Improving Body Imaging Throughput in the Midst of COVID-19
Images
At the onset of the COVID-19 pandemic in the United States, many elective procedures and non-urgent ambulatory visits were rescheduled to comply with stay-at-home orders and to ensure patient and staff safety. This has created a significant backlog of patients who need service at many clinics and outpatient centers in the coming months. Hospital ambulatory clinics and radiology waiting rooms are typically crowded and not set up to facilitate physical distancing; limiting schedules severely hampers patient throughput and adversely affects ability to provide timely care and address these backlogs. In addition, many patients currently avoid hospitals for fear of contracting the virus. With COVID-19 cases not yet significantly abating in many areas, the question arises whether radiologists can safely and efficiently care for patients until a vaccine for COVID-19 is widely available.
Here we will discuss our experience using fast MRI body imaging protocols in combination with strategic use of free-standing facilities to safely reduce our patient backlog and manage our MR imaging load.
Fast MR Imaging: Rationale for Use
In the setting of the COVID-19 pandemic and significant patient backlogs, shortening MRI protocols to relieve backlogs and minimize potential COVID-19 exposure to patients and staff seems logical, particularly with respect to vulnerable populations. However, faster patient turnaround risks undesirable overcrowding of MRI and hospital outpatient waiting areas.
Many hospital systems have affiliated free-standing outpatient imaging centers in proximity to residential areas, thus providing easy access for patients. Parking tends to be more common at ground level and readily accessible to the facility entrance. Patients may also feel more comfortable at smaller facilities, which can provide a friendlier, “non-hospital”’ environment, decrease the stress on large hospital outpatient waiting areas, and allay any fears patients might have with regard to satisfactory physical distancing measures. Free-standing imaging centers often have a smaller footprint, allowing for nimble operational changes and facilitating physical distancing. It is also faster to test fast scanning protocols in a small number of scanners at free-standing imaging centers instead of attempting to implement them across an entire hospital system. Several of our suggested solutions allow for safer, more expeditious patient throughput, which is key for the effective application of fast MRI protocols to help reduce patient backlog.
Fast MRI Effectiveness
The growing trend toward more patient-centered health care has challenged radiologists to assess MRI protocols more critically, with an emphasis on efficient and fast protocols.1 Fast (also called rapid, focused, or abbreviated) MRI protocols offer an alternative to standard protocols for answering specific clinical questions, potentially improving workflows, addressing imaging demand, and reducing costs, all without sacrificing patient safety.
Several retrospective studies have shown the effectiveness of fast MRI for HCC screening.2-7 Nougaret, et al, for example, reported that contrast-enhanced scans did not provide additional information over unenhanced scans of pancreatic cystic lesions.8 Short protocols have also been proposed for other procedures, such as screening the adrenal glands, kidneys, and female pelvis.1 Seo, et al proposed using MR enterography to evaluate small-bowel inflammation in Crohn disease with non-enhanced diffusion weighted imaging (DWI).9 Kang, et al evaluated 10 studies and found no significant differences in specificity or sensitivity between bi-parametric and multi-parametric MRI scans for prostate cancer evaluation.10 Short, specific protocols have been proposed for breast MRI screening and assessment of breast lesion size.11-13 Ross, et al showed high sensitivity and specificity for hip and pelvic fractures using an abbreviated MRI protocol.14 Khurana, et al showed similar results with a short MRI protocol to evaluate hip pain in the emergency room setting.15
Planning Fast MRI Implementation
Our healthcare system consists of hospital, outpatient, and free-standing clinics, with imaging equipment acquired from three MRI vendors. Therefore, a free-standing imaging center and a limited number of scanners of similar generation and vendor were key to effective and efficient rollout of fast body MR imaging.
