Neonatal Thymic Hemorrhage
Images
Case Summary
An infant presented with difficulty breathing and feeding. The patient had hyperbilirubinemia and bilious stools since birth and developed acute hypoxic respiratory failure. These signs were related to a large mediastinal mass, severe metabolic lactic acidosis, anemia, acute severe coagulopathy, and hemorrhagic disease of the newborn, all due to vitamin K deficiency.
Laboratory serum analysis demonstrated low hemoglobin and high urine glucose levels. Thrombocytopenia was also present (110 K/µL). These were followed-up with x-ray, CT, MRI, and ultrasound to help determine the etiology of the mediastinal mass.
Imaging Findings
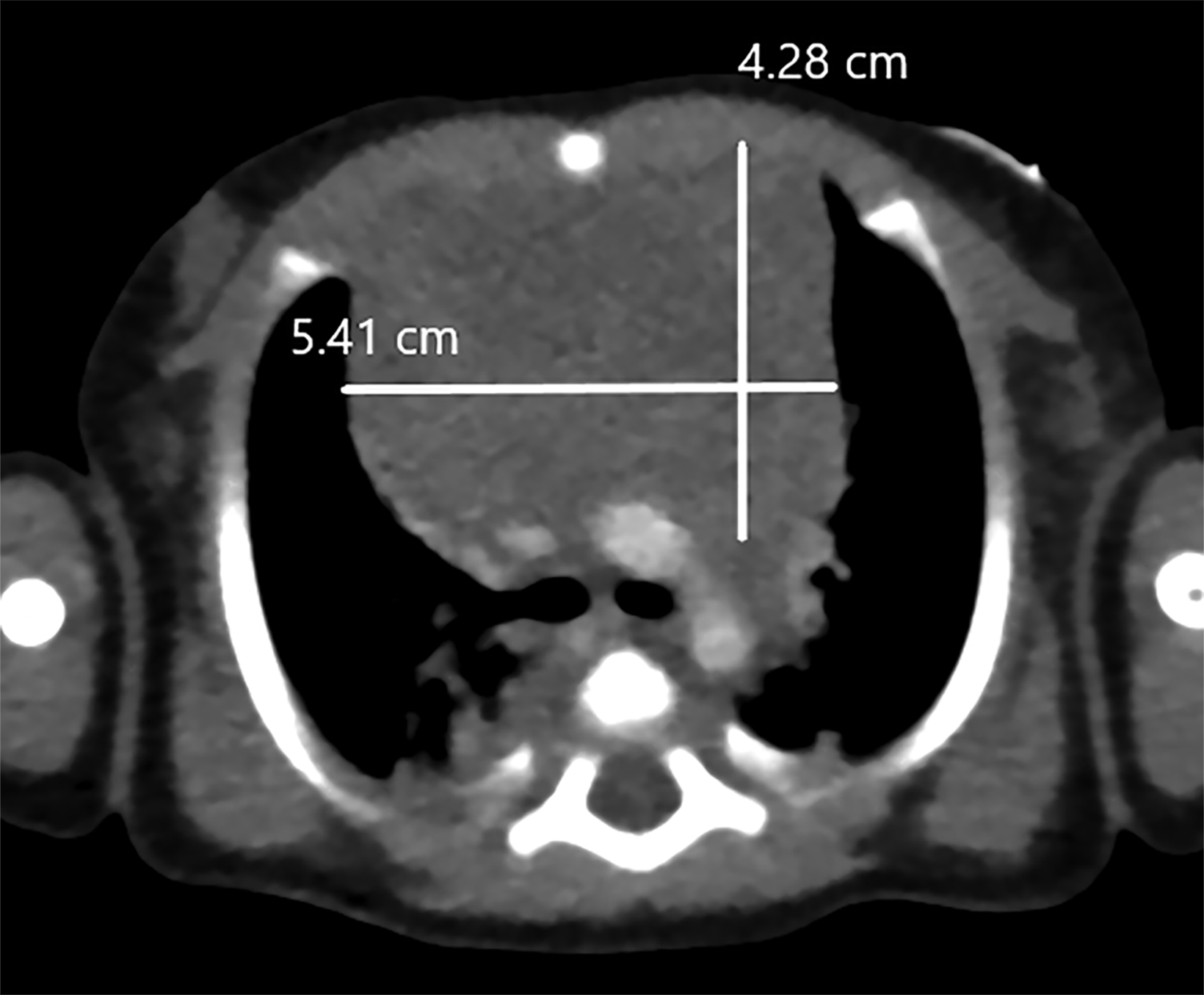
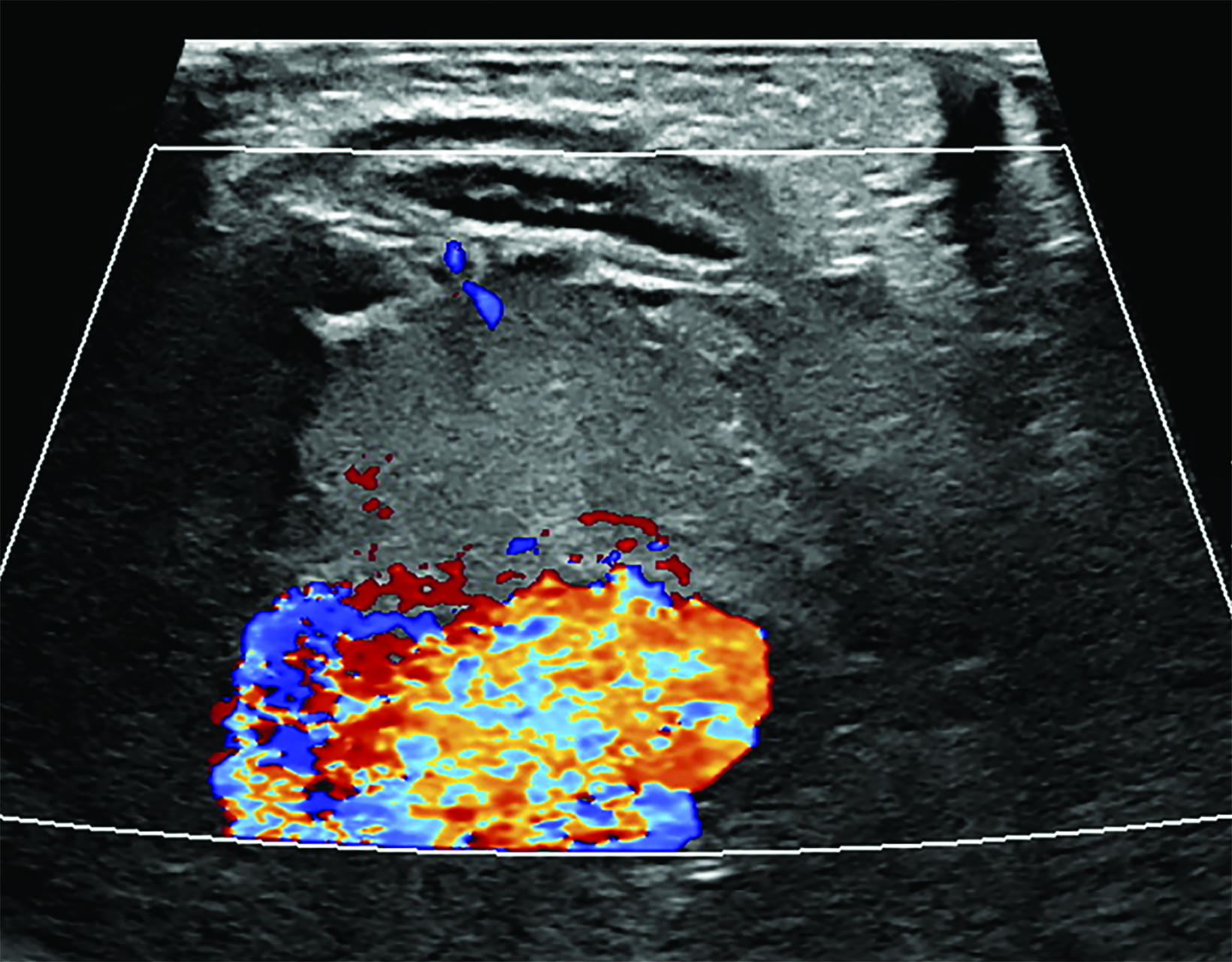
Contrast-enhanced chest CT (Figure 1) demonstrated an anterior mediastinal mass measuring 4.3 × 5.4 cm, exerting pressure on the heart and left brachiocephalic vein with mildly prominent bilateral lymph nodes. Doppler ultrasound of the chest (Figure 2) did not demonstrate blood flow within the lesion.
