Managing Incidental Findings
Images
An incidental finding, also referred to as an incidentaloma, is a mass or lesion detected on diagnostic imaging studies performed for an unrelated reason.1 For example, a pulmonary nodule discovered on a computed tomography (CT) angiogram of the chest for a suspected pulmonary embolism is considered an incidental finding.2
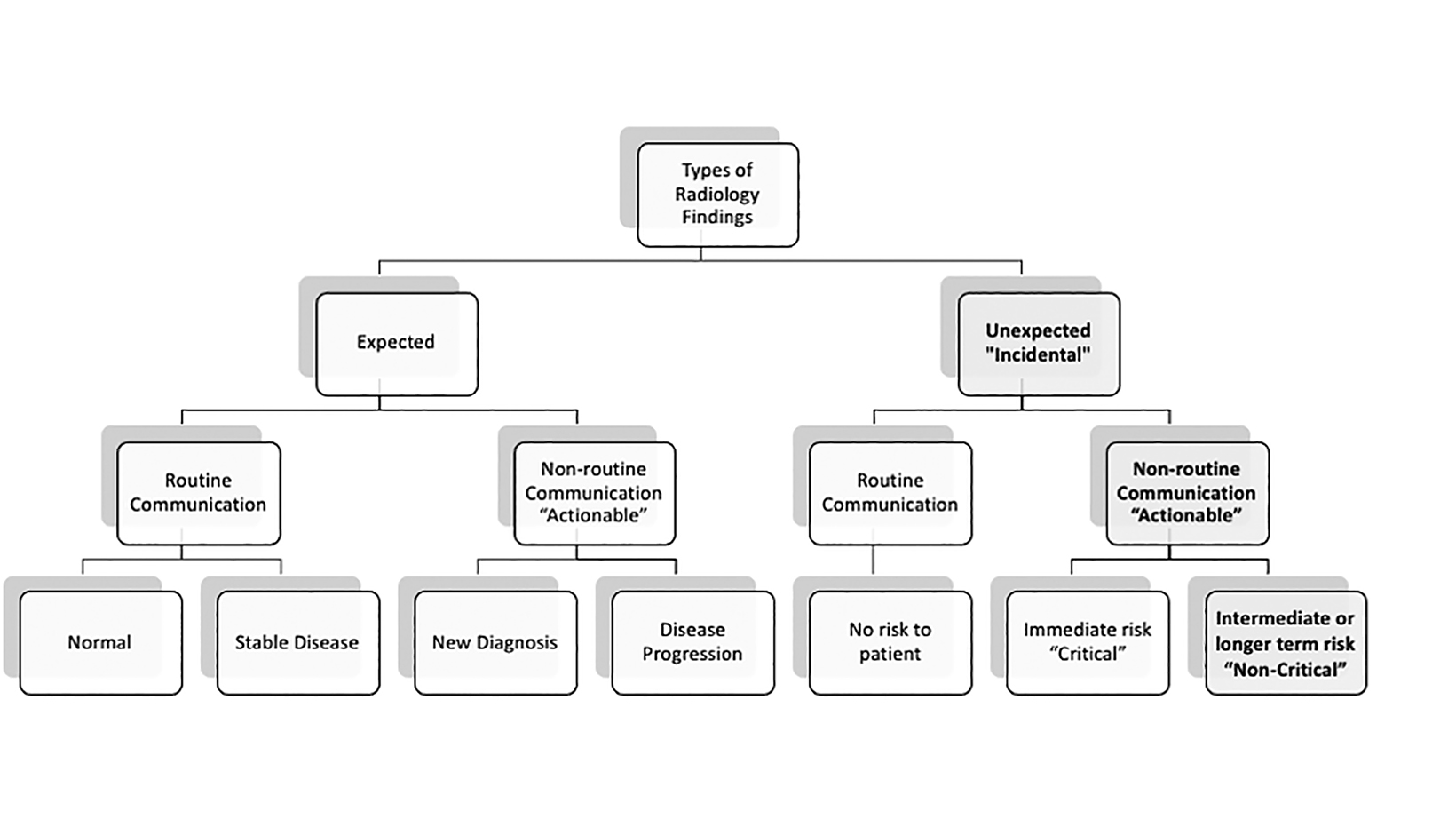
Radiologists recognize that ensuring appropriate follow-up for incidental findings is highly important. Those that require additional action are referred to as an actionable incidental finding (AIF, Figure1). Approximately 65% of all incidental findings are AIFs; among these, a diagnosis is confirmed in approximately 45% of patients.3 The incidence of cancer among all incidental findings completing follow-up is 2.3-4.5%.4,5
In this review, we discuss the nature of AIFs and how radiologists supported by information technology (IT) tools can best manage them to achieve better patient outcomes.
