Key Steps Toward Climate-Resilient Imaging
Introduction
Climate change refers to long-term shifts in temperatures and weather patterns, primarily driven by human activity, notably the burning of fossil fuels (coal, oil, and gas).1 1 The “triple planetary crisis” of climate change, biodiversity loss, and air pollution is a health crisis with significant direct and indirect adverse impacts on human health and on the resiliency of the health care system.2 As discussed in the previus issue of Applied Radiology , planetary health is the concept that human well-being over the long term depends on clean air, clean water, healthy soil, and the well-being of all living and nonliving systems.3
The health care sector is responsible for approximately 5% of total global greenhouse gas (GHG emissions and 8.5% of GHG emissions in the US. As a substantial contributor to the climate crisis and environmental degradation, the health care sector faces increasing pressure to minimize waste and emissions associated with health care delivery while being simultaneously stressed by the impacts of extreme weather events. Medical imaging is estimated to be responsible for up to 1% of global GHG emissions and 20% of total health care emissions.4 The need for change is urgent. As global health care systems set net-zero targets, radiology is well positioned to lead low-carbon, high-quality, transformative health care initiatives.
Planetary Health Care in Radiology
While the previous Global Health column introduced radiology’s roles in planetary health, here we take a closer look at how the following 3 sustainability principles by MacNeill et al can help position radiology on a promising course toward low-carbon, high-quality care5 ( Figure 1 ):
-
Reduce the demand for resource-intensive hospital care.
-
Provide the right care to the right patient at the right time.
-
Reduce emissions and the environmental impact of medically necessary health care.
Planetary health care framework for environmentally sustainable radiology.
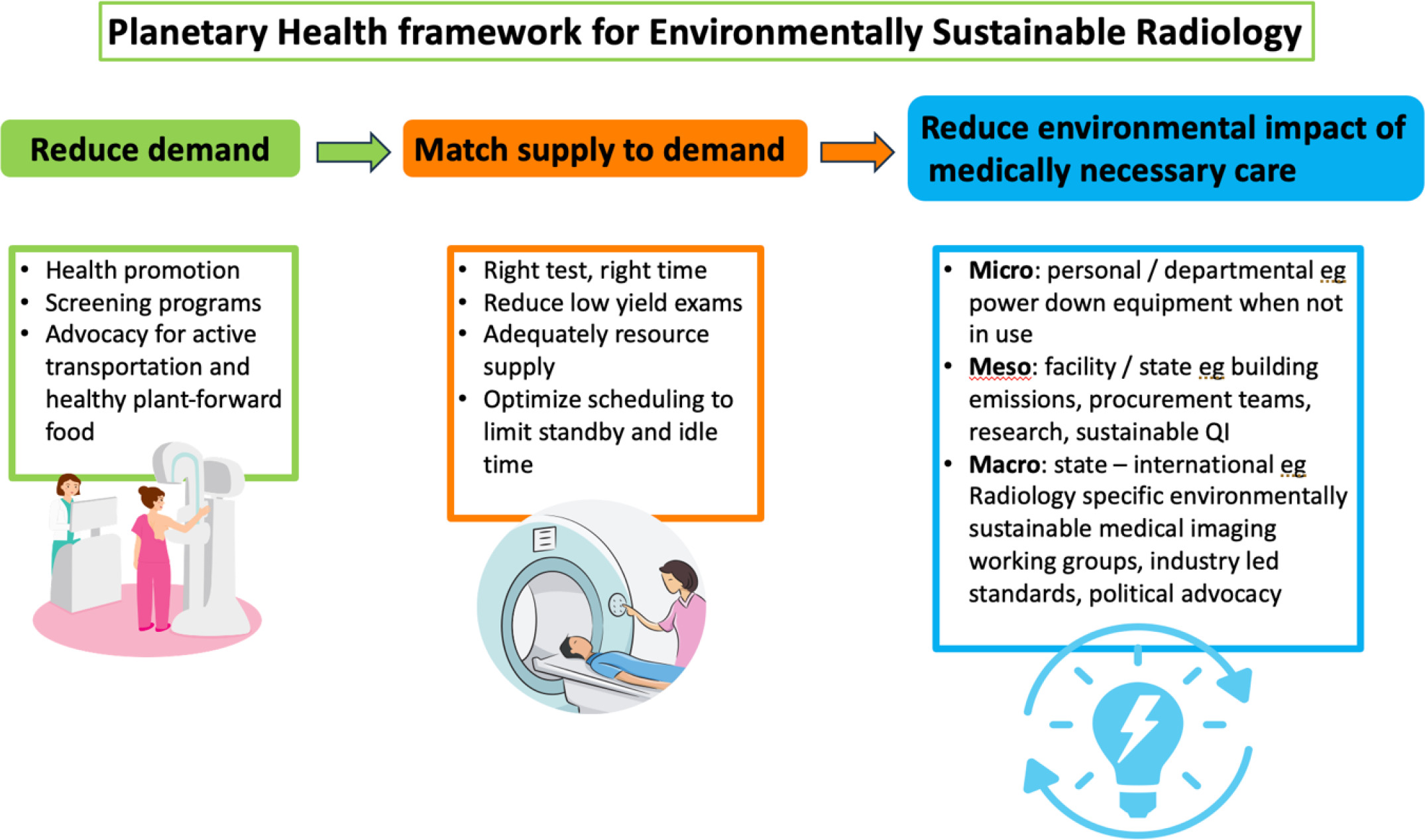
Reduce Demand
The first principle emphasizes that reducing the demand for resource-intensive hospital care is achievable through a strong focus on primary and preventive care.6 Many health care systems operate in a reactive manner, providing care in response to illness. This is both costly and resource-intensive as hospital care accounts for 36% of all health care emissions.7
