Modified Barium Swallow Study ACR-SPR Practice Parameter: 2023 Update
Images

SLP/CRA/CE credits are available for this article here.
Introduction
The modified barium swallow study (MBSS) is a videofluoroscopic study used to evaluate oral and pharyngeal swallowing and airway protection.1-6 The American College of Radiology (ACR) creates and periodically updates Practice Parameters and Technical Standards for various radiologic procedures, including the MBSS. The goal of these Practice Parameters is to “promote the safe and effective use of diagnostic and therapeutic radiology by describing specific training, skills, and techniques,” and to “narrow the variability among radiology practices and provide guidance to achieve quality in radiology.”7 In 2023, the ACR partnered with the Society of Pediatric Radiology (SPR) to update the MBSS Practice Parameter. Here, the ACR-SPR Practice Parameter for the Performance of the Modified Barium Swallow Study is summarized, with a focus on the changes made in the recent update.8
The MBSS Description and Indications
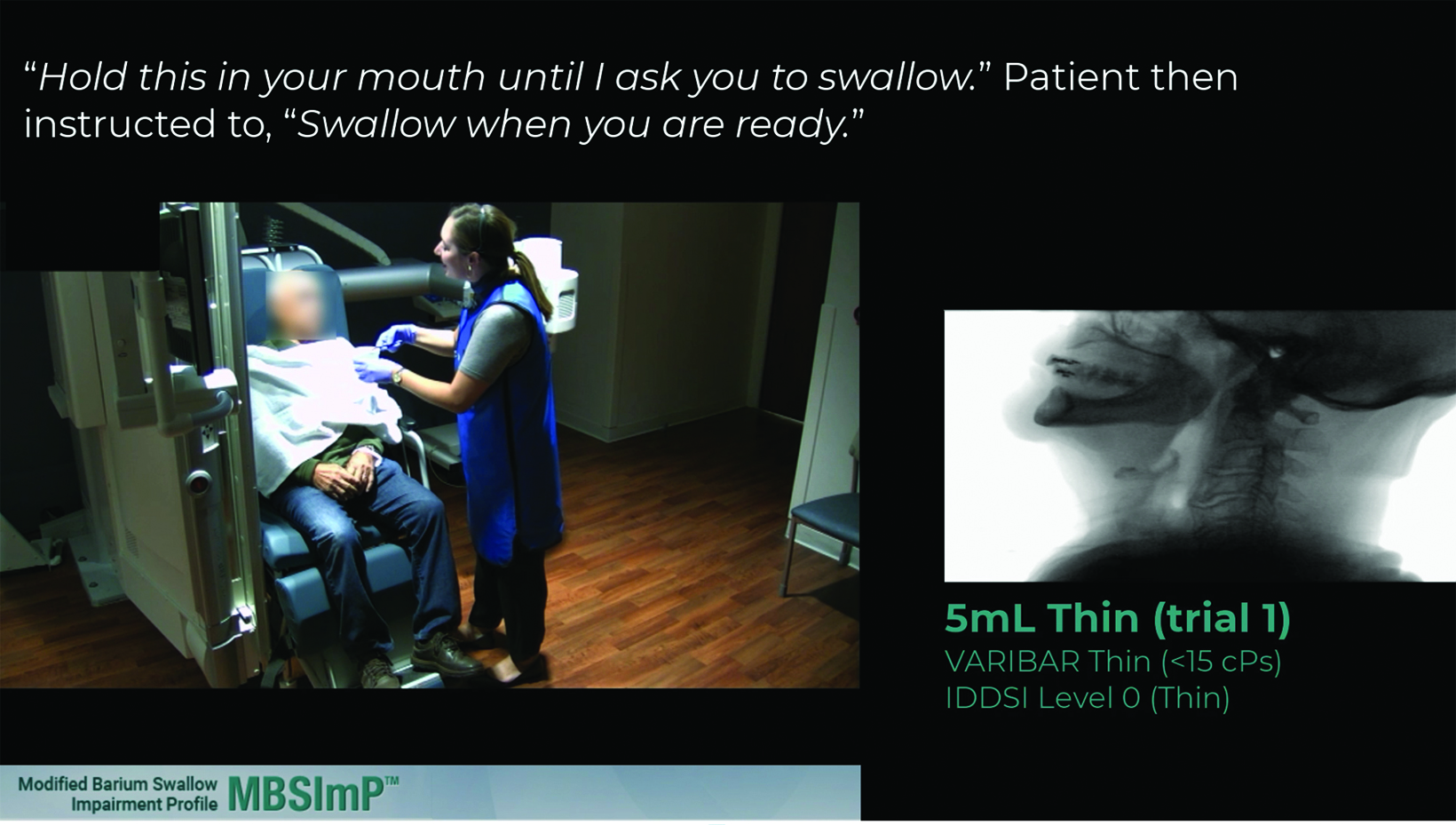
The MBSS is a real-time, contrast-enhanced fluoroscopic study performed to assess oral and pharyngeal swallowing function, airway protection, and clearance of swallowed material.1-6 It is typically performed by a radiologist and a speech-language pathologist (SLP). (Figure 1) The exam assesses the oral cavity, pharynx, larynx, and pharyngoesophageal junction. In addition to this general description, the 2023 update to the MBSS Practice Parameter includes a new paragraph describing the primary goals of the MBSS more specifically: to “identify and distinguish the presence, type, and estimated severity of physiologic swallowing impairment; determine the safety of oral intake (airway protection); determine the efficiency of oral intake (clearance); detail the effects of selected frontline interventions (postures, maneuvers, bolus variables) on swallowing physiology, airway protection, and efficiency; identify indications for specific interventions that may be appropriate for the clinical condition of the patient; and develop intake (oral, tube, etc) and diet texture/nutritional management plans in collaboration with the physician and other interdisciplinary team members.” The most commonly used contrast agent for oropharyngeal swallowing assessment contains the active ingredient barium sulfate. Patients are asked to swallow different consistencies of barium to evaluate swallowing physiology and the impact of consistencies and volumes on swallowing function.10-16
The MBSS is indicated for known or suspected oropharyngeal dysphagia. The updated ACR-SPR MBSS Practice Parameter lists 20 indications for the MBSS, up from 15 in the prior version. Additions focus mainly on broadening the indications (eg, neurologic or neurodegenerative; myopathy or nerve injury; preoperative and follow-up posttreatment), but several are entirely new: pulmonary conditions possibly related to swallowing dysfunction; after prolonged intubation and/or deconditioning; prior abnormal MBS with subsequent modification of swallow technique or improvement in patient conditioning; nasal stuffiness or noisy breathing that worsens with feeding (pediatrics); and laryngotracheal cleft.8 Unlike the previous version of the practice parameter, the update includes several contraindications: (1) known or suspected leaks from the pharynx or esophagus such as those following trauma or surgery (if a leak is suspected, an esophagram using nonionic low osmolar water-soluble contrast material should be performed before MBSS); and (2) known or suspected tracheoesophageal fistula (if suspected, an esophagram using low osmolar water-soluble contrast material should be performed before MBSS).8
The Modified Barium Swallow Study Protocol