Best Practices for Managing AIFs
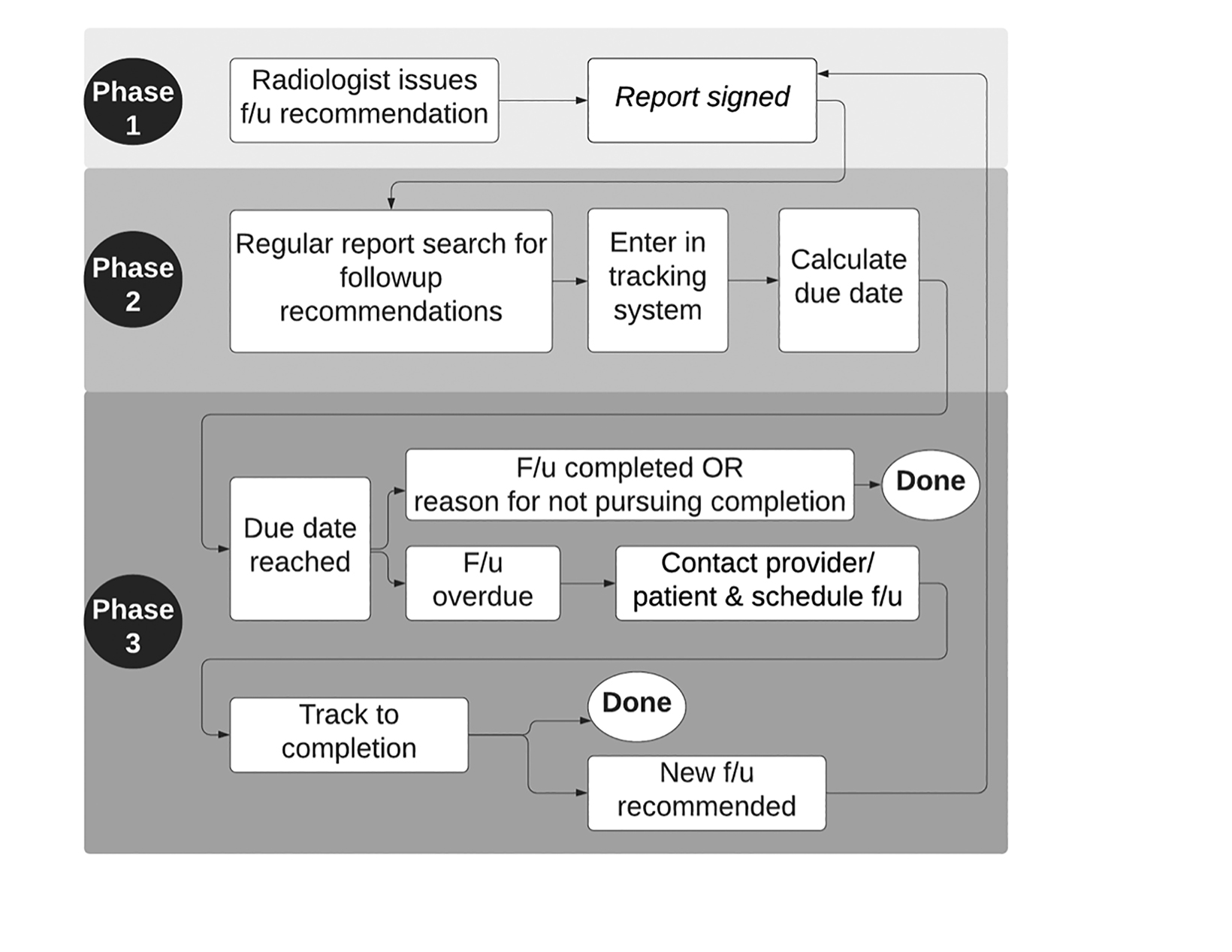
Managing AIFs is complex; ensuring completion of any recommended follow-up is vitally important (Figure 2). The process starts when the radiologist detects and determines that a lesion on an image is an AIF and issues a recommendation for follow-up review, which is then accompanied by a closed-loop result communication to clinicians. Follow-up is tracked and documented upon completion.
