Mayo Clinic Researchers Recommend Minimally Invasive Treatments for Uterine Fibroids
Images
Mayo Clinic researchers recommend minimally invasive treatment alternatives to hysterectomy, in an invited clinical practice paper published in the New England Journal of Medicine.
"Less invasive treatments can help women recover faster and resume their normal activities more quickly. Additionally, many studies have now shown that there are health benefits to keeping the uterus and the ovaries," says Shannon Laughlin-Tommaso, MD, Mayo Clinic OB-GYN and co-lead author of the paper.
Removing the uterus, even while sparing the ovaries, increases the risks of cardiovascular disease, depression, anxiety and higher mortality. These risks are higher for people who get their uteruses removed at a young age. "Women contemplating a hysterectomy deserve counseling about these risks since there are other less invasive options for many women with fibroids," Dr Laughlin-Tommaso says.
A recent study found that nearly 60% of women undergoing hysterectomy for fibroids had not received a less invasive treatment first. Having alternative options to hysterectomy allow women to maintain their uteruses for longer.
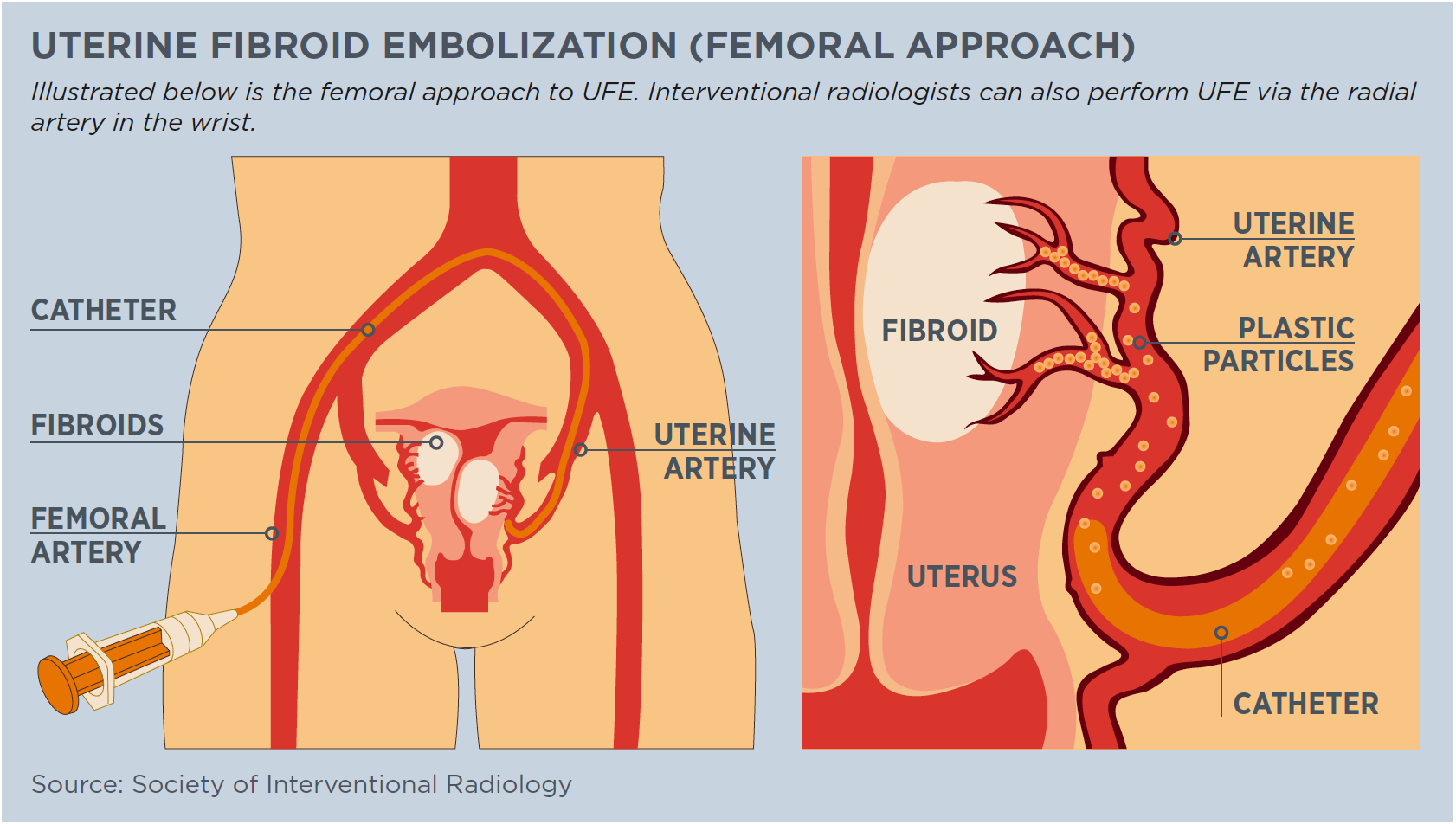
These alternatives include medical therapies, hormone-releasing IUDs, radiofrequency ablation, focused ultrasound ablation and uterine artery embolization. Early detection is key. When fibroids are found early, they tend to be smaller and less extensive. As a result, treating them early is medically less complicated. The incidence of fibroids increases with age until menopause and is higher among Black women. In addition, this population often presents with more severe fibroids.
"Earlier diagnosis and treatment of uterine fibroids can help reduce this health disparity among Black women," says Ebbie Stewart, MD, co-lead author and Mayo Clinic gynecologist and reproductive endocrinologist. In survey-based studies, many Black patients preferred minimally invasive therapies over hysterectomies.
Diagnosing fibroids is straightforward with a pelvic ultrasound but determining who to screen is not, and screening usually occurs after the fibroids are large or the patients are symptomatic. Many women with symptomatic fibroids have reported psychological suffering, including depression, concern, anger and body image distress.
The researchers suggest that future studies should include screening younger women, particularly young Black women, and people with a strong family health history of fibroids to determine if early treatment reduces long-term risks.
Hysterectomies have been the most common treatment for uterine fibroids for several reasons. "Hysterectomy makes decision-making easier for medical providers and patients. For providers, they don't have to determine which fibroids to treat or remove. Hysterectomy is also universally available in OB-GYN practices," explains Dr Laughlin-Tommaso.
Additionally, concerns about inadvertently missing a rare cancer that grows in the smooth muscle of the uterus, known as leiomyosarcoma, has led to an increased rate of hysterectomies over less invasive approaches. Lastly, a major reason for hysterectomy is that fibroids can recur about 50% of the time within five years after they are removed. However, the researchers note that not all new fibroids will become symptomatic, especially among women entering menopause.