The study protocol section of the ACR-SPR MBSS Practice Parameter includes the following: (A) Patient Selection, Preparation, and Positioning; (B) Personnel; (C) Method of Recording; (D) Modified Barium Swallow Technique; and (E) Radiographic Quality Control.8
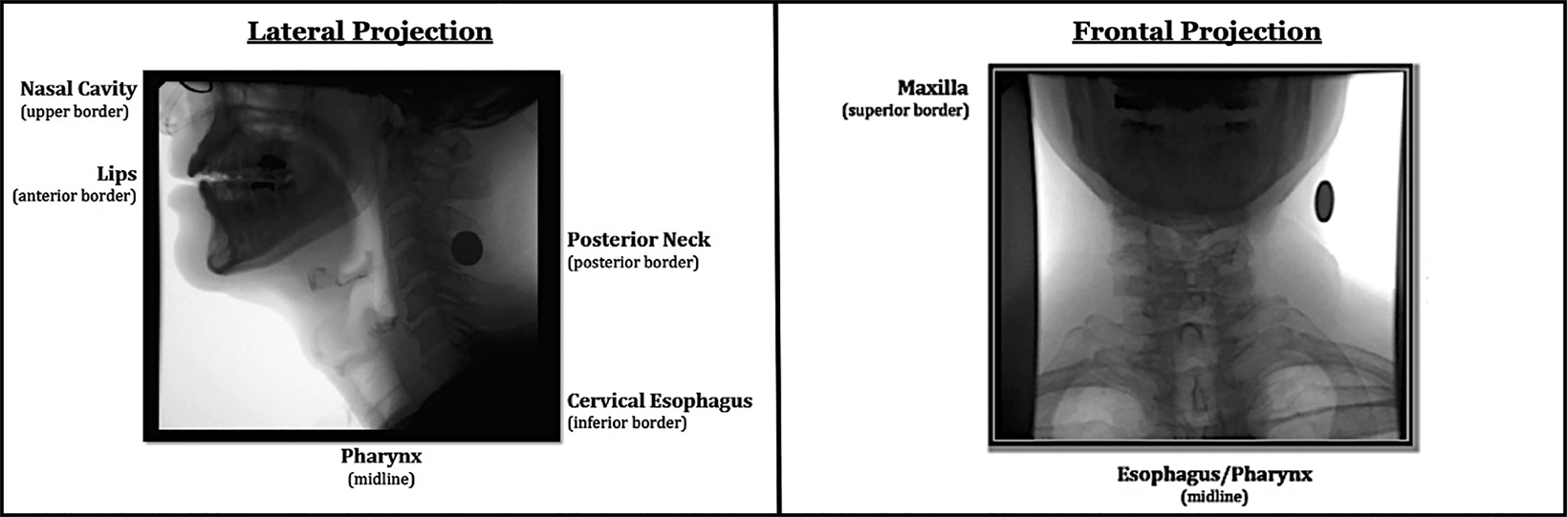
In the Patient Selection, Preparation, and Positioning section, the Practice Parameter states that “swallowing functions are usually evaluated initially in the lateral plane with the patient upright, with gravity assistance to mimic the eating and drinking position. The lateral view may be followed by frontal view observations, whenever positioning allows, to provide evaluation of symmetry of swallowing function.
Stable, commercially-prepared barium and validated, standard protocols are encouraged to optimize visualization and reproducibility of the MBS and comparison of findings across sites.”8,13,15,16
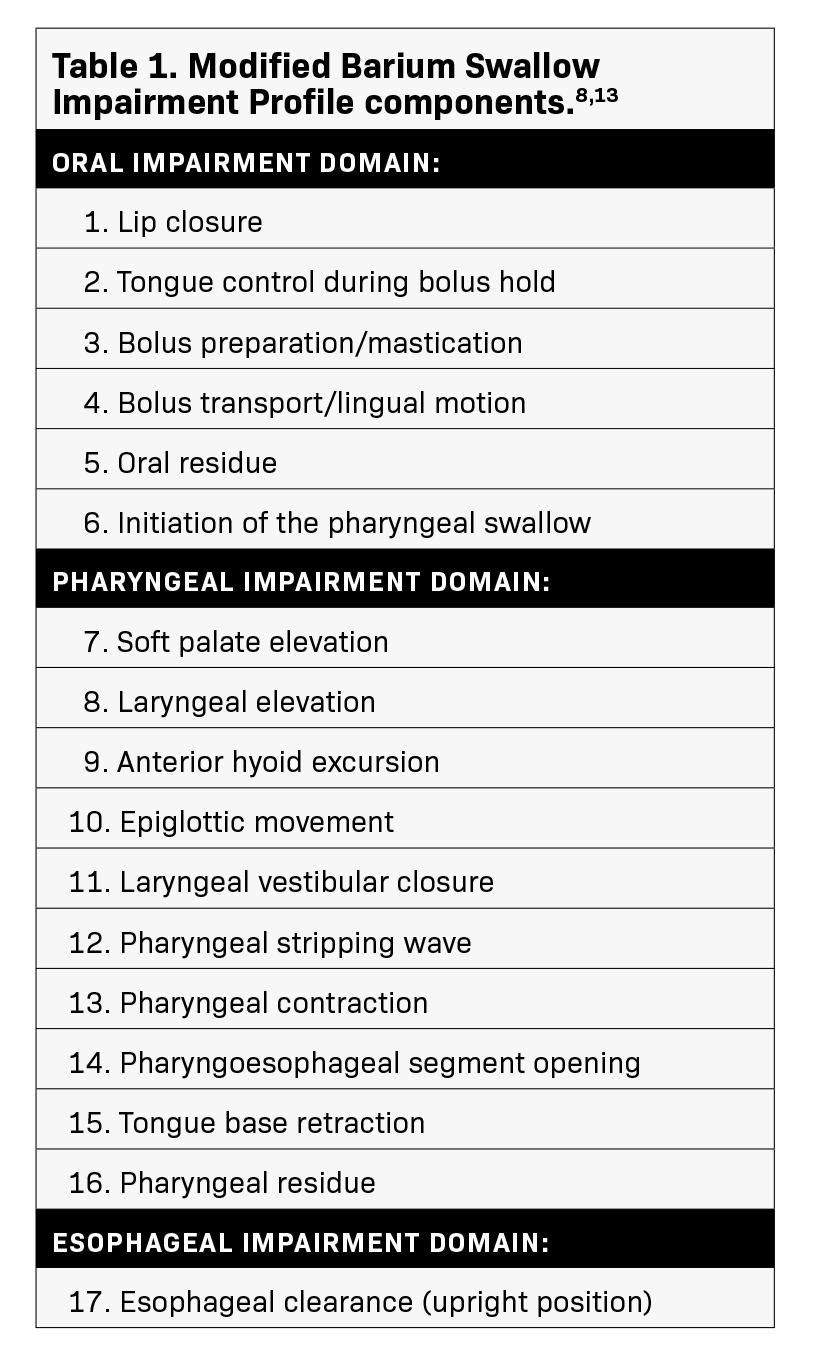
The last recommendation, to use stable, commercially-prepared barium and validated, standard protocols, has been made by experts in oropharyngeal swallowing evaluation for years, and is now included throughout the ACR-SPR Practice Parameter.13,15,16 The only avail- able standardized assessment protocol for the MBSS exam that has been rigorously tested and validated specifically for scoring oropharyngeal swallow physiology is the Modified Barium Swallow Impairment Profile (MBSImP).11,13 The MBSImP tool assesses 17 components of swallowing physiology and bolus clearance for each consistency of barium sulfate contrast.11,13 (Table 1) When used, the MBSImP allows for specific, consistent, accurate, and objective interpretation and communication of MBSS results.11,13,18,19