Closing the Loop on Result Communication
An important concept in managing AIF is “closing the loop.” This consists of conveying the specified information to a recipient, the recipient acknowledging receipt of the information and requesting clarification if necessary and, finally, the original sender confirming that the information received is well understood.6 Closed loop communications, including the names of the sender and recipient, are documented in the radiology report or patient chart and include the names of both the reporter and recipient of the information, date, time, and means of communication.7
Closed-loop communication with respect to AIFs may be accomplished verbally or through electronic communication technologies that can automatically confirm that the results were read by the recipient. Such technology can reduce the notification time of abnormal results, increase the rates of lab and pathology follow-up, and improve communication of these results.8
Evidence-based Follow-up Recommendations
Evidence-based documents guide radiologists in identifying findings that do or do not require follow-up. They also help radiologists issue follow-up recommendations with regards to imaging modality and follow-up time intervals. Evidence-based guidance can prevent unnecessary follow-up tests, thereby decreasing patient anxiety and financial burden on patients and society.9
Many medical societies and the American College of Radiology (ACR) have developed documents to guide management of various incidental findings.10 When the evidence base for some existing guidance documents is weak, or when there is no evidence to inform management, radiologists can collaborate locally to develop standardized recommendations based on local expert opinions.11 Otherwise, radiologists have to rely on their own experience and level of confidence.
Effectiveness of Follow-up Recommendations
The wording and placement of follow-up recommendations in the radiology report can affect how likely they are to be completed and to engage patients in the process.
Follow-up recommendation language should be clear and concise. Statements like, “If clinically indicated, follow-up CT could be performed in 4–6 weeks to document resolution,” limit clinicians’ ability to judge the necessity of follow-up and lead to low follow-up rates.12,13 On the other hand, recommendations that precisely identify the lesion in question, the recommended modality, and time interval can result in higher completion rates.12,13 Detailed recommendations should be placed in the Impression section of the radiology report, where they can be easily seen and noted by clinicians.14,15 For example, a section in the radiology report reading, “Recommendation: Right upper lobe pulmonary nodule follow-up with a CT in 3-6 months to assess stability,” is more useful than “follow-up to assess stability.”13,15
Patient engagement plays an important role in ensuring that follow-up is completed. With passage of the 21st Century Cures Act, patient access to test results and clinical notes no longer poses a barrier, but their highly technical language is inaccessible to most patients.16 In the emergency room and some radiology settings, results may be discussed directly with patients.14,17 This helps ensure that patients fully understand the findings and their next steps.14 Similarly, placing Info-RADS messages in radiology reports is an effective way to convey the nature of imaging results and whether any further steps are necessary.18 These messages indicate to patients either that the results are normal and no additional steps need to be taken, or that there was a non-emergent finding for which the patient should contact their provider to discuss next steps.18 Sending radiology results to patients, as is mandated in states such as Pennsylvania for AIFs, without providing an opportunity to ask for clarification, can risk increased patient distress that could in turn decrease patient willingness to pursue follow-up.18,19
Closing the Loop on Timely Follow-up Execution
Tracking systems can be used to check whether follow-up has been completed or deemed clinically obsolete, as well as to intervene when it has not been completed as required (Figure 2).4,5,20
About 30% of follow-up recommendations lack confirmation of completion, posing a significant safety gap for patients and providers.21-23 The effectiveness of tracking systems in diminishing this safety gap is well documented. For example, a tracking system for incidental lung nodules reduce the missed follow-up rate from 74% to 10%.24 Mammography reminder systems increase the likelihood of obtaining a mammogram by 50%.25 At a single institution, AIF tracking systems increased follow-up completion rates from 43% to 71%.20
Tracking Process and IT Tools
Many strategies are becoming available to simplify and make AIF management more effective and efficient.
