Imaging Testicular Torsion
Images
Testicular torsion, or more accurately, spermatic cord torsion, is an important cause of an acute scrotum. Clinically, patients may present with any of the following symptoms: acute scrotal pain not relieved by scrotal elevation; scrotal swelling; absent cremasteric reflex; nausea; and vomiting. Radiologists play a critical role in the evaluation of the acute scrotum and must be able to recognize complete and incomplete testicular torsion.
Two types of testicular torsion with different peaks have been described. Extravaginal testicular torsion occurs primarily in utero or in neonates. Intravaginal testicular torsion is most common around 12 years of age but can occur at any age.1 The bell clapper anomaly is the primary risk factor for intravaginal torsion; the condition usually presents bilaterally and is estimated to occur in 12% of testes.2
The tunica vaginalis begins as the processus vaginalis, an outpouching of peritoneum. It surrounds the testis as it descends into the scrotum and then obliterates proximally. Normally, the tunica vaginalis attaches to the posterolateral aspect of the testis and covers only its anterior surface. In the bell clapper anomaly, the tunica vaginalis attaches to the spermatic cord abnormally high in the scrotum and completely encircles the epididymis, distal spermatic cord, and testis. Thus, these structures hang freely in the intravaginal space and can more easily twist and torse.
Testicular torsion can be complete (360° up to 1,080° [3 full turns]) or incomplete (less than 360°). The twist may be either clockwise or counterclockwise. The vascular twisting causes venous obstruction initially, followed by arterial obstruction and eventually testicular ischemia. Treatment consists of either manual or surgical detorsion. Salvage