Low-Frequency Ultrasound Volography as Sensitive as 7T MRI for Prostate Cancer Screening
 A National Cancer Institute study comparing the low-frequency ultrasound volography QTscan with multi-parametric (mp) 7T MRI for prostate cancer screening found it was equal or better in sensitivity for detection of cancer. The initial series of 10 patients in the blinded study was done in collaboration with the Urologic Oncology Branch, Center for Interventional Oncology National Cancer Institute, Bethesda, MD and the Department of Biomedical Engineering, Johns Hopkins University, Baltimore, MD.
A National Cancer Institute study comparing the low-frequency ultrasound volography QTscan with multi-parametric (mp) 7T MRI for prostate cancer screening found it was equal or better in sensitivity for detection of cancer. The initial series of 10 patients in the blinded study was done in collaboration with the Urologic Oncology Branch, Center for Interventional Oncology National Cancer Institute, Bethesda, MD and the Department of Biomedical Engineering, Johns Hopkins University, Baltimore, MD.
On blinded sector-based analysis, QT's low-frequency-transmitted ultrasound volography had a sensitivity of 85.7% and specificity of 93.9%, while mpMRI had a sensitivity of 65.3% and specificity of 96.6%. These results demonstrate that QT's imaging technology has significant potential as a low-cost, high resolution imaging modality for prostate cancer.
The study collected specimens from 53 patients undergoing Robot Assisted Radical Prostatectomy (RARP) for biopsy-confirmed PCa from February 2021 to February 2022. Thirteen of fifty-three prostate specimens had scanned and annotated histopathology slides and mpMRI scans; three were excluded for a history of androgen deprivation therapy or radiation. Of the remaining ten, the median age at surgery was 60 years [IQR 58.3-67.5] and median PSA was 6.85 ng/mL [IQR 5.78-8.73]. Six patients had Gleason Grade Group (GG) two cancer on RARP, one had GG 3, two had GG 4, and 1 had GG 5.
"These results demonstrate the clinical value of QT's low frequency transmitted sound volography as a high-resolution imaging modality. We are encouraged by the continued high performance of QT imaging, especially in general anatomic and body imaging," said John Klock, MD, CEO and CMO at QT Imaging.
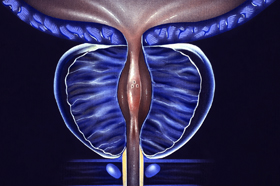
According to the abstract, “Low frequency transmitted ultrasound volography, previously shown to have high sensitivity for the diagnosis of breast cancer, provides 360-degree submillimeter-resolution imaging for tissue characterization and cancer detection even in the presence of bone and air, and with limited view tomographic data. In this study, we sought to validate this technique for detection of prostate cancer by imaging ex vivo whole prostate specimens after radical prostatectomy, comparing lesion detection and visualization with low-frequency-transmitted ultrasound volography with mpMRI, and correlating imaging findings with wholemount histopathology.”