Intraperitoneal Focal Fat Infarction of the Lesser Omentum
Images


CASE SUMMARY
A 56-year-old presented to our emergency department complaining of persistent epigastric pain of 48 hours’ duration. The patient had no fever, nausea, vomiting, or diarrhea. The patient’s personal and family medical history were unremarkable. On physical examination epigastric rebound tenderness was noted, indicating peritoneal irritation. Blood tests were significant for a normal white blood cell count of 10440/mm3 (neutrophils 72.2%), a mildly elevated C-reactive protein (CRP) level of 15.42 mg/L, and a mildly elevated serum lactate of 22mg/dl.
IMAGING FINDINGS
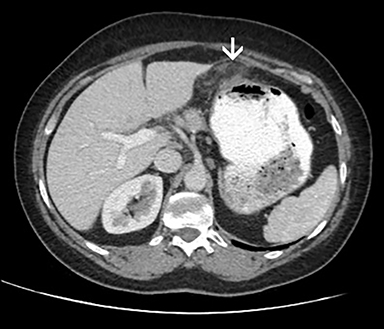
Contrast-enhanced CT with oral water-soluble contrast was performed to assess for gastrointestinal perforation and peptic ulcer disease. This was combined with CT angiography (CTA) of the mesenteric vessels to assess for mesenteric ischemia. The CTA was normal (Figure 1). No pneumoperitoneum, ascites, or extraluminal oral contrast were noted. No other CT findings indicative of peptic ulcer disease or gastrointestinal perforation (eg, mucosal discontinuity, hump, foreign body) were observed. No enlarged lymph nodes were evident.
However, a localized, slightly edematous, ovoid, fatty lesion with central radiating, hyperattenuating streaks was detected between the gastric body and the left hepatic lobe. Multiplanar reconstructions confirmed the presence of these fairly circumscribed inflammatory changes, at the expected location of the gastrohepatic ligament (Figure 2).
DIAGNOSIS
Intraperitoneal focal fat infarction of the lesser omentum
DISCUSSION
Intraperitoneal focal fat infarction (IFFI) is a rare condition that may present with acute or subacute abdominal pain.1 The term was introduced to group numerous entities with focal intraabdominal adipose tissue ischemia and/or necrosis as the common pathogenetic mechanism---torsion of epiploic appendages, infarction of the greater omentum and, rarely, the lesser omentum. They all share similar symptomatology, laboratory findings, and imaging features, and are all associated with a benign prognosis.2
Clinical manifestations are often nonspecific, consisting mainly of localized abdominal pain with rebound tenderness, indicating peritoneal irritation. Laboratory tests may reveal mildly raised inflammatory markers (white blood cell count and CRP).3 In our case, mildly elevated serum lactate was also noted, a finding that prompted CTA.
Related to abdominal pain localization, initial differential diagnoses to consider in a clockwise distribution, include: appendicitis and cholecystitis (right-sided pain), peptic ulcer disease and gastrointestinal perforation or ischemia (midabdominal area and epigastrium), splenic infarction (left-sided pain), and diverticulitis and pelvic inflammatory disease (left-sided and low abdominal pain).4,5
In this setting, CT is the initial modality of choice to exclude acute/surgical pathology requiring urgent treatment and to establish the presence of omental disease.6 Multiplanar reconstructions are valuable to demonstrate the extent of the process. The imaging protocol may be adjusted to reflect the differential diagnostic considerations, including the addition of vascular imaging, as in our case.7
The lesser omentum consists of the gastrohepatic and hepatoduodenal ligaments.8 The former extends from the lesser curvature of the stomach to the inferior surface of the liver, while the latter extends from the proximal duodenum to the porta hepatis. Blood vessels and lymphatics are enveloped within two sheets of peritoneal membrane in a variable amount of adipose tissue.8 IFFI of the lesser omentum and adipose tissue about the stomach has been referred to as perigastric appendagitis.9
CT features indicative of IFFI of the lesser omentum may range from mild stranding of the adipose tissue, to edematous, mass-like changes or swirling haziness around a central vessel, the “whirl” sign, a finding indicative of omental torsion.8,9 Ultrasonographic changes are usually subtle, mainly consisting of nonspecific echogenic fatty changes and therefore may miss the final diagnosis, given the low awareness of this entity.