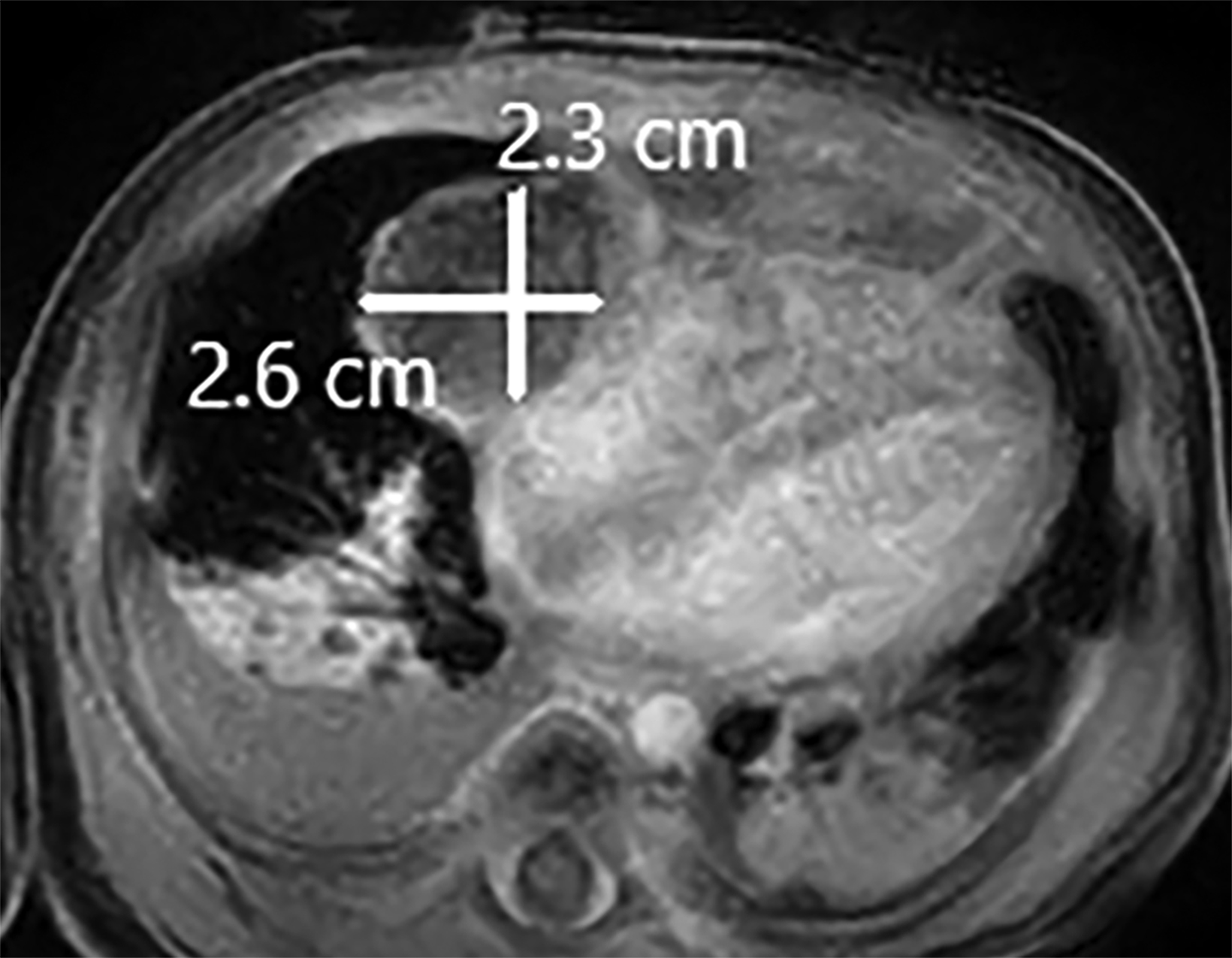
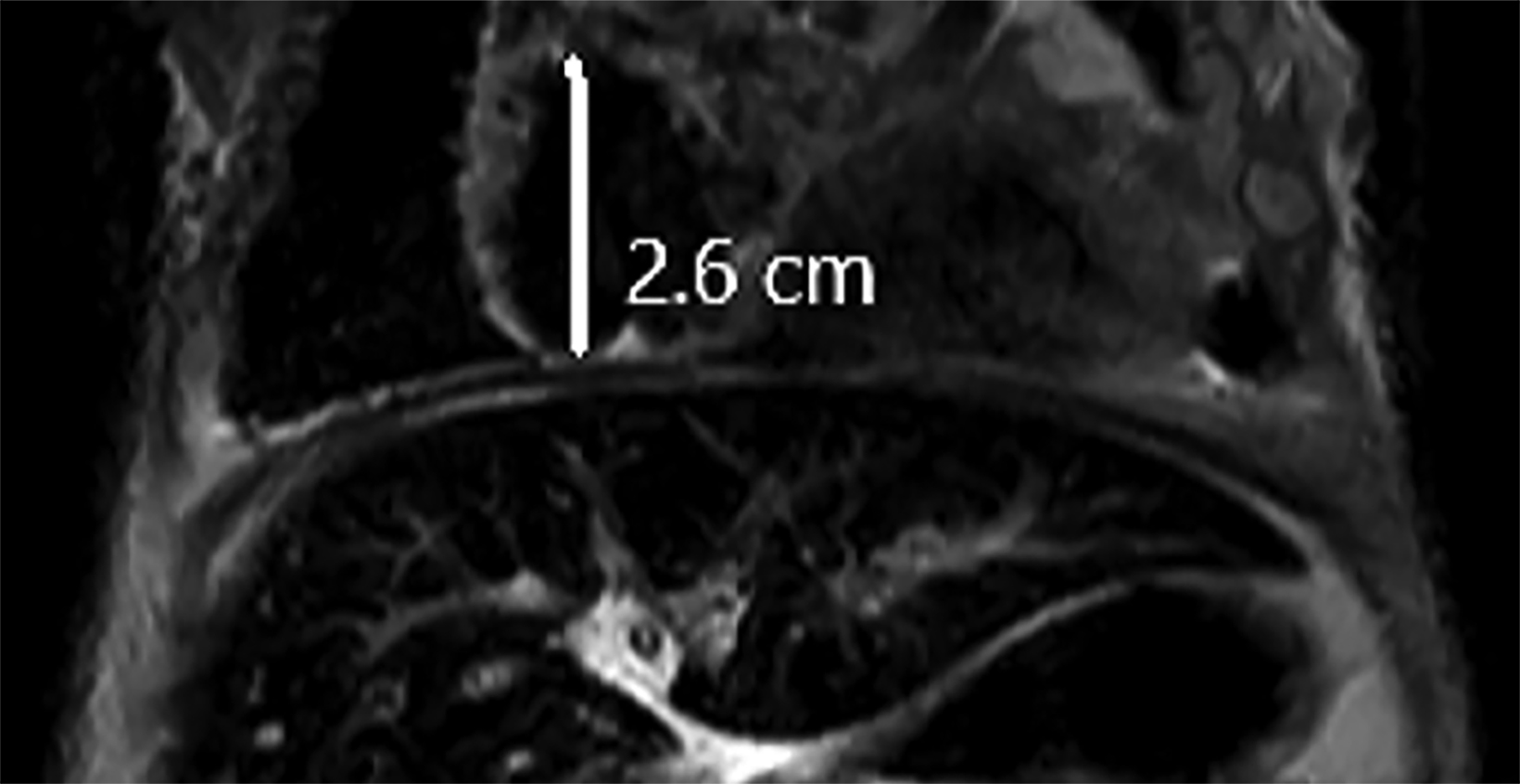
Contrast MRI of the chest/abdomen (Figure 3) demonstrated the crescent-shaped mediastinal mass measuring 4.1 × 3.8 × 1.0 cm anterior to the thymus and heart. A T1 precontrast coronal image of the infant’s thoracoabdominal region (not shown) demonstrated mild hyperintensity, but no significant contrast enhancement. T2 images showed hypointense signal.
