Multinodular and Vacuolating Neuronal Tumor
Case Summary
An adult presented with a 1-year history of intermittent nonfocal headaches. Physical examination was unremarkable. Routine laboratory investigations were normal.
Imaging Findings
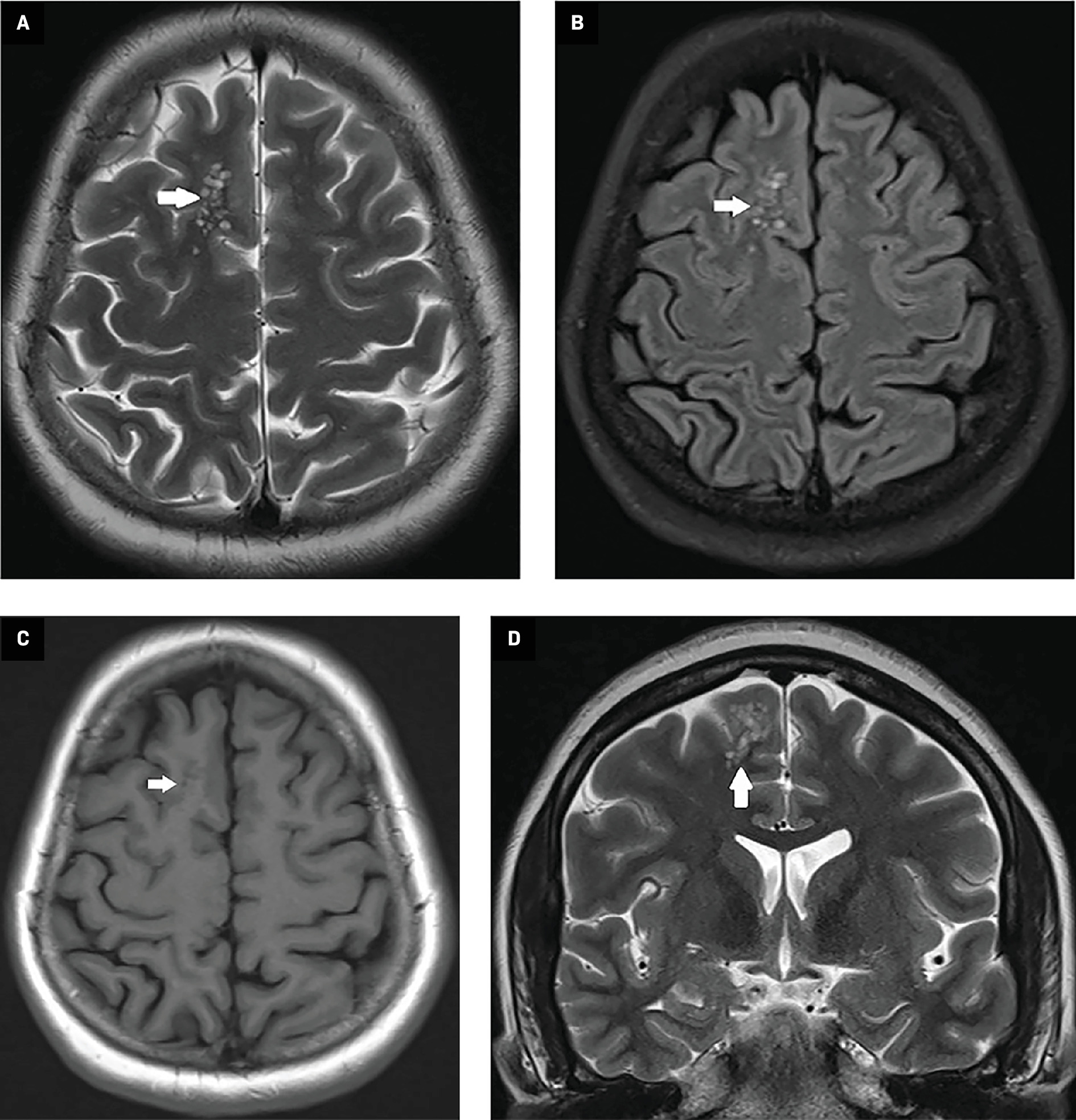
MRI of the brain ( Figure 1 ) revealed a cluster of multiple nodules in the gray-white matter junction and subcortical white matter in the right superior frontal gyrus. The nodules were hyperintense to gray matter on T2-weighted and FLAIR images, and iso-to-hypointense on T1-weighted images. No restriction was seen on diffusion-weighted images. No blooming was noted on susceptibility-weighted images. The nodules were coalescent, especially toward the gray-white matter junction. Neither mass effect nor contrast enhancement was noted. Based on MRI findings, a diagnosis of multinodular and vacuolating neuronal tumor (MVNT) was presumed, and the patient was offered symptomatic treatment. Follow-up MRI at 18 months later revealed a stable lesion.