The contrast used for the MBSS is barium sulfate, and only one commercially prepared, US Food and Drug Administration (FDA)– approved agent specifically indicated for the MBSS exists: Varibar (Bracco Diagnostics Inc.; Figure 2). Varibar products have been formulated specifically for healthcare providers to use during the MBSS based on consistencies known to affect swallowing physiology.11,16,20 In addition, Varibar possesses minimal coating properties in order to facilitate clear visualization of the dynamic swallowing process.21,22 In standardized MBSS methodology, swallowing of a full range of barium volumes—from lower to higher—and consistencies—thin to thick—is tested using the standardized MBSImP assessment tool.14,23 Importantly, the MBSImP assessment tool was validated using Varibar; therefore, as stated in the ACR-SPR MBSS Practice Parameter, using them together is recommended to ensure reproducible, high-quality MBSS results.12,14,16,20 Despite this emphasis on standardization, it is important to note that the MBSS performed should be based on the clinical experience of the radiologist and SLP and tailored to the patient’s specific clinical question.
The section on Personnel states that the examination may be performed by a physician alone for diagnostic evaluation or by a physician and a speech-language pathologist together for both diagnosis and recommendation for therapy.8 The 2023 update also allows for a nonphysician radiology provider (NPRP) to perform the test under physician supervision.8 The precise role of the NPRP is more clearly delineated in the section on Qualifications And
Responsibilities Of Personnel (see below).8 The Method of Recording section describes the recommendations for recording functional and morphologic assessment: “For functional assessment, the fluoroscopic portion of the examination should be recorded on high-resolution videofluorographic (VF) and/or rapid digital fluorographic imaging.”8,10,24 This section is essentially unchanged in the updated Practice Parameter, except for removal of the statement that single contrast techniques may be sufficient in children.