Accessing Evidence-based Guidance
Some strategies focus on making evidence-based guidance accessible to radiologists when they are issuing their reports. Low-fidelity strategies using either no or simple IT tools, fall into three categories: physical or verbal reminders, electronic references, and enhanced reporting templates.26 Radiologists may access guidance documents as abbreviated hard copies their workstation. They may learn about guidance documents during monthly case conferences or through designated “guideline champions” who work with clinical teams to sustain guidance-based incidental findings management.27-29 Electronic guideline references may also be embedded within reporting systems, where radiologists can easily access and review them.30-33 In “enhanced radiology reporting,” the report includes more detail, such as the probability that a lung nodule is cancer, and a reference to the follow-up recommendation.34,35
Although these simple strategies are an improvement over baseline, they typically yield inconsistent results owing to their reliance on individual radiologist practices. It is conceivable that practice standardization across the radiology enterprise using more sophisticated technology would be more successful.26,36-38
Tracking Systems
Several US radiology practices use hybrid tracking systems that employ a mix of staffing and advanced IT tools (Figure 2).4
These systems may identify reports containing follow-up recommendations either by asking radiologists to flag reports with specific searchable phrases (eg, “#follow”) or by having tracking staff search independently for keywords and phrases.4 These tools may work manually or employ natural language processing (NLP) capabilities. The tracking team manually enters incomplete follow-up cases into an electronic database, and IT tools may be used to determine the date by which a given follow-up should be completed.4 For overdue cases, the responsibility for ordering follow-up care is typically reassigned to the clinical team.14,24,39-42
Tracking system scalability remains a challenge, owing mainly to the need for support staff. No consensus currently exists among medical specialists and administrators regarding responsibility for oversight and financial accountability for tracking systems.43 As an unintended consequence, underfunded tracking programs may focus only on a handful of incidental finding categories, such as lung nodules.24,44-51
Natural Language Processing
Natural language processing has emerged as a promising building block towards full automation of tracking systems.52-55 NLP-enabled applications can extract information from radiology reports and identify text that represents either AIFs or follow-up ecommendations.48,56 Currently, NLP tools can identify radiology reports with follow-up recommendations entered into a tracking system, but chart review and additional follow-up actions still require dedicated staffing.
Fully Automated Tracking
Full tracking automation would be able to mine reports for AIFs based on descriptors used by the radiologist; insert appropriate follow-up recommendations into the report; transfer cases into a tracking data base, search electronic medical records for follow-up completion; send reminders for any pending follow-up; assist with scheduling, and issue a final alert should a completed follow-up not be identified. While some NLP-based methods have been developed, dashboard review, closed-loop provider and/or patient messaging systems, and scheduling tools, and comprehensive tools supporting the entire tracking process for the breadth of incidental finding types remain lacking.
Future Directions
Ensuring completion of follow-up recommendations for AIFs is important, given the large number of patients affected and the relatively high yield of clinically relevant diagnoses in this cohort. Missing such diagnoses, particularly with respect to cancer, is devastating for patients and represents a medicolegal risk to radiology practices.
Several studies have shown the feasibility of tracking systems for radiology follow-up recommendations, resulting in significant improvements in follow-up completion rates. However, the development of IT tools that support each step of the tracking workflow and that can easily be integrated with existing workflow technologies are urgently needed to make tracking programs more affordable and reliable. Tracking systems largely do not meet patients’ needs, thereby limiting patient engagement and compliance with radiology follow-up recommendations.