Axial T2-weighted ( A ) and FLAIR ( B ) MR images demonstrate a cluster of hyperintense nodules (bubbles) in the subcortical white matter in the right frontal lobe (white arrows). The nodules appear iso-to-hypointense (white arrow) on T1-weighted image ( C ). Conglomeration of nodules toward the gray-white matter junction (white arrow) is seen on coronal T2-weighted image ( D ). Note the absence of mass effect.
Diagnosis
Multinodular and vacuolating neuronal tumor.
Differential diagnosis includes dysembryoplastic neuroepithelial tumor (DNET) and enlarged perivascular spaces.
Discussion
Multinodular and vacuolating neuronal tumor was first described by Huse et al1 in 2013 as a non-neurocytic, seizure-associated tumor in 10 patients. The entity was subsequently included as a new cytoarchitectural pattern in the 2016 update of the World Health Organization (WHO) classification of tumors of the central nervous system.2 This pattern was thought to be malformative and related to ganglion cell tumors.
In the 2021 classification,3 this entity is included in WHO grade 1 glioneuronal and neuronal tumors. Genetic alterations in the mitogen-activated protein kinase pathway are found in these tumors.
Multinodular and vacuolating neuronal tumors are usually found in adults, with a mean age at presentation of 38-44 years.4 - 7 Most cases present with headache (usually nonfocal) or seizure, while some can be asymptomatic.4 - 7 The parietal lobe is most often involved, followed by the frontal lobe.
Histopathologically, these lesions show neuroepithelial cells arranged as nodules with conspicuous vacuolation. These dysplastic cells are in the deep portion of the cortex, gray-white matter junction, and subcortical white matter, and are oriented perpendicular to the cortical surface.4
Most lesions exhibit typical MRI features. They appear iso-to-hypointense on T1-weighted images and as clusters of well-circumscribed T2-weighted and FLAIR hyperintense nodules in subcortical white matter with or without involvement of overlying cortex.
The nodules demonstrate a “bubbly” appearance on T2-weighted images.4, 5 Abnormal white matter signal can surround these bubble-like lesions,4, 5 and mass effect is typically absent. The lesions demonstrate neither restricted diffusion nor paramagnetic susceptibility effect. Nunes et al4 noted one case demonstrating subtle focal contrast enhancement; otherwise, contrast enhancement has not been reported in MVNTs. The imaging features are in keeping with its nonaggressive nature.6
Typical MRI patterns help differentiate MVNTs from DNET, which are cortical lesions, often wedge-shaped with FLAIR hyperintense components and a multicystic appearance. On CT, the lesions may either not be seen or appear as hypodense.5
Biopsy is not required in MVNTs as characteristic MRI features are sufficient for diagnosis. Most lesions are managed conservatively as they are indolent. Surgical resection may be required where seizures or symptoms are attributable to the lesion.4 Surgical resection is generally curative.1
Conclusion
Multinodular and vacuolating neuronal tumors can usually be diagnosed via characteristic MRI features. Familiarity with these lesions may prevent unnecessary biopsy.
References
Citation
Patil PV, DNB. Multinodular and Vacuolating Neuronal Tumor. Appl Radiol. 2024;(6):39 - 41.
doi:10.37549/AR-D-24-0047
December 1, 2024