Therapeutic management is debatable, owing to the lack of comparative studies and insufficient data. Some advocate exploratory laparotomy and others opt for conservative treatment with analgesics, anti-inflammatory medication, and fluid replacement unless there is a clinical deterioration. Recent literature questions the need for surgery in order to avoid unnecessary cost and perioperative morbidity. Deterioration of symptomatology or laboratory markers warrants surgical exploration.10
CONCLUSION
IFFI of the lesser omentum can present with severe epigastric pain mimicking an acute abdomen. Epiploic appendagitis, omental torsion, and omental infarction represent the spectrum of IFFI, share similar pathophysiological etiology, and are rare causes of acute abdominal pain. Watchful waiting is generally considered safe and appropriate. Imaging serves to exclude surgical pathology, to suggest the diagnosis, and to guide management to avoid unnecessary invasive treatment. Radiologists should be aware of this entity and the distinct imaging features consistent with fat inflammation in the distribution of the gastrohepatic and hepatoduodenal ligaments.
REFERENCES
- van Breda Vriesman AC, Lohle PN, Coerkamp EG, Puylaert JB (1999) Infarction of omentum and epiploic appendage: diagnosis, epidemiology and natural history. Eur Radiol. 9(9):1886-92.
- Coulier B, Van Hoof M. Intraperitoneal fat focal infarction of the lesser omentum: case report (2004) Abdom Imaging. 29 (4): 498-501. doi: 10.1007/s00261-003-0140-9
- Park TU, Oh JH, Chang IT, Lee SJ, Kim SE, Kim CW, Choe JW, Lee KJ (2012) Omental Infarction: Case Series and Review of the Literature. J Emerg Med, 42(2):149-54. doi: 10.1016/j.jemermed.2008.07.023
- Tonerini M, Calcagni F, Lorenzi S, Scalise P, Grigolini A, Bemi P (2015). Omental infarction and its mimics: imaging features of acute abdominal conditions presenting with fat stranding greater than the degree of bowel wall thickening. Emerg Radiol, 22(4):431-6. doi: 10.1007/s10140-015-1302-0
- Kamaya A, Federle MP, Desser TS (2011). Imaging Manifestations of Abdominal Fat Necrosis and Its Mimics. Radiographics, 31(7):2021-34. doi: 10.1148/rg.317115046.
- Puylaert JB (1992) Right-sided segmental infarction of the omentum: clinical, US, and CT findings. Radiology, 185:169–72.
- Naffaa L, Shabb N, Haddad M (2003). CT findings of omental torsion and infarction. Clin Imaging, 27(2):116-8.
- Yoo E, Kim JH, Kim MJ, Yu JS, Chung JJ, Yoo HS, Kim KW (2007). Greater and Lesser Omenta: Normal Anatomy and Pathologic Processes. RadioGraphics, 27(3):707-20.
- Justaniah AI, Scholz FJ, Katz DS, Scheirey CD (2014). Perigastric appendagitis: CT and clinical features in eight patients. Clin Radiology, 69(12):e531-7.
- Itenberg E, Mariadason J, Khersonsky J and Wallack M (2010). Modern Management of Omental Torsion and Omental Infarction: A Surgeon’s Perspective. J Surg Educ, 67(1):44-7. doi: 10.1016/j.jsurg.2010.01.003.
Citation
A K, A S, K P, M K. Intraperitoneal Focal Fat Infarction of the Lesser Omentum. Appl Radiol. 2021;(2):48C-48D.
March 11, 2021