The MBSS technique section reviews the examination protocol itself; the VF recording medium; tailored examinations; and protective, therapeutic, and provocative maneuvers. The Examination section describes the anatomical areas that should be evaluated: “The examination should include evaluation of oral, and nasopharyngeal, pharyngeal, laryngeal, and pharyngoesophageal segment function and morphology in the lateral projection. Evaluation in the frontal projection, including the oral cavity, pharyngeal walls, pharyngoesophageal segment, and upper airway, is useful to view symmetry of function and effects of applied compensatory strategies on swallowing safety and bolus clearance.”8 (Figure 3) The VF recording medium section describes recommendations related to technical aspects (eg, administration of barium consistencies and volumes customized for the MBSS and approximating the consistencies of liquids and food in an oral diet to detect swallowing impairment; assessment of the patient’s response to airway invasion, their ability to clear the aspirated materials, and their response to protective and therapeutic maneuvers; and the use of 30 pulses per second or continuous fluoroscopy).8 This section also discusses tailoring the exam to the patient, using protective and therapeutic maneuvers to limit aspiration, and provocative maneuvers to evoke or eliminate swallowing dysfunction.8 The 2023 update to this section also:
- Expands areas required for evaluation to include nasopharyngeal, laryngeal, and pharyngoesophageal function and morphology;
- Highlights the limitations of the MBSS in assessing esophageal function;
- States that, “depending on patient symptoms and findings (or lack of findings) on MBS, an esophagram may be required to complete the assessment of the patient.”8,25-28
The VF recording section has been rewritten to emphasize a number of points. First, the prior version stated that the MBSS should be performed “while the patient swallows a variety of consistencies of barium or barium-impregnated food with varying bolus volumes,” and that “the viscosity and volume of each bolus may be varied by the clinical judgment of the speech-language pathologist or the radiologist based on the patient’s presenting symptoms.”8
The newly revised Practice Parameter now says the MBSS should be performed “while the patient is administered barium consistencies and volumes customized for the MBS and that approximate the consistencies of liquids and food in an oral diet to detect swallowing impairment.”8 Moreover, the guidance now states that the use of a standardized and validated set of commercially prepared barium consistencies and volumes is recommended whenever possible, to ensure the ability to reproduce or compare repeat evaluation results, to reduce risks associated with aspiration of these substances, and to minimize infection control issues.8,11,13,18,19
