who present with a palpable abdominal mass are first imaged with ultrasound to determine the organ of origin. Features that help the radiologist make a presumptive diagnosis of neuroblastoma include a suprarenal location and foci of internal echogenicity related to tumoral calcification.6 Computed tomography or MRI is used to further evaluate the tumor and determine if any of 20 different IDRFs are present7. On CT and MRI, neuroblastomas present as heterogeneous masses with variable enhancement.8 MIBG scans are used to track radiotracer uptake from neuroblastomas at both the primary and distant sites.9
Treatment involves chemotherapy, resection, or radiotherapy. However, in stage MS neuroblastomas, most patients can be monitored with the expectation that the tumor will regress spontaneously.9 Radiotherapy may be used when hepatic metastases are present and inhibit respiratory function.8
Conclusion
Neuroblastoma is the most common extracranial solid malignancy in children. Stage MS tumors represent a unique, uncommon, variant that occurs exclusively in children younger than 18 months. Ultrasound is used initially to diagnose neuroblastoma and is followed by CT and/or MRI for staging, and MIBG scanning to determine extent of disease. Patients with stage MS neuroblastomas often are followed with surveillance with the expectation of spontaneous regression.
References
- Arendonk KV, Chung D. Neuroblastoma: tumor biology and its implications for staging and treatment. Children. 2019;6(1):12.
- Colon NC, Chung DH. Neuroblastoma. Adv Pediatr. 2011;58(1):297-311.
- Monclair T, Brodeur GM, Ambros PF, et al. The International Neuroblastoma Risk Group (INRG) Staging System: An INRG Task Force Report. J Clin Oncol. 2009;27(2):298-303. doi:10.1200/JCO.2008.16.6876.
- Taggart DR, London WB, Schmidt ML, et al. Prognostic value of the stage 4S metastatic pattern and tumor biology in patients with metastatic neuroblastoma diagnosed between birth and 18 months of age. J Clin Oncol. 2011;29(33):4358-4364.
- Tas ML, Nagtegaal M, Kraal KC, et al. Neuroblastoma stage 4S: Tumor regression rate and risk factors of progressive disease. Pediatric Blood & Cancer. 2019;67(4) e28061. doi: 10.1002/pbc.28061. Epub 2019 Nov 17.
- Kembhavi S, Shah S, Rangarajan V, Qureshi S, Popat P, Kurkure P. Imaging in neuroblastoma: An update. Indian J Radiol Imaging. 2015;25(2):129-136.
- Chen AM, Trout AT, Towbin AJ. A review of neuroblastoma image-defined risk factors on magnetic resonance imaging. Pediatr Radiol. 2018;48(9):1337-1347. doi: 10.1007/s00247-018-4117-9. Epub 2018 Aug 4.
- Papaioannou G. Neuroblastoma in childhood: review and radiological findings. Cancer Imaging. 2005;5(1):116-127.
- Sharp SE, Trout AT, Weiss BD, Gelfand MJ. MIBG in neuroblastoma diagnostic imaging and therapy. RadioGraphics. 2016;36(1):258-278.
References
Citation
AJ BRTRSCT. Neuroblastoma, Stage MS. Supplement to Applied Radiology . 2022;(5):3-5.
September 1, 2022