is more likely with earlier detorsion, decreasing from 90% salvage rate before 12 hours, to 54% between 13 and 24 hours, and to 18% beyond 24 hours.3 Imaging plays a crucial role in the timely and accurate diagnosis of testicular torsion. Treatment delays resulting from repeat imaging have been associated with increased risk of orchiectomy.4
Imaging Protocol
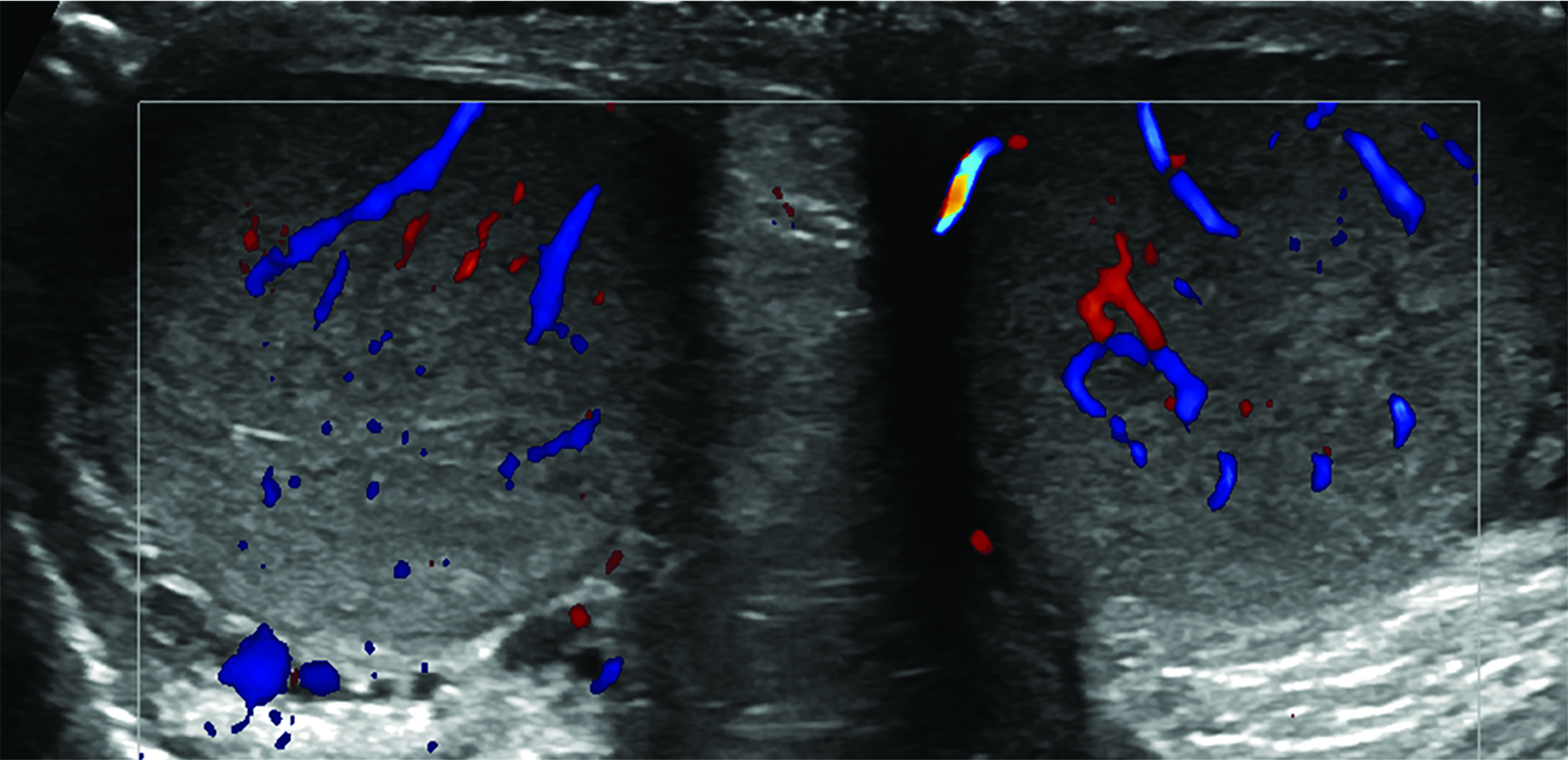
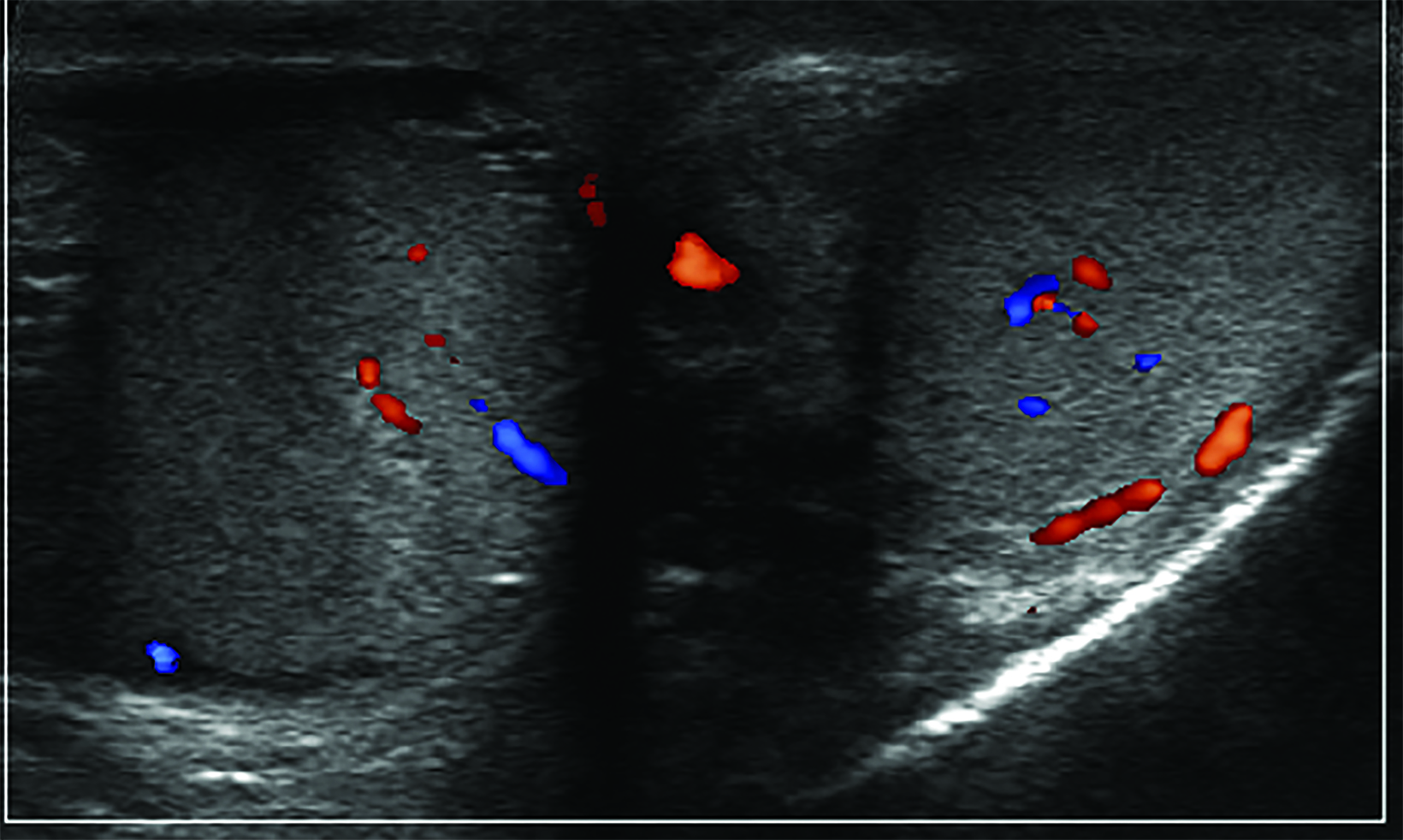
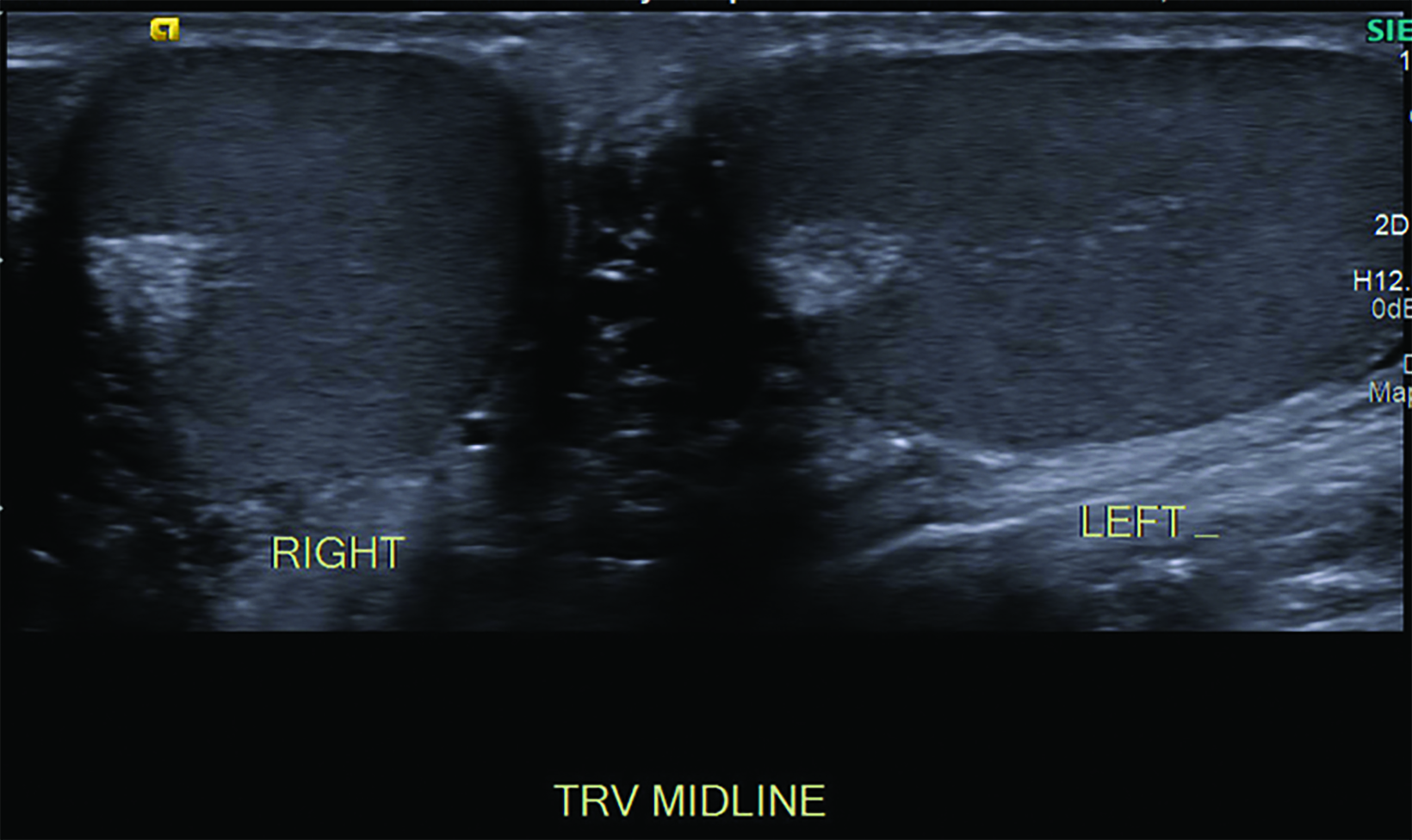
Color Doppler ultrasound is the modality of choice for investigating the acute scrotum. The scan is performed with a high-frequency linear-array transducer.5 The examination should begin with a side-by-side, short axis comparison (sometimes referred to as a buddy shot, sunglasses view, or saddle view) in grayscale and color Doppler. This view facilitates detection of subtle asymmetry in echotexture or color Doppler flow.