These statements are consistent with those made throughout the updated guidance document that highlight the importance of using a standard protocol and commercially prepared, validated barium products to ensure repeatability and minimize contamination.13,15 Additionally, these statements are made to address the practice of mixing barium sulfate with foods and liquids, as has been done in the past in “barium kitchens.” Such practice is not recommended for a number of reasons: increased risk of aspiration, the risk of contamination from a food safety perspective, and difficulty replicating the standardized consistencies and barium concentrations within and between clinical practices, increasing intra- and interpatient variability of test results.16
The second notable addition to the VF Recording section, absent from the prior version, is guidance regarding fluoroscopic acquisition rates. Per the updated Practice Parameter: “The literature supports a fluoroscopic acquisition rate of 30 pulses per second or continuous fluoroscopy whenever possible to provide optimal visualization of rapid movements associated with swallowing and aspiration detection.18,29,30 However, fluoroscopic acquisition rates should be determined by the supervising radiologist with attention to optimally minimizing the patient’s radiation exposure and maximizing adequate swallowing evaluation.”8
Third, the updated guidance clarifies the role of the MBSS in evaluating the esophagus: “An evaluation of esophageal structure and function is beyond the scope of the MBS, which is focused on assessment of functional swallowing in the areas of the oral cavity, pharynx, larynx, and pharyngoesophageal junction.”8 MBSImP training documents concur: the role of the SLP in assessment of esophageal function should be limited to observation of bolus clearance in the upright or semi-upright position, and the MBSS or MBSImP approach is not designed to evaluate esophageal motility or structural abnormalities.36 In the MBSS Practice Parameter, it is further suggested that for evaluation of the esophagus, one consult the ACR Practice Parameter for the Performance of Esophagrams and Upper Gastrointestinal Examinations in Adults and the ACR–SPR Practice Parameter for the Performance of Contrast Esophagrams and Upper Gastrointestinal Examinations in Infants and Children.8,31,32
MBSS Pediatric Considerations
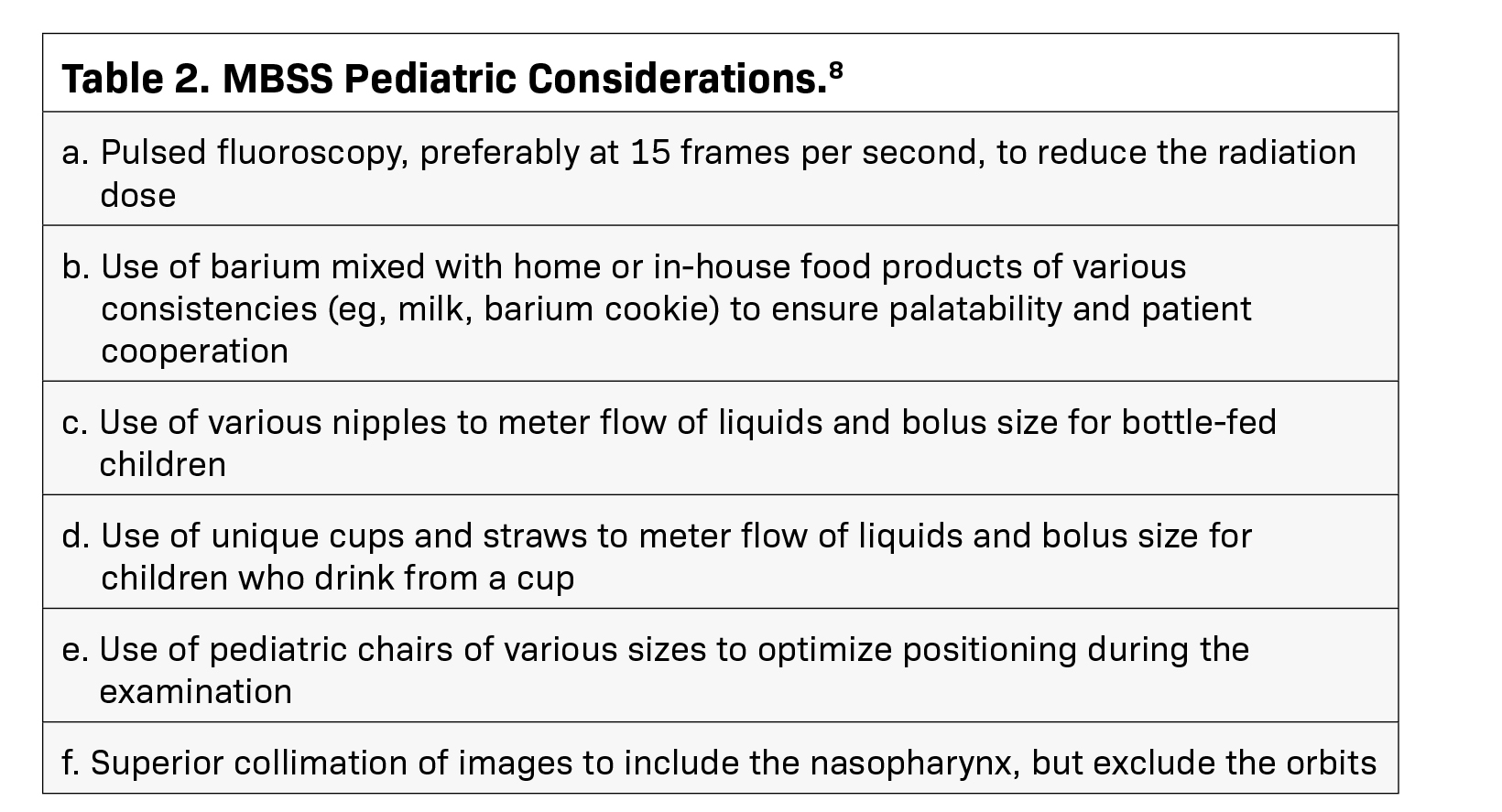
Importantly, the conclusion of the VF Recording Medium section of the updated ACR-SPR MBSS Practice Parameter document, now includes a new section supporting pediatric considerations. The recommendations, which are listed in Table 2,8 state that “pulsed fluoroscopy, preferably at 15 pulses per second, is recommended to reduce the radiation dose.”8 However, this recommenda- tion remains controversial. Some experts consider a frame rate of 30 frames per second necessary to obtain sufficient quality images.10,18
In addition, reduction in frame rate may not result in the expected concordant decrease in radiation exposure to the patient. (J. Hill; pers comm) Therefore, such guidance should be discussed among those involved in making these technical decisions and should include pediatric radiologists and medical physicists. Notably, perhaps the most effective way to reduce radiation exposure is to eliminate inappropriate or unnecessary examinations and, therefore, ensuring that an MBSS is appropriate for a particular patient is vital.
