Multi-Tracer PET Personalizes Advanced Prostate Cancer Management
Images
A new whole-body multi-tracer PET imaging approach can accurately identify evolving subtypes of cancer cells within distinct metastases in the same prostate cancer patient. The new research, published in The Journal of Nuclear Medicine, reports these changing cancer cells found in different metastases from the same patient—known as intrapatient intermetastatic heterogeneity (IIH)—were detected in 83% of metastatic castration-resistant prostate cancer (mCRPC) patients. Understanding their characteristics can provide physicians with valuable insights for developing personalized treatment plans.
Advances in medicine now allow mCRPC patients to undergo several types of treatment targeting different cancer pathways. Multiple treatments, however, cause cancer cells to change, resulting in IIH. These changes to challenges in monitoring cancer treatment resistance, defining progression, and making therapeutic decisions.
“Prior to this study, evidence of IIH in prostate cancer was determined by biopsy from only a few metastatic sites, either late in the disease course or after rapid autopsy,” said Frédéric Pouliot, MD, PhD, FRCSC, clinician-scientist and associate professor in the department of surgery, urology division, at CHU de Québec–Université Laval Research Center in Quebec City, Quebec, Canada. “By using whole-body PET/CT to scan for IIH earlier, clinicians can integrate IIH knowledge in their treatment decisions, including radiopharmaceutical therapy.”
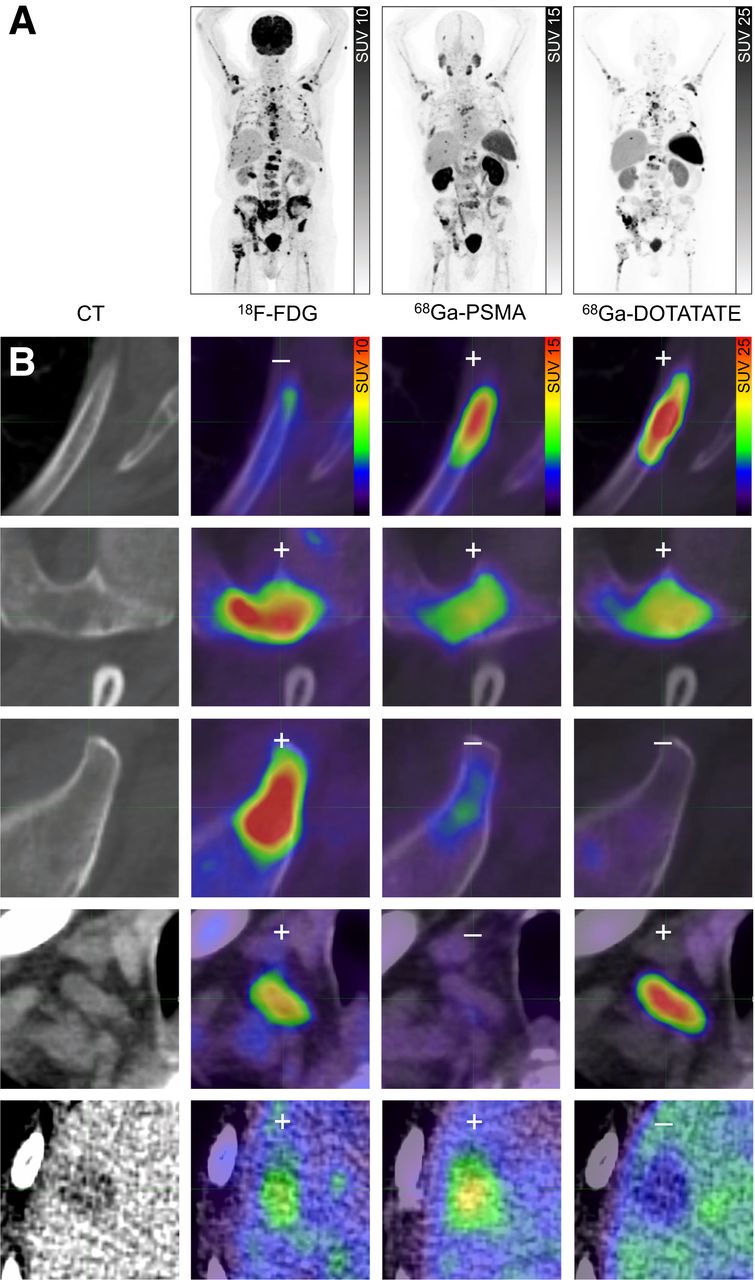
In the study, authors assessed the prevalence of IIH in mCRPC and its associated impact on overall survival. Whole-body PET imaging was conducted with three distinct PET tracers (18F-FDG, 68Ga-PSMA-617, and 68Ga-DOTATATE). Ninety-eight patients were included in the primary analysis, which included 18F-FDG and 68Ga-PSMA-617 PET/CT scans. Thirty-seven patients who were found to have at least one 18F-FDG-positive/68Ga-PSMA-617-negative lesion received an additional 68Ga-DOTATATE PET/CT scan.
IIH prevalence in the 98 patients receiving 18F-FDG and 68Ga-PSMA-617 PET/CT scans was 82.7%. In the patients who underwent 68Ga-DOTATATE PET/CT, the prevalence of IIH was 83.8%, and 16.2% had positive lesions. Based on the individual metastasis uptakes of the three tracers in each patient, at least 12 different mCRPC IIH combinations were found.
The overall survival of all enrolled patients was 10.2 months. Patients with IIH had a median overall survival of only 9.5 months and a 2.7-fold higher probability of dying of prostate cancer during the study follow-up than those without IIH. Those with at least one 18F-FDG-positive/68Ga-PSMA-617-negative lesion had a median overall survival of only 5.6 months and a 2.8-fold higher probability of dying of prostate cancer during the study follow-up than those with only 68Ga-PSMA-617-positive lesions. Finally, patients who had at least one 68Ga-DOTATATE-postive lesion had a poor median overall survival of 3.0 months and a 5.0-fold higher probability of dying of prostate cancer during the study follow-up than those without.
“These findings show an unexpected high prevalence of IIH in mCRPC patients and demonstrate that IIH and some patterns of tracer positivity are associated with decreased survival,” noted Pouliot. “In the future, molecular imaging with multiple tracers may have a novel and important role for precision medicine in mCRPC and other cancers.”
Related Articles
Citation
Multi-Tracer PET Personalizes Advanced Prostate Cancer Management. Appl Radiol.
November 18, 2024