References
- American College of Radiology (ACR). Incidental Findings. Accessed July 18, 2021. https://www.acr.org/Clinical-Resources/Incidental-Findings.
- Hall WB, Truitt SG, Scheunemann LP, et al. The prevalence of clinically relevant incidental findings on chest computed tomographic angiograms ordered to diagnose pulmonary embolism. Arch Intern Med. 2009 Nov 23;169(21):1961-5. doi: 10.1001/archinternmed.2009.360. PMID: 19933956.
- Lumbreras B, Donat L, Hernández-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol. 2010 Apr;83(988):276-89. doi: 10.1259/bjr/98067945. PMID: 20335439; PMCID: PMC3473456.
- Irani N, Saeedipour S, Bruno MA. Closing the loop-a pilot in health system improvement. Curr Probl Diagn Radiol. 2020 Sep-Oct;49(5):322-325. doi: 10.1067/j.cpradi
- ol.2020.02.006. Epub 2020 Mar 2. PMID: 32220539.
- Mannix J, LaVoye J, Wasserman M, et al. Notification system for overdue radiology recommendations improves rates of follow-up and diagnosis. AJR Am J Roentgenol. 2021 Jun 2:1-6. doi: 10.2214/AJR.20.23173. Epub ahead of print. PMID: 34076452
- Salik I, Ashurst JV. Closed Loop Communication Training in Medical Simulation. 2021 Jul 26. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 31751089.
- American College of Radiology (ACR). ACR Practice Guideline For Communication Of Diagnostic Imaging Findings (2020). Accessed July 18, 2021. https://www.acr.org/-/media/acr/files/practice-parameters/communicationdiag.pdf.
- Sloan CE, Chadalavada SC, Cook TS, Langlotz CP, Schnall MD, Zafar HM. Assessment of follow-up completeness and notification preferences for imaging findings of possible cancer: what happens after radiologists submit their reports? Acad Radiol. 2014 Dec;21(12):1579-86. doi: 10.1016/j.acra.2014.07.006. Epub 2014 Aug 30. PMID: 25179562; PMCID: PMC4825815.
- Hanna TN, Shekhani H, Zygmont ME, Kerchberger JM, Johnson JO. Incidental findings in emergency imaging: frequency, recommendations, and compliance with consensus guidelines. Emerg Radiol. 2016;23(2):169-174. PMID: 26842832.
- American College of Radiology (ACR). Incidental Findings. Accessed July 18, 2021. https://www.acr.org/Clinical-Resources/Incidental-Findings.
- Roddy E, Zhang W, Doherty M,et al. Evidence-based clinical guidelines: a new system to better determine true strength of recommendation. J Eval Clin Pract. 2006 Jun;12(3):347-52. doi: 10.1111/j.1365-2753.2006.00629.x. PMID: 16722921.
- Gunn ML, Lehnert BE, Hall CS, Yetisgen M, Trovato K, Dalal S. Use of conditional statements in radiology follow-recommendation sentences: relationship to follow up compliance. In Radiological Society of North America 101st Scientific Assembly and Annual Meeting 2015 Nov 29.
- Mabotuwana T, Hall CS, Tieder J, Gunn ML. Improving quality of follow-up imaging recommendations in radiology. AMIA Annu Symp Proc. 2018 Apr 16;2017:1196-1204. PMID: 29854188; PMCID: PMC5977608.
- Baccei SJ, Chinai SA, Reznek M, Henderson S, Reynolds K, Brush DE. System-level process change improves communication and follow-up for emergency department patients with incidental radiology findings. J Am Coll Radiol. Apr 2018;15(4):639-647. doi:10.1016/j.jacr.2017.11.031
- Lukaszewicz A, Uricchio J, Gerasymchuk G. The art of the radiology report: practical and stylistic guidelines for perfecting the conveyance of imaging findings. Can Assoc Radiol J. 2016 Nov;67(4):318-321. doi: 10.1016/j.carj.2016.03.001. Epub 2016 Jul 21. PMID: 27451909.