While hospital care is essential, prioritizing health promotion, addressing social determinants of health, and expanding patient-centered primary care can enhance population health. This approach reduces the burden and severity of disease, while reducing the environmental footprint of the health care sector.
Access to robust screening programs plays a crucial role in early disease detection. For instance, screening mammography is an important tool for reducing the incidence of late-stage breast cancer. Treatment costs, intensity, and duration of care are significantly higher for late-stage breast cancer diagnoses.8
Match Supply to Demand
The second principle is to align supply to demand by ensuring the right care is provided at the right time, avoiding over- or underutilization of health care resources.6 In radiology, this involves reducing low-value imaging exams and enhancing the efficiency of available resources. Avoiding unnecessary investigations and treatment requires broad stakeholder engagement including collaboration with referring clinicians and patient partners. Clinical decision support tools such as Choosing Wisely and those provided by the American College of Radiology offer valuable guidance and patient education resources.9 - 11 It is essential to avoid delays in medically necessary imaging tests as this may result in later presentation with more advanced disease and ultimately require more resource-intensive, in-hospital care.
Inefficient use of resources in diagnostic imaging may occur when medical imaging equipment remains idle due to scheduling gaps. Instead, optimizing staff and patient scheduling to reduce scanner idle time between patients can reduce scanner-on time for the same workload per scanner. The transformation to low-carbon, climate-resilient medical imaging requires patient-centered resource allocation prioritizing health and well-being, thereby improving access and health equity.6
Reduce the Environmental Impact of Medically Necessary Care
The third principle is to reduce the environmental impact of medically necessary care.
Opportunities for low-carbon, high-quality diagnostic imaging are present at the micro (radiologist), meso (department, facility, or regional), and macro (state, federal, or international) levels ( Figure 2 ).12
Opportunities to reduce emissions and waste in medical imaging at the micro (personal), meso (department/facility), and macro (state, federal, or international) levels.
