Melorheostosis and Osteopoikilosis
Images




Case Summary
A previously healthy adult with no medical history presented to the emergency department following pelvic and lower limb trauma.
Imaging findings
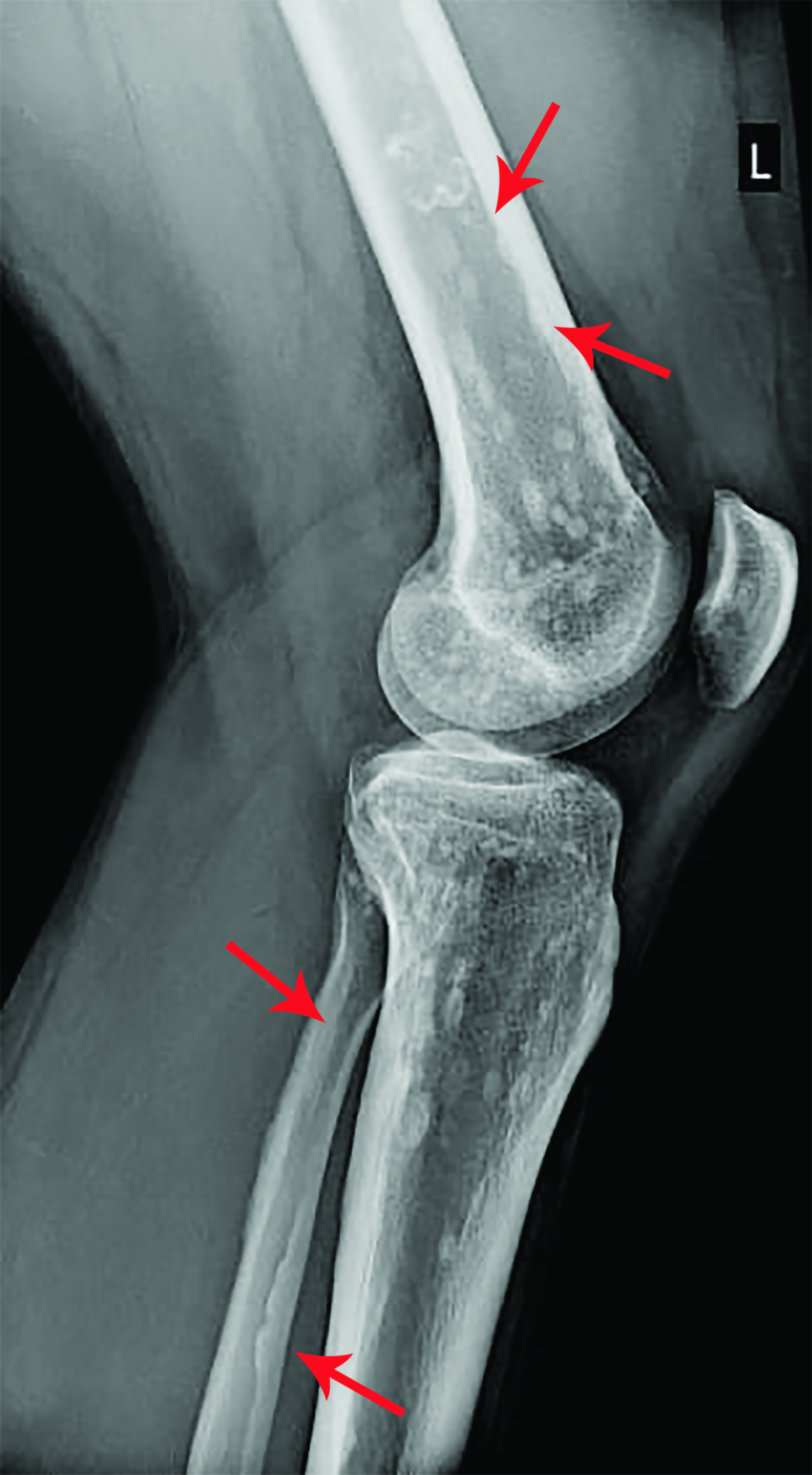
X-rays of the pelvis and left lower limb showed multiple micronodular, high-intensity, homogeneous densities varying in size up to 10 mm. These densities involved the acetabula, bilateral ilio-pubic and ischio-pubic rami, proximal and distal ephyphyses and metaphyses of the left femur and tibia, as well as the calcaneus and tarsal bones (Figure 1). The images also revealed homogeneous thickening on the inner cortical surfaces at the distal diaphysis of the left femur and proximal and middle diaphyses of the left fibula (Figure 2), with a “dripping candle wax’’ appearance.