- Trofimova A, Vey BL, Safdar NM, Duszak R Jr, Kadom N. Radiology report readability: an opportunity to improve patient communication. J Am Coll Radiol. 2018 Aug;15(8):1182-1184. doi: 10.1016/j.jacr.2018.03.032. Epub 2018 May 10. PMID: 29755002.
- Mohan SK, Hudgins PA, Patel MR, Stapleton J, Duszak R Jr, Aiken AH. Making time for patients: positive impact of direct patient reporting. AJR Am J Roentgenol. 2018 Jan;210(1):W12-W17. doi: 10.2214/AJR.17.18327. Epub 2017 Dec 8. PMID: 29220209.
- Kadom N, Tamasi S, Vey BL,et al. Info-RADS: adding a message for patients in radiology reports. J Am Coll Radiol. 2021 Jan;18(1 Pt A):128-132. doi: 10.1016/j.jacr.2020.09.049. Epub 2020 Oct 14. PMID: 33068534.
- Mittl GS, Cook TS, Hill PA,et al. Patient understanding of abnormal imaging findings under Pennsylvania act 112: a call to revise mandated notification message language. J Am Coll Radiol. 2021 Jul;18(7):951-961. doi: 10.1016/j.jacr.2021.02.012. Epub 2021 Mar 13. PMID: 33726983.
- Wandtke B, Gallagher S. Reducing delay in diagnosis: multistage recommendation tracking. AJR Am J Roentgenol. 2017 Nov;209(5):970-975. doi: 10.2214/AJR.17.18332. Epub 2017 Jul 25. PMID: 28742377.
- Kadom N, Doherty G, Solomon A et al. Safety-Net Academic Hospital Experience in Following Up Noncritical Yet Potentially Significant Radiologist Recommendations. AJR Am J Roentgenol. 2017 Nov;209(5):982-986.
- Lee B, Otero HJ, Whitehead MT. The fate of radiology report recommendations at a pediatric medical center. Pediatr Radiol. 2017 Dec;47(13):1724-1729. doi: 10.1007/s00247-017-3960-4. Epub 2017 Aug 29. PMID: 28852809.
- Mabotuwana T, Hombal V, Dalal S, Hall CS, Gunn M. Determining adherence to follow-up imaging recommendations. J Am Coll Radiol. 2018 Mar;15(3 Pt A):422-428. doi: 10.1016/j.jacr.2017.11.022. PMID: 29502651
- Shelver J, Wendt CH, McClure M, et al. Effect of an automated tracking registry on the rate of tracking failure in incidental pulmonary nodules. J Am Coll Radiol. 2017 Jun;14(6):773-777. doi: 10.1016/j.jacr.2017.02.001. Epub 2017 Apr 21. PMID: 28434846; PMCID: PMC8048208.
- Wagner TH. The effectiveness of mailed patient reminders on mammography screening: a meta-analysis. Am J Prev Med. 1998 Jan;14(1):64-70. doi: 10.1016/s0749-3797(97)00003-2. PMID: 9476837.
- Crable EL, Feeney T, Harvey J, et al. Management strategies to promote follow-up care for incidental findings: a scoping review. J Am Coll Radiol. 2021 Apr;18(4):566-579. doi: 10.1016/j.jacr.2020.11.006. Epub 2020 Dec 2. PMID: 33278340.