Staff Roles and Responsibilities
Because the MBSS involves a team of healthcare providers, the Practice Parameter aims to define the role of each team member, as well as the expectations for their training. The team includes the physician, the NPRP, the radiologic technologist, and the SLP.8 With the exception of the SLP, there are few changes to the updated MBSS Practice Parameter in this section. The physician should be li- censed and trained, and be up-to-date in their continuing medical education.8 The NPRP (which includes a registered radiologist assistant [RRA], radiology practitioner assistant [RPA], etc.) may assist with or participate in portions of the practice of a radiologist-led team.8 The radiologic technologist should be qualified to perform GI radiography; this includes certification by the American Registry of Radiologic Technologists (ARRT) or unrestricted state licensure.8 For SLPs, in addition to holding the Certificate of Clinical Competence in SLP from the American Speech-Language-Hearing Association (ASHA), their role has been slightly updated: “This professional should have specific education and training related to the indications and to the performance and interpretation of the MBS using validated and standardized methods.”8 Note again the use of the words “validated” and “standardized,” and how they appear repeatedly throughout the updated Practice Parameter.
Documentation
The section on documentation states that “reporting should be in accordance with the ACR Practice Parameter for Communication of Diagnostic Imaging Findings.8,33 In addition, it states that “comparison to prior MBS studies should be performed when relevant, particularly when the examination is performed to follow up previously demonstrated abnormalities” and that “patient identity (using name and/or a unique identifying number) and examination date should be recorded on the VF recording medium.”8 The only changes to this section emphasize the importance of teamwork and collaboration: “The images should be reviewed by the performing team with a discussion of the findings and conclusions agreed upon by them” and, “if there are any discordant opinions not resolved by image review, additional imaging should be performed.”8 This point is essentially reiterated at the end of this section:
“It is recommended that the radiologist and speech-language pathologist corroborate findings at the conclusion of the examination.”8,10
Equipment Specifications
Per the Practice Parameter: “Equipment performance monitoring should be in accordance with the ACR–AAPM Technical Standard for Diagnostic Medical Physics Performance Monitoring of Radiographic Equipment and the ACR–AAPM Technical Standard for Diagnostic Medical Physics Performance Monitoring of Fluoroscopic Equipment.8,34 The section on equipment specifications has been updated primarily to include reference to the importance of creating and maintaining a Quality Control (QC) Program. Specifically, the following has been added: “The equipment should be part of a Quality Management (QM)/QC Program. The QM/QC program should include an annual survey by a medical physicist.”8
Radiation Safety, Quality Control, Safety Control, and Patient Education
No changes have been made to these sections. All individuals involved in the MBSS are responsible for safety, including ensuring radiation exposure is “as low as reasonably achievable (ALARA).”8 In addition, the parameter recommends that “policies and procedures related to quality, patient education, infection control, and safety should be developed and implemented in accordance with the ACR Policy on Quality Control and Improvement, Safety, Infection Control, and Patient Education on the ACR website.”8,35
Conclusions
In 2023, the ACR and SPR updated the practice parameter for the MBSS. Overall, the most significant changes included an emphasis on using standardized, validated protocols together with stable, commercially prepared barium sulfate products, as well as the addition of specific recommendations for pediatric patients. To improve patient care and management, these updated recommendations should be considered when developing or reviewing MBSS protocols.
Author Commentary
Introductions
J. Zarzour, MD: I am an Associate Professor of Radiology at the University of Alabama at Birmingham and Vice Chair of Education for the Department of Radiology. I have been in clinical radiology practice for 15 years and enjoy collaborating with our speech language pathology colleagues.
B. Martin-Harris, PhD: I am the Alice Gabriel Twight Professor in the Department of Communication Sciences and Disorders and Associate Dean for Faculty Affairs at Northwestern University in the School of Communication. I also hold appointments in the Feinberg School of Medicine and Otolaryngology, Head and Neck Surgery and Radiation Oncology. I have been a clinician and a clinician scientist for nearly 30 years, working extensively with upper aerodigestive tract systems and disorders. I have extensive experience in conducting MBSSs, as well as in designing and executing research studies on swallowing measurement, impairment, and treatment.