Diagnosis
Melorheostosis and osteopoikilosis.
The differential diagnosis for melorheostosis includes myositis ossificans, osteoma, focal scleroderma, parosteal osteosarcoma, Caffey disease, sclerotic metastases, and hypertrophic osteoarthropathy.
The differential diagnosis for osteopoikilosis (OP) includes incidental bone islands (enostoses), other sclerosing bone dysplasias, sclerotic metastases, osteosarcoma, lymphoma, osteoid osteoma, chronic multifocal sclerosing osteomyelitis, calcium and phosphate metabolism abnormalities, Erdheim-Chester disease, previous instrumentation or fracture, and Paget disease.
Discussion
Melorheostosis, also known as Leri disease, ranks among the rarest, strangest, and least understood medical disorders.1 Although this sclerosing bone disorder was initially described in 1922, fewer than 500 reports can be found in the literature.1 Melorheostosis should be relatively easy to diagnose because it is characterized by sclerotic cortical bone distributed in segments.
However, a variety of radiographic patterns have been reported, and only about one-third of cases show the typical “dripping candle wax” appearance of the cortex.1 Both the periosteal and endosteal bone surfaces have thick, atypical, and eccentric hyperostosis, and it can affect a single bone or a group of contiguous bones.1 Generally, the medial or lateral side of the bone is affected, and the boundary between the affected and healthy bone is usually extremely distinct.1
Concomitant dystrophy/dysplasia issues can be particularly challenging in the syndrome of mixed sclerosing bone, as melorheostosis often coexists with different types of bone sclerosis.1 At least four distinct forms of this disorder have been identified, depending on the relative predominance of melorheostosis, osteopoikilosis, osteopathia striata, and osteosclerosis.1
Osteopoikilosis, also known as osteopathia condensans disseminata, or “spotted bone disease,” was initially recognized as an asymptomatic condition in 1915 by Albers-Schönberg. The condition is characterized by the formation of round/oval sclerotic lesions, symmetrically distributed in the epiphyses and metaphyses of the long bones and pelvis that range from 2 to 10 mm in size.2 This condition is defined by an anomaly in bone maturation during endochondral ossification.2 It first manifests in childhood and carries on throughout adulthood.2 An autosomal dominant hereditary condition, OP is brought on by a loss-of-function mutation in the LEMD3 gene.2 Typically, radiographs are sufficient to diagnose OP.2
Most of the time OP is asymptomatic, but in 15–20% of patients it manifests as pain and/or joint effusion,without deformity or dysfunction at the involved site(s).2 The cause of the symptoms and signs is unknown.2 Similar to the lesions seen in Buschke-Ollendorff syndrome, OP is occasionally accompanied by diffuse white skin lesions (dermatofibrosis lenticularis) and may also be linked to conditions like melorheostosis, keloid propensity, spinal stenosis, dwarfism, tuberous sclerosis, and scleroderma.2
Overlap syndromes are mixed sclerosing bone dysplasias that share characteristics with several different bone dysplasias.3 Dysplasias with hereditary and nonhereditary components can occur simultaneously; the combination of osteopoikilosis and melorheostosis is the most prevalent overlap syndrome.3 In general, no medical or surgical treatment is necessary for these two bone conditions.
Conclusion
Osteopoikilosis and melorheostosis are rare, but their radiological appearance is quite pathognomonic, and radiologists should be aware of the characteristic findings in these disorders to diagnose them accurately. Patient demographics and presentation are important; most patients begin developing the lesions in early childhood and are asymptomatic. They may also be part of sclerotic mixed bone disorders associated with other pathologies, making them more challenging to characterize.
References
Citation
C P, AC M, C T, D T, M R,. Melorheostosis and Osteopoikilosis. Appl Radiol. 2023;(3):46-47.
May 5, 2023