- Ridge CA, Hobbs BD, Bukoye BA, et al. Incidentally detected lung nodules: clinical predictors of adherence to Fleischner Society surveillance guidelines. J Comput Assist Tomogr. Jan-Feb 2014;38(1):89-95. doi:10.1097/RCT.0b013e3182a939a5
- Rosenkrantz AB, Kierans AS. US of incidental adnexal cysts: adherence of radiologists to the 2010 Society of Radiologists in Ultrasound guidelines. Radiology. 2014;271(1):262-71. doi:10.1148/radiol.13131203
- Paluska TR, Sise MJ, Sack DI, Sise CB, Egan MC, Biondi M. Incidental CT findings in trauma patients: incidence and implications for care of the injured. J Trauma. 2007;62(1):157-61. doi:10.1097/01.ta.0000249129.63550.cc
- Clark TJ, Coats G. Adherence to ACR incidental finding guidelines. J Am Coll Radiol. Dec 2016;13(12 Pt A):1530-1533. doi:10.1016/j.jacr.2016.05.008
- Zygmont ME, Shekhani H, Kerchberger JM, Johnson JO, Hanna TN. Point-of-Care Reference Materials Increase Practice Compliance With Societal Guidelines for Incidental Findings in Emergency Imaging. J Am Coll Radiol. Dec 2016;13(12 Pt A):1494-1500. doi:10.1016/j.jacr.2016.07.032
- Eldeiry LS, Alfisher MM, Callahan CF, Hanna NN, Garber JR. The impact of an adrenal incidentaloma algorithm on the evaluation of adrenal nodules. J Clin Transl Endocrinol. Sep 2018;13:39-45. doi:10.1016/j.jcte.2018.07.001
- Kim DC, Bennett GL, Somberg M, et al. A multidisciplinary approach to improving appropriate follow-up imaging of ovarian cysts: a quality improvement initiative. J Am Coll Radiol. May 2016;13(5):535-41. doi:10.1016/j.jacr.2016.01.015Woloshin S, Schwartz LM, Dann E, Black WC. Using radiology reports to encourage evidence-based practice in the evaluation of small, incidentally detected pulmonary nodules. A preliminary study. Ann Am Thorac Soc. Feb 2014;11(2):211-4. doi:10.1513/AnnalsATS.201307-242BC
- Zafar HM, Chadalavada SC, Kahn CE, Jr., et al. Code abdomen: an assessment coding scheme for abdominal imaging findings possibly representing cancer. J Am Coll Radiol. Sep 2015;12(9):947-50. doi:10.1016/j.jacr.2015.04.005
- Prior M, Guerin M, Grimmer-Somers K. The effectiveness of clinical guideline implementation strategies--a synthesis of systematic review findings. J Eval Clin Pract. Oct 2008;14(5):888-97. doi:10.1111/j.1365-2753.2008.01014.x
- Bosmans JM, Weyler JJ, De Schepper AM, Parizel PM. The radiology report as seen by radiologists and referring clinicians: results of the COVER and ROVER surveys. Radiology. Apr 2011;259(1):184-95. doi:10.1148/radiol.10101045
- Chung CY, Makeeva V, Yan J, et al. Improving billing accuracy through enterprise-wide standardized structured reporting with cross-divisional shared templates. J Am Coll Radiol. Jan 2020;17(1 Pt B):157-164. doi:10.1016/j.jacr.2019.08.034
- Moseson EM, Wiener RS, Golden SE, et al. Patient and clinician characteristics associated with adherence: a cohort study of veterans with incidental pulmonary nodules. Ann Am Thorac Soc. May 2016;13(5):651-9. doi:10.1513/AnnalsATS.201511-745OC
- Holden WE, Lewinsohn DM, Osborne ML, et al. Use of a clinical pathway to manage unsuspected radiographic findings. Chest. May 2004;125(5):1753-60. doi:10.1378/chest.125.5.1753
- Huynh TT, Moran KR, Blackburn AH, Jacobs DG, Thomason MH, Sing RF. Optimal management strategy for incidental findings in trauma patients: an initiative for midlevel providers. J Trauma. Aug 2008;65(2):331-4; discussion 335-6. doi:10.1097/TA.0b013e31817e5153