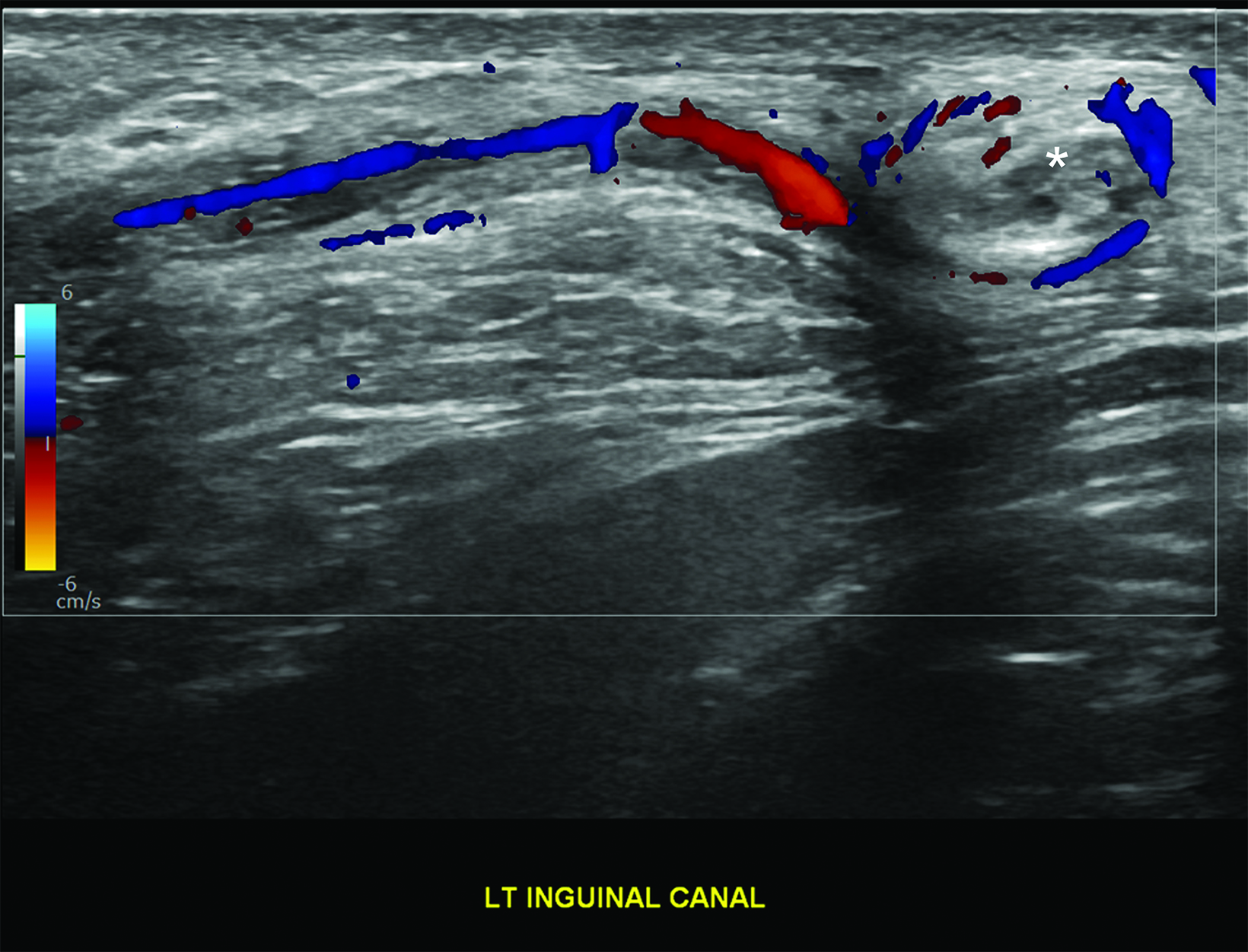
The examination should then proceed with imaging of the asymptomatic side first, permitting optimization of the focal zone, depth, grayscale gain, and Doppler parameters.5 These images will establish a baseline for comparison. Images of the upper, middle, and lower testicle should be obtained in the medial, middle, and lateral portions of the testis. Evaluation of the upper, middle, and lower epididymis should occur next. The exam of the asymptomatic side concludes with following the spermatic cord from the inguinal canal to the testis and is repeated on the symptomatic side.
Imaging Findings
Color Doppler Flow
