Infarction of the territory of the Artery of Percheron
Images
CASE SUMMARY
A 69-year-old woman with a history of diabetes mellitus, paroxysmal atrial fibrillation, and hypertension presented to the emergency department following a fall. She developed progressively worsening encephalopathy. Alcohol/drug screen and lumbar puncture were negative. A CT scan demonstrated only a 3 mm subdural hematoma. The patient’s mental status quickly deteriorated and the patient was intubated and admitted to the ICU. On physical examination, the patient had symmetric nonreactive pupils, nonpurposeful movement of the left lower extremity more than the right, and diminished symmetric reflexes. An MRI of the brain was obtained. The patient’s mental status did not improve and decision was made to withdraw life support days later.
IMAGING FINDINGS
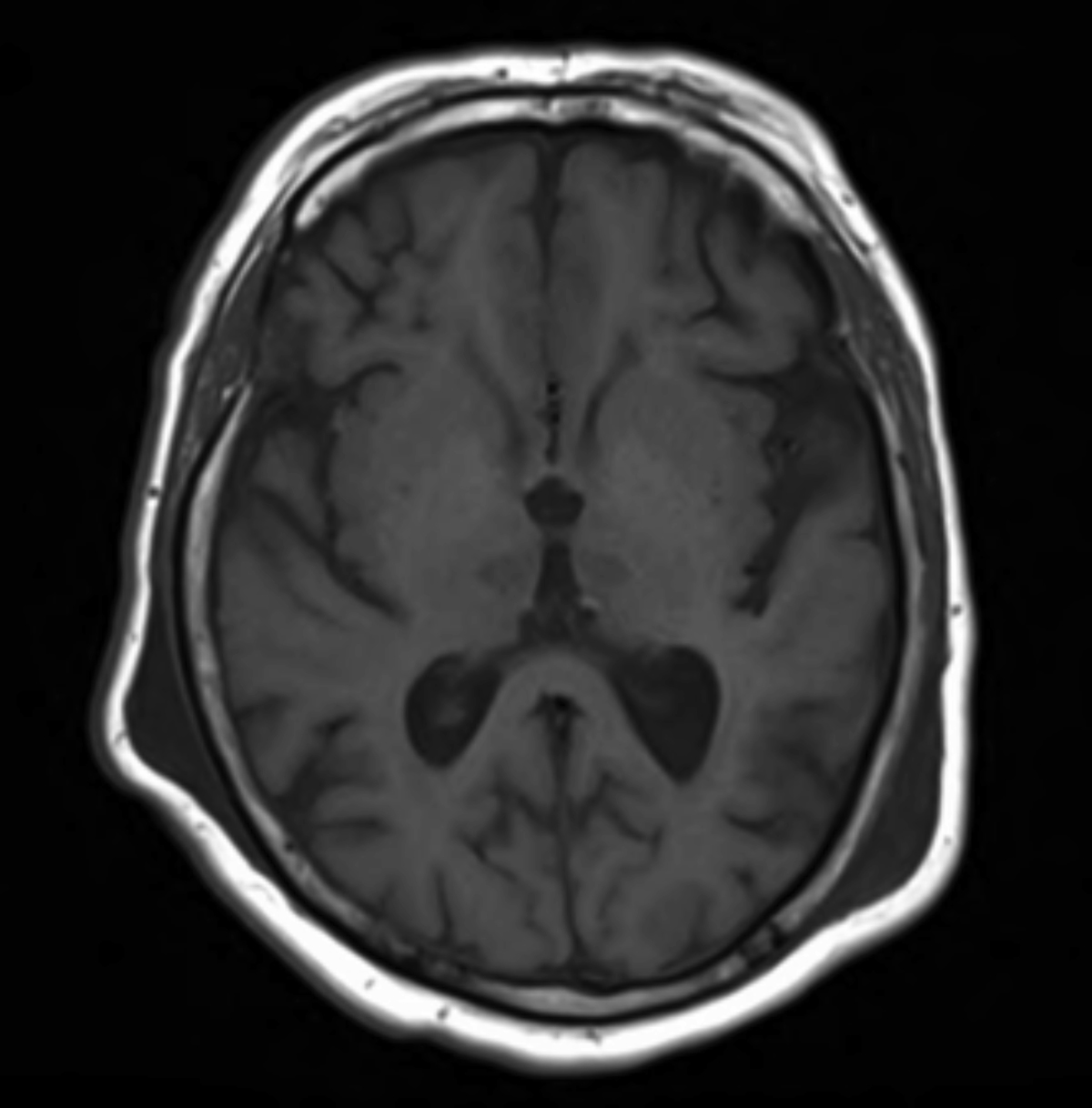
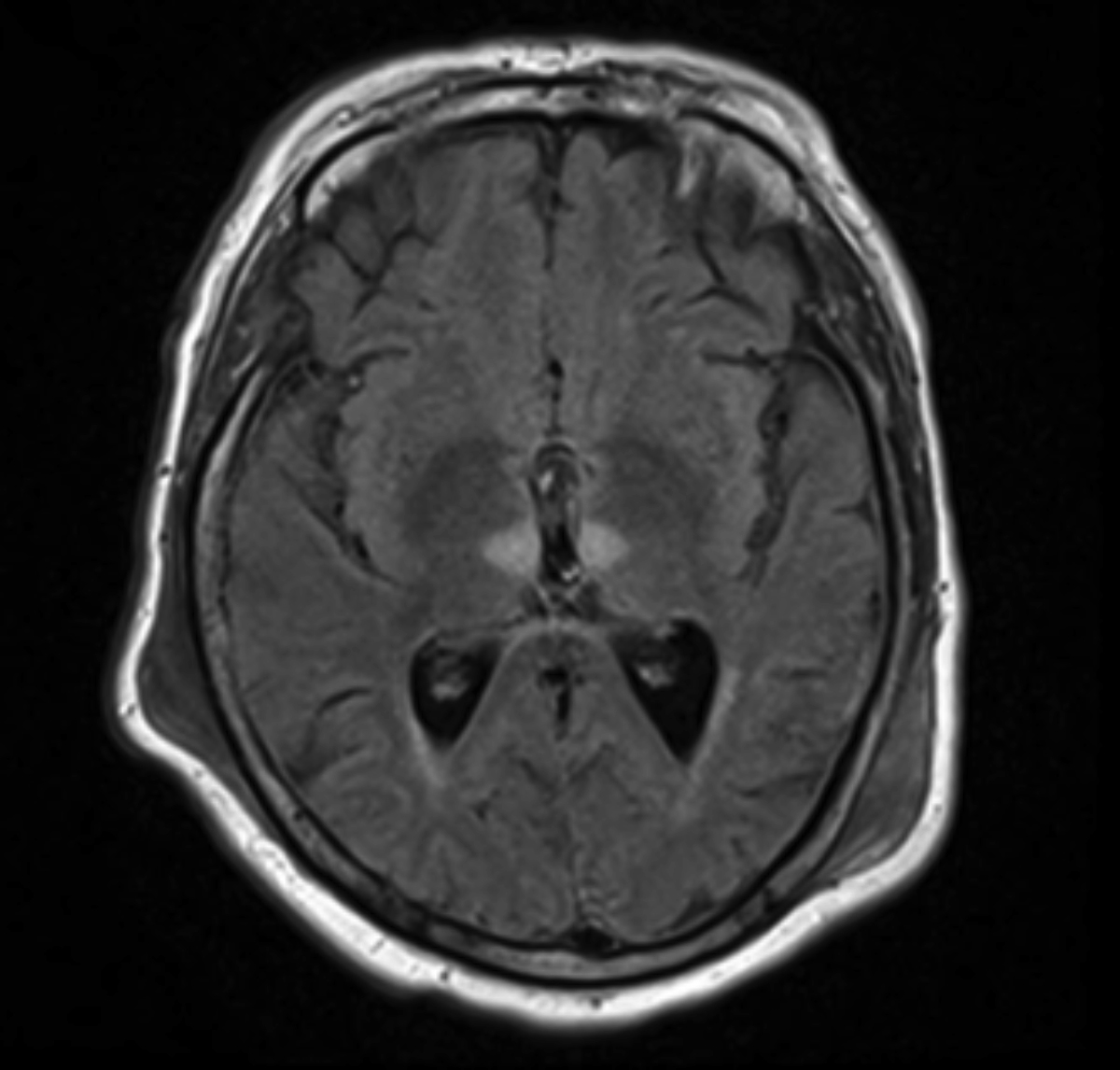
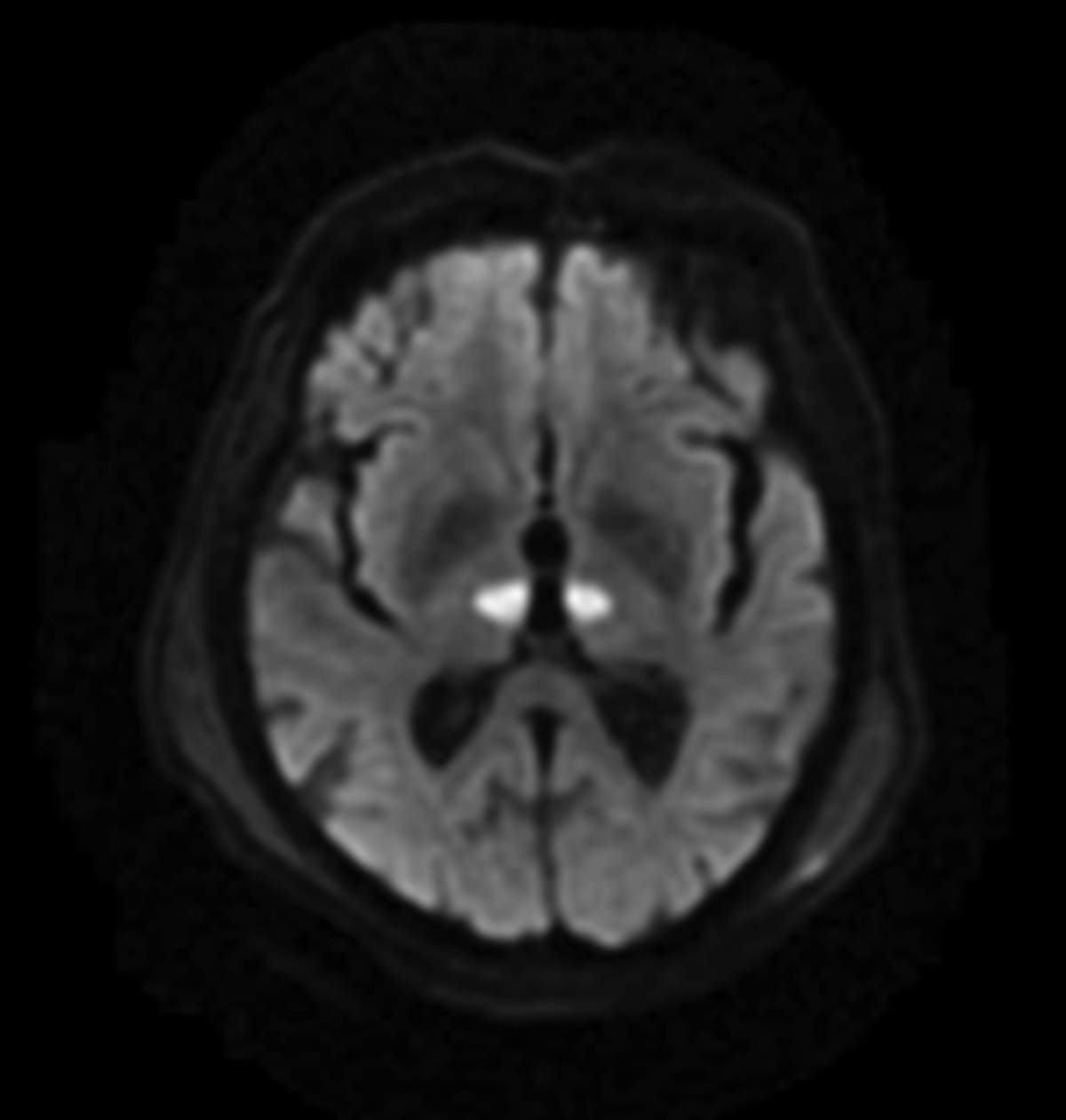
Symmetric T1 hypointensities/T2 Flair hyperintensities that demonstrate diffusion restriction in the bilateral paramedian thalami (Figures 1–3).
DIAGNOSIS
Acute ischemic infarction of the territory of Artery of Percheron (AOP)
DISCUSSION
The case described above demonstrates classic imaging findings of an ischemic stroke in the territory of the AOP, an anatomic variant. MR imaging demonstrated symmetric infarctions of the bilateral paramedian thalami. A concomitant small SDH from the patient’s fall was a not believed to be clinically significant.