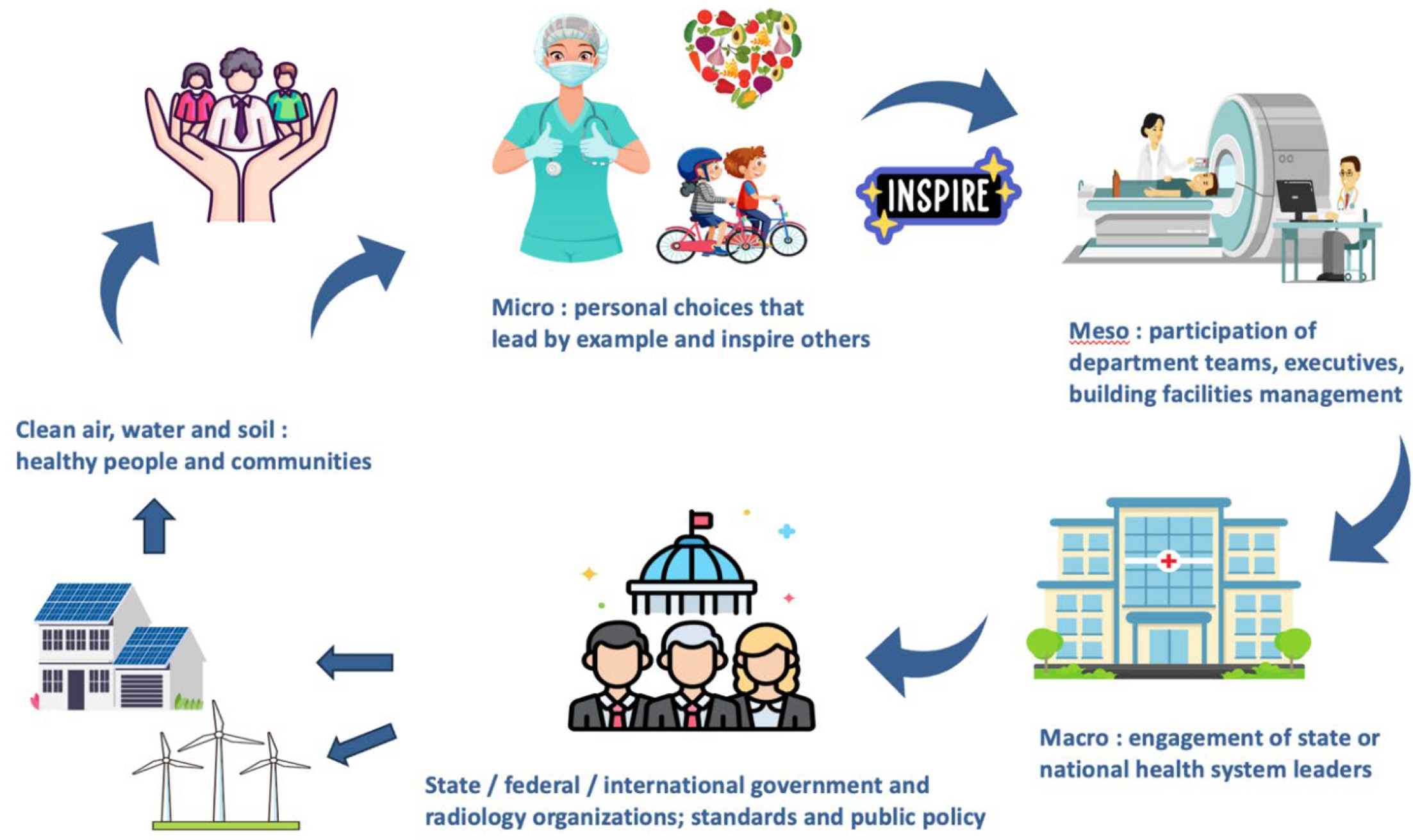
Micro-level actions include personal choices to reduce one’s carbon footprint, such as cycling to work or making plant-forward food choices, as well as leading departmental initiatives to power off medical imaging equipment during non-operational hours.13
Meso-level actions at the facility or regional level may include participation on procurement teams to ensure sustainability criteria are included in requests for proposals and advocating for procurement teams to support the principles of the circular economy. Radiologists can support purchase of refurbished medical imaging equipment, which significantly reduces production-phase (raw materials to delivery) emissions.14 The technical guide to Good Refurbishment Practice provides frameworks for safe use of refurbished medical imaging equipment. Additional opportunities may include advocacy for hybrid or virtual meetings and conferences, or organizational work-from-home policies. Research and sustainable quality improvement are essential. As new artificial intelligence (AI) tools evolve that shorten protocols, saving time and money, and improving patient experience, it will be essential to measure their benefits against the increased energy use and data storage requirements associated with AI.15
Macro-level actions may include engagement with state, national, and international organizations to endorse low-carbon, sustainable health care, or joining environmentally sustainable medical imaging working groups in university, state, or national organizations. This may include participating in grassroots efforts such as Radiologists for a Sustainable Future or the task force on climate change and sustainability by the American College of Radiology.16
Available national and international resources include the industry-led European Coordination Committee of the Radiological, Electromedical and Health care IT Industry, and governmental agencies such as the US Environmental Protection Agency, which have developed criteria for the environmental sustainability and energy efficiency of medical imaging equipment.17, 18
Conclusion
Climate change is a continuing threat to local, regional, and international human health and well-being. As an important new tool, climate-resilient imaging can advance patient-centered care and improve access to imaging overall. Fortunately, radiologists are well positioned within the health care system to engage others and to lead the transition to net zero health care.
References
Citation
Brown M, MHA. Key Steps Toward Climate-Resilient Imaging. Appl Radiol. 2024;(6):24 - 27.
doi:10.37549/AR-D-24-0042
December 1, 2024