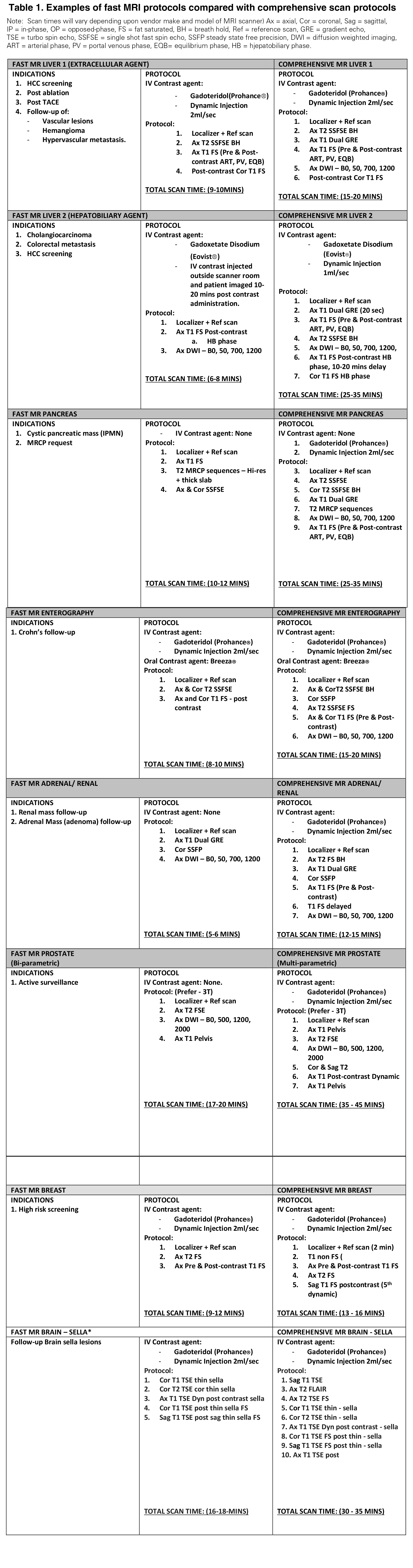
To begin, we created an ad hoc group to rapidly conceive and implement a fast MR scanning program. An experienced radiologist from each imaging section reviewed the literature and proposed feasible protocols. Whenever possible, more frequently used comprehensive MRI protocols were converted to fast MRI protocols. Each of these protocols was then vetted by each section and the MRI imaging modality group (Table 1, online at http://appliedradiology.com/articles/improving-body-imaging-throughput-in-the-midst-of-covid-19). We established the following inclusion and exclusion criteria for fast body MRI protocols:
Inclusion Criteria
- Prior good quality baseline MRI scan in the PACS as a reference scan;
- As a follow up scan of a pre-existing medical condition; and
- Scan indication is a focused clinical question; eg, is the tumor bigger or smaller, was locoregional therapy effective, or was there tumor recurrence or new metastasis?
- Exclusion criteria
- Request for lesion characterization;
- Work-up of findings seen on other imaging modalities;
- Specific request for standard MRI study.
Fast MRI Practices
Patient Access
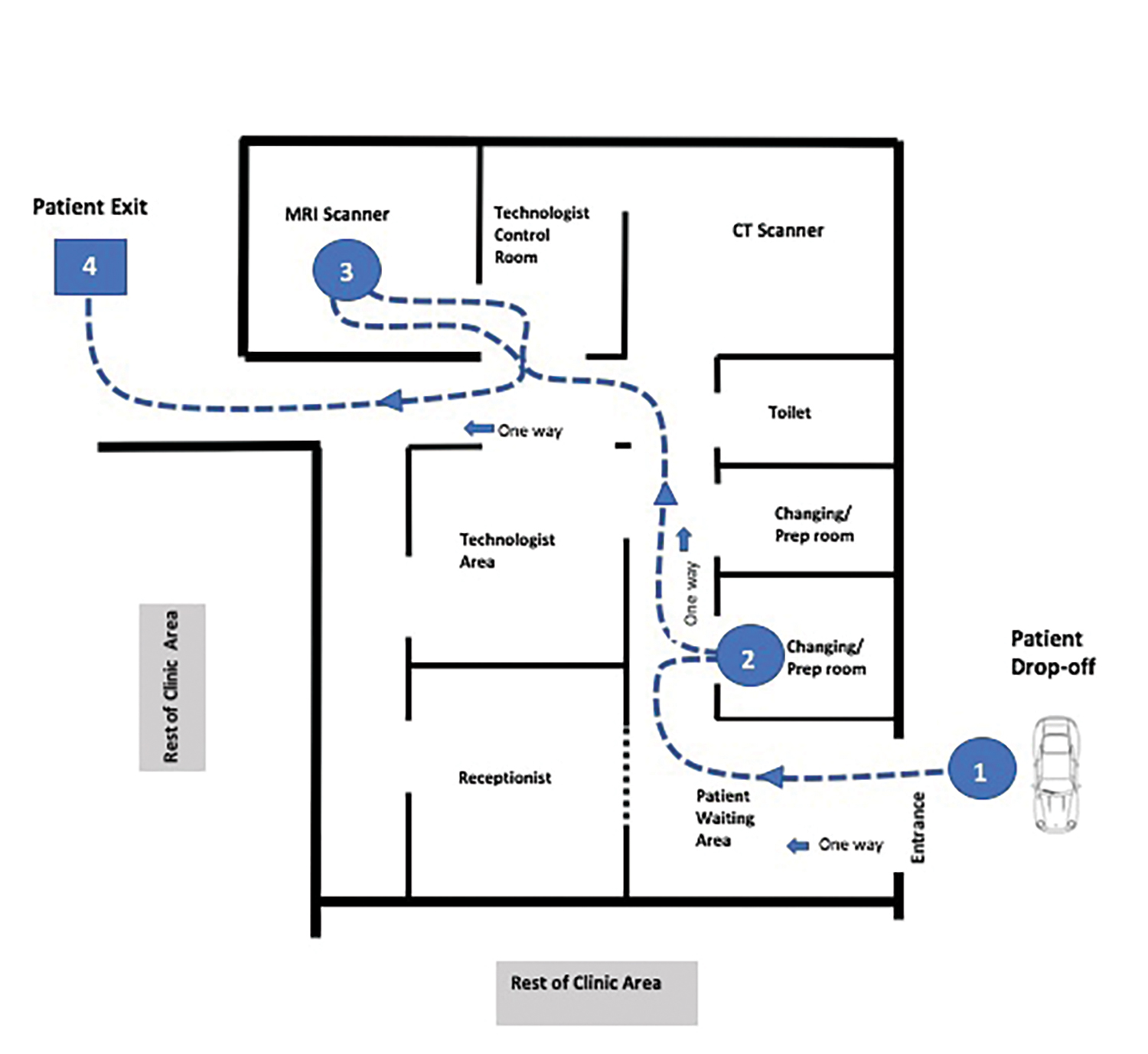
All patients were asked to comply with masking and were screened for signs/symptoms of illness in advance of and upon arrival for their appointment (Figure 1). Waiting room seating was configured to maintain a distance of 6 feet between patients. To minimize use of waiting areas, patients who arrived by automobile were asked to wait in their car until called for scanning. Our health system is implementing a patient texting platform, which is expected to further expedite this process. If necessary for an exam, oral contrast was delivered to the patient’s vehicle. Cashless co-payment procedures and devices prevented contact with registration staff.
Facility Changes
Physical barriers created a six-foot perimeter around the MRI console; no one was allowed within that zone while it was occupied by a technologist. An MRI technologist oversaw and maintained a clean and safe environment in all work areas. The scanner room was cleaned with hospital-grade germicidal wipes between each procedure. High-contact surfaces (eg, doorknobs, locker handles) were also cleaned with these wipes. All used linens were removed and disposed of appropriately. Restroom signs indicated occupancy. Patients were prepped in designated areas, further limiting contact with other patients and staff. Entry and exit of patients were regulated as much as possible through a “one-way-only” system. Arrow markers on the floors and walls helped facilitate this system.