- Hammer MM, Kapoor N, Desai SP, et al. Adoption of a closed-loop communication tool to establish and execute a collaborative follow-up plan for incidental pulmonary nodules. AJR Am J Roentgenol. Feb 19 2019:1-5. doi:10.2214/ajr.18.20692
- Kadom N, Fredericks N, Moore CL, Seidenwurm D, Shugarman S, Venkatesh A. Closing the compliance loop on follow-up imaging recommendations: comparing radiologists’ and administrators’ attitudes. Curr Probl Diagn Radiol. Aug 2021. doi:10.1067/j.cpradiol.2021.08.003
- Singh H, Thomas EJ, Mani S, et al. Timely follow-up of abnormal diagnostic imaging test results in an outpatient setting: are electronic medical records achieving their potential? Arch Internal Med. 2009;169(17):1578-86. doi:10.1001/archinternmed.2009.263
- Choksi VR, Marn CS, Bell Y, Carlos R. Efficiency of a semiautomated coding and review process for notification of critical findings in diagnostic imaging. AJR Am J Roentgenol. Apr 2006;186(4):933-6. doi:10.2214/ajr.04.1913
- Kang SK, Doshi AM, Recht MP, Lover AC, Kim DC, Moore W. Process improvement for communication and follow-up of incidental lung nodules. J Am Coll Radiol. Feb 2020;17(2):224-230. doi:10.1016/j.jacr.2019.11.023
- Singh H, Arora HS, Vij MS, Rao R, Khan MM, Petersen LA. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. Jul-Aug 2007;14(4):459-466. doi:10.1197/jamia.M2280
- Cook TS, Lalevic D, Sloan C, et al. Implementation of an automated radiology recommendation-tracking engine for abdominal imaging findings of possible cancer. J Am Coll Radiol. 2017 May;14(5):629-636. doi: 10.1016/j.jacr.2017.01.024. Epub 2017 Mar 17. PMID: 28325488.
- Blagev DP, Lloyd JF, Conner K, et al. Follow-up of incidental pulmonary nodules and the radiology report. J Am Coll Radiol. Apr 2014;11(4):378-83. doi:10.1016/j.jacr.2013.08.003
- Little BP, Gilman MD, Humphrey KL, et al. Outcome of recommendations for radiographic follow-up of pneumonia on outpatient chest radiography. AJR Am J Roentgenol. Jan 2014;202(1):54-9. doi:10.2214/ajr.13.10888
- Balthazar P HP, Safdar N, Toland C, Reigel T. Use of automated retrieval tool to track noncritical incidental findings follow-up. Poster presented at: SIIM Scientific Sessions; 2017; Pittsburgh, PA. Accessed February 5, 2020.
- Bala W, Steinkamp J, Feeney T, et al. A web application for adrenal incidentaloma identification, tracking, and management using machine learning. Appl Clin Inform. Aug 2020;11(4):606-616. doi:10.1055/s-0040-1715892
- Kang SK, Garry K, Chung R, et al. Natural language processing for identification of incidental pulmonary nodules in radiology reports. J Am Coll Radiol. Nov 2019;16(11):1587-1594. doi:10.1016/j.jacr.2019.04.026
- Oliveira L, Tellis R, Qian Y, Trovato K, Mankovich G. Identification of incidental pulmonary nodules in free-text radiology reports: an initial investigation. Stud Health Technol Inform. 2015;216:1027. PMID: 26262327.
- Dutta S, Long WJ, Brown DF, Reisner AT. Automated detection using natural language processing of radiologists recommendations for additional imaging of incidental findings. Ann Emerg Med. Aug 2013;62(2):162-9. doi:10.1016/j.annemergmed.2013.02.001
- Trivedi G, Dadashzadeh ER, Handzel RM, Chapman WW, Visweswaran S, Hochheiser H. Interactive NLP in clinical care: identifying incidental findings in radiology reports. Appl Clin Inform. 2019 Aug;10(4):655-669. doi: 10.1055/s-0039-1695791. Epub 2019 Sep 4. PMID: 31486057; PMCID: PMC6727024
References
Citation
V M, K S, M D, N K. Managing Incidental Findings. Appl Radiol. 2021;(6):22-26.
November 6, 2021