J. Hill, MD: I am a Professor of Radiology and Pediatrics at the Medical University of South Carolina, as well as Vice Chair of Education for the Department of Radiology and Radiologic Science and Associate Dean for Career Planning and Advising in the College of Medicine. I have been in clinical pediatric radiology practice for 30 years and have participated in multiple research projects with my speech language pathologist colleagues.
ACR-SPR MBSS Practice Parameter Considerations
J. Zarzour, MD: Each practice parameter is developed through a consensus process. The members of the writing committee consist of physicians knowledgeable in the field. The practice parameters are updated at least every five years, or sooner if needed. I was a member of the writing committee. These are helpful practice parameters to reference as questions come up or new practices are established.
B. Martin-Harris, PhD: The practice parameters are meant to provide safe and effective use of diagnostic and therapeutic radiology by describing specific training skills and techniques, with the goal of reducing variability among radiology practices and providing guidance to achieve quality in radiology. Speech-language pathologists appreciate practice parameters and guidelines to help them reduce variability and improve outcomes. This practice parameter was developed by the ACR, not an SLP professional group, but it is inclusive of the SLP as a key figure in carrying out this examination. I have been an invited consultant to, and now associate member of, the Society of Abdominal Radiology (SAR). While I am not a member of the radiology writing group, I am pleased to have had the opportunity to provide input.
J. Hill, MD: The ACR puts out practice parameters across all sorts of imaging procedures. For us, these are guidelines – not medicolegal documents—and a consensus statement based on current literature and knowledge at the time of publication. We certainly refer to them, but they are not prescriptive –clinical judgment should be applied to each individual patient.
ACR-SPR MBSS Practice Parameter Protocol Standardization
J. Zarzour, MD: Standardized, validated protocols with commercially available barium consistencies are encouraged to optimize reproducibility and reduce variability between exams. The commercially available barium products have been developed specifically for the MBSS. Many of our patients are frequent flyers – they keep coming back, so it’s important that we can compare before and after exams to assess whether a treatment is improving their swallowing function. It’s the safest, most protocol-driven way of taking care of these patients.
B. Martin-Harris, PhD: The recommended standardized, validated protocols referenced by the writing group are based on evidence and years of research. It is a positive step forward to see that radiologists, our collaborators in swallowing assessment, value and reference the evidence in the new practice parameters.
J. Hill, MD: Standardization is important because it’s not unusual for us to have a patient referred from another institution. If the other institution is using the same protocol, then our study will be comparable, and we can determine if there’s been improvement or if it’s static or if, in fact, the function has gotten worse. And we use Varibar – it has specific consistencies, and we typically start with the thin consistency and continue on until we find the consistency that the patient is safely able to handle.
MBSS Care Team Collaboration
J. Zarzour, MD: Collaboration between the radiologists and SLP is critical to ensure the best care for our patients. We start the collaboration before the exam begins, reviewing the clinical indications for the exam, the patient’s history, and results of any prior exams. We then perform the exam together and review the findings at the conclusion. If there are conflicting conclusions in our individual reports, it could be very confusing for the team of people taking care of the patient.
B. Martin-Harris, PhD: Dr Zarzour and I have worked very hard to develop the notion of a collaborative examination between radiologists and SLPs outside of this practice parameter initiative. We are currently involved in the development of a radiology resident training initiative toward best practices in implementation and interpretation of MBSSs.
J. Hill, MD: That it’s a collaborative exam is an important point. We defer to the SLP’s expertise. They’ve often already examined the child clinically and assessed their swallowing function, so they have an idea of what the problem is. We’ll usually confer before the examination about their concerns and how best to approach the patient – they typically have much more knowledge about the individual patient when they come in to do the study with us.
ACR-SPR MBSS Practice Parameter Resources
It is recommended that the ACR-SPR MBSS Practice Parameter be reviewed, and any pertinent updates considered, when assessing the quality, reproducibility, and safety of the MBSS. The updated ACR-SPR MBSS Practice Parameter can be accessed at: www.acr.org/-/media/ACR/Files/Practice-Parameters/Modified-Ba-Swallow.pdf.
References
Citation
JG Z, B M, JG H. Modified Barium Swallow Study ACR-SPR Practice Parameter: 2023 Update. Supplement to Applied Radiology. 2024;(2):.
March 5, 2024