Personal Protective Equipment and Other Protection Measures
All staff were provided with personal protective equipment (PPE). Owing to resource limitations, more extensive PPE was used for COVID-19-positive patients or patients under investigation for the disease, while standard universal protection measures were implemented for other patients. Staffing of these sites was important to manage the increase in patient volume and to provide safety for patients and staff. Whenever possible, two teams of technologists alternated scanning patients, thus providing continuity of care. At least two prep rooms were also used to help patients prepare patients expeditiously.
Scanning Checklist
Protocols were tested and approved for use. An additional torso coil was also acquired to help speed patient throughput and case turnaround. Once completed, scans were automatically sent to the PACS system, without providing radiologists with the opportunity to check them or to add sequences. Hence, it was important that the scanning technologist closely adhere to the imaging parameters and review all images for screening and diagnostic quality. To facilitate this process, technologists were provided with a checklist (Appendix 1) to complete and scan into the PACS at the conclusion of each study.
Teamwork Is Vital
Since success in this endeavor required the support of our clinical colleagues, we consistently kept channels of communication open. For example, we established a list of patients whose tests were rescheduled because of stay-at-home orders. We designated radiologists in each imaging section to consult with referring physicians for approval of fast MRI protocols on a patient-by-patient basis. At every stage we made sure to involve all stakeholders, including MRI staff, imaging supervisors, administrators, and local technical applications support personnel. Including technologists on our task force facilitated their buy-in during the operational change process.
Implementation Challenges
Change often raises questions and challenges, especially with regard to implementing unconventional approaches to long-standing procedures. For example, some radiologists expressed their fear of missing findings and the accompanying medico-legal ramifications. We addressed this issue by having any patient who required more detailed imaging to return for a more comprehensive scan. Using a smaller facility, located apart from our main hospital, is not always ideal for patients with clinic visits at a different location on the same day. Working with the patient’s clinical team to coordinate appointment times helped us to prevent delays in patient care.