Diagnosis
Neonatal thymic hemorrhage.
Differential diagnosis of mediastinal mass lesions in neonates includes thymoma, thymic carcinoma, lymphoma/lymphadenopathy, thyroid mass, and germ-cell neoplasm.
Discussion
Thymic hemorrhage is defined by extravasated erythrocytes in the thymic parenchyma. In neonates, this commonly results from diet and vitamin K deficiency but is also possible from trauma.1 Reported cases of thymic hemorrhage in newborns have presented with respiratory distress, pleural effusion, mediastinal mass lesions, anemia, and vitamin K deficiency.2,3
Vitamin K deficiency is common in newborns, owing to limitations in transplacental passage of vitamin K and only trace amounts of the vitamin present in breast milk. A prolonged deficiency may cause complications such as Vitamin K deficiency bleeding (VKDB),4 which is commonly secondary to preexisting bleeding disorders.5
A typical dose of vitamin K prophylaxis administered intramuscularly at birth aids in addressing the deficiency. However, out-of- hospital births, concerns among parents about the injection, and anti-vaccination sentiment can sometimes lead to refusal of prophylaxis, as in this case.6
Denial of prophylaxis in this patient potentially resulted in poor Vitamin K-dependent coagulation factors, which subsequently caused coagulopathy and jaundice, two symptoms of VKDB.7 On the third day after the neonate’s admission to the hospital, the hematology service recommended administration of 2.5 mg of vitamin K supplementation daily. X-ray imaging approximately one month days after admission demonstrated resolution of the mediastinal mass, confirming the diagnosis of thymic hemorrhage mimicking a mass.
The etiology and pathognomonic sequelae of thymic hemorrhage are obscure, but many signs indicate the condition. Respiratory distress in newborns is one initial sign.2,3 The most prevalent imaging sign is a mediastinal mass. These lesions are commonly misinterpreted as tumors, owing to their infrequency. Distinguishing a hematoma from a malignancy can be achieved through cross-sectional imaging and short-interval follow-up to ensure lesional resolution.
Lack of k-dependent coagulant proteins from vitamin K deficiency may restrict clotting and cause increased blood loss in atypical regions, including the thymus. Bleeding can also occur intrathoracically, intracranially, and in the abdominal cavity among other locations.7
If an infant presents with a large thymic mass due to a potential hemorrhage, determining whether they received vitamin K supplementation at birth is critical as a thymic mass is more likely to be of hemorrhagic etiology if no prophylaxis was administered.
Laboratory results also support the diagnosis under the above circumstances. Low hemoglobin, blood glucose, lymphocyte, and platelet levels, as well as signs of anemia, all demonstrate potential hemorrhage. Thymic bleeding may cause these deficiencies.
Conclusion
Neonatal thymic hemorrhage is an exceedingly rare condition that requires investigation of the etiology. Imaging can help elucidate the etiology of the thymic lesion, particularly with blood-sensitive MRI sequences in the appropriate clinical setting.
References
Citation
JA W, GreerJB, L N, AR G, SB D.Neonatal Thymic Hemorrhage. Appl Radiol. 2023; (3):38-39.
May 5, 2023