The AOP is an uncommon anatomic variant in the blood supply to the thalamus.1 There are four principle regions of the thalamus: anterior (tuberothalamic), inferolateral, paramedian, and posterior choroidal.1,2 Thalamoperforators arise off the posterior cerebral arteries to supply the paramedian region of the thalamus bilaterally and extend to supply a portion of the rostral midbrain. Typically, each thalamic hemisphere has its own blood supply via these thalamoperforators.3,4 The AOP is an anatomic variant where a single trunk arises off of the P1 segment of the posterior cerebral artery to supply both paramedian hemispheres of the thalamus and/or rostral midbrain.1-3
An infarct of the AOP results in bilateral paramedian thalamic ischemia. Bilateral paramedian thalamic involvement is classically characterized by a triad of altered mental status, vertical gaze palsy, and memory impairment with or without coma.3 However, the presentation may vary as demonstrated in this patient. If the rostral midbrain is involved, oculomotor palsies, hemiplegia, and cerebellar ataxia can be seen.3,5
Brain MRI is the best early imaging modality and demonstrates abnormal signal intensities in the bilateral paramedian thalami. The bilateral and symmetric nature of this infarct may mislead the physician into investigating systemic or inflammatory causes in lieu of a vascular etiology.3 These often can be differentiated by clinical history if imaging alone is not definitive. Like all other ischemic infarcts, the hallmark of AOP territory infarction is T1 hypointensity, T2/FLAIR hypertintesity and diffusion restriction in the affected area. More specifically, a “V sign”—a distinct pattern of V-shaped hyperintensity on axial FLAIR and DWI sequences along the pia surface of the midbrain adjacent to the interpeduncular fossa—has been described in 67% of AOP cases.5 Nonetheless, 38% of AOP territory infarcts involve the paramedian thalami alone.5 There is little role for CT or MR angiography, as both modalities are usually ineffective for visualizing the AOP.3
Few prior studies have investigated the prevalence of the AOP in the general population. In one small autopsy study, the prevalence of the AOP variant was 11.7%.6 AOP infarcts are believed to represent 0.1 to 2% of all ischemic stroke.7,8 More specifically, this variant is involved in 4 to as many as 35% of thalamic ischemic strokes.5,9
CONCLUSION
The case describes an AOP territory infarction, an uncommon event with poor prognosis without early intervention. MR imaging demonstrates bilateral T1 hypointensitites, T2/FLAIR hyperintensities and diffusion restriction of the bilateral paramedian thalami. AOP infarcts are unique in their bilateral, symmetric nature and can be mistaken for a systemic, rather than a vascular process.
References
- Sandvig A, Lundberg S, Neuwirth J. Artery of Percheron infarction: a case report. Journal of Medical Case Reports. 2017; 11:221.
- Schmahmann JD. Vascular syndromes of the thalamus. Stroke. 2003;34(9):2264-2278.
- Amin OS, Shwani SS, Zangana HM, Hussein EM, Ameen NA. Bilateral infarction of paramedian thalami: a report of two cases of artery of Percheron occlusion and review of the literature. BMJ Case Rep. 2011;2011.
- Percheron G. The anatomy of the arterial supply of the human thalamus and its use for the interpretation of the thalamic vascular pathology. Z Neurol. 1973;205(1):1-13.
- Lazzaro NA, Wright B, Castillo M, et al. Artery of percheron infarction: imaging patterns and clinical spectrum. AJNR Am J Neuroradiol. 2010;31(7): 1283-1289.
- Kocaeli H, Yilmazlar S, Kuytu T, Korfali E. The artery of Percheron revisited: a cadaveric anatomical study. Acta Neurochir (Wien). 2013;155(3): 533-539.
- Carrera E, Michel P, Bogousslavsky J. Anteromedian, central, and posterolateral infarcts of the thalamus: three variant types. Stroke. 2004;35 (12):2826-2831.
- Pezzini A, Del Zotto E, Archetti S, et al. Thalamic infarcts in young adults: relationship between clinical-topographic features and pathogenesis. Eur Neurol. 2002;47(1):30-36.
- Arauz A, Patiño-Rodríguez HM, Vargas-González JC, et al. Clinical spectrum of artery of Percheron infarct: Clinical-radiological correlations. J Stroke Cerebrovasc Dis. 2014;23(5):10838.
- Rodriguez EG, Lee JA. Bilateral thalamic infarcts due to occlusion of the Artery of Percheron and discussion of the differential diagnosis of bilateral thalamic lesions. J Radiol Case Rep. 2013;7(7):7-14.
Citation
A S, ZE S, A U,. Infarction of the territory of the Artery of Percheron. Appl Radiol. 2019;(2):34-35.
March 28, 2019