Scan Reimbursement
Institution-specific guidelines were created for assessing a limited charge modifier (CPT modifier 52) for billing of the fast MR protocols. For example, limited-charge modifiers may be appropriate for scanning procedures or room use lasting less than 10 minutes. Similarly, a limited-charge modifier may be considered if the protocol sequences do not fulfill the study recommendations put forth by the appropriate accrediting body (eg, The American College of Radiology). The application of the limited-charge modifier is largely at an institution’s discretion; many fast protocols will not require it, as they meet recommended guidelines. Indeed, the majority of fast protocols at our institution did not require the modifier. Billing can be nuanced, however, with regional and institutional variations based on payer mix, standard of care and, ultimately, the clinical question being answered.
Fast MRI Improves Throughput
At the start of this fast MRI protocol implementation, nearly half of our body imaging backlog studies were deemed eligible for fast protocols. By utilizing the resources of our free-standing imaging centers, the fast protocols enabled our facility to return to 90% of our average pre-COVID-19 MRI scans per day within one month of implementation. By comparison, our hospital-based outpatient facility MR imaging volume returned to only 57% of the pre-COVID-19 average.
Based on our experience, a thoughtful, well-planned execution of fast MRI protocols in smaller and more easily modified imaging facilities can potentially provide more efficient patient care and reduce scanning backlogs during the continuing COVID-19 pandemic. Indeed, these protocols may continue to be utilized beyond cessation of these conditions, pending assessment of radiologist, technologist, patient, and clinician satisfaction.
References
- Canellas R, Rosenkrantz AB, Taouli B, et al. Abbreviated MRI protocols for the abdomen. Radiographics 2019;39(3):744-758.
- Marks RM, Ryan A, Heba ER, et al. Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid–enhanced MRI for hepatocellular carcinoma surveillance. AJR 2015;204(3):527-535.
- Besa C, Lewis S, Pandharipande PV, et al. Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdom Radiol (NY) 2017; 42(1):179–190.
- Lee JY, Huo EJ, Weinstein S, et al. Evaluation of an abbreviated MRI screening protocol for patients at risk for hepatocellular carcinoma. Abdom Radiol (NY) 2018;43(7):1627-1633.
- Tillman BG, Gorman JD, Hru JM, et al. Diagnostic per-lesion performance of a simulated gadoxetate disodium-enhanced abbreviated MRI protocol for hepatocellular carcinoma screening. Clinical Radiology 2018 May; 73(5):485-493.
- Khatri G, Pedrosa I, Ananthakrishnan L, et al. Abbreviated-protocol screening MRI vs. complete-protocol diagnostic MRI for detection of hepatocellular carcinoma in patients with cirrhosis: an equivalence study using LI-RADS v2018. J Magn Reson Imaging 2020 Feb; 51 (2):415-425
- Vilgrain V, Esvan M, Ronot M, et al. A meta-analysis of diffusion-weighted and gadoxetic acid-enhanced MR imaging for the detection of liver metastases. Euro Radiol 2016; 26(12):4595-4615.
- Nougaret S, Reinhold C, Chong J, et al. Incidental pancreatic cysts: natural history and diagnostic accuracy of a limited serial pancreatic cyst MRI protocol. Eur Radiol 2014; 24(5):1020-1029.
- Seo N, Park SH, Kim K, et al. MR enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 2016;278(3):762-772.
- Kang Z, Min X, Weinreb J, Li Q, Feng Z, Wang L. Abbreviated biparametric versus standard multiparametric MRI for diagnosis of prostate cancer: a systematic review and meta-analysis. AJR 2019;212(2):357-365. doi: 10.2214/AJR.18.20103.
- Harvey SC, Di Carlo PA, Lee B, Obadina E, Sippo D, Mullen L. An abbreviated protocol for high-risk screening breast MRI saves time and resources. JACR 2016 Nov;13(11):R74-R80.
- Ko ES, Morris EA. Abbreviated magnetic resonance imaging for breast cancer screening: concept, early results, and considerations. Korean J Radiol 2019; 20(4):533-541. Published online 2019 Mar 11.
- Kim SY, Cho N, Choi Y, et al. Ultrafast dynamic contrast-enhanced breast MRI: lesion conspicuity and size assessment according to background parenchymal enhancement. Korean J Radiol 2020; 21(5):561–571. Published online 2020 Mar 31.
- Ross AB, Chan BY, Yi PH, Repplinger MD, Vanness DJ, Lee KS. Diagnostic accuracy of an abbreviated MRI protocol for detecting radiographically occult hip and pelvis fractures in the elderly. Skeletal Radiol 2019;48(1):103-108.
- Khurana B, Okanobo H, Ossiani M, Ledbetter S, Dulaimy KA, Sodickson A. Abbreviated MRI for patients presenting to the emergency department with hip pain. AJR 2012; 198(6):W581-W588.
Citation
JV T, KK P, SA W, A S, MB F, DE M, CL C.Improving Body Imaging Throughput in the Midst of COVID-19. Appl Radiol. 2020; (5):33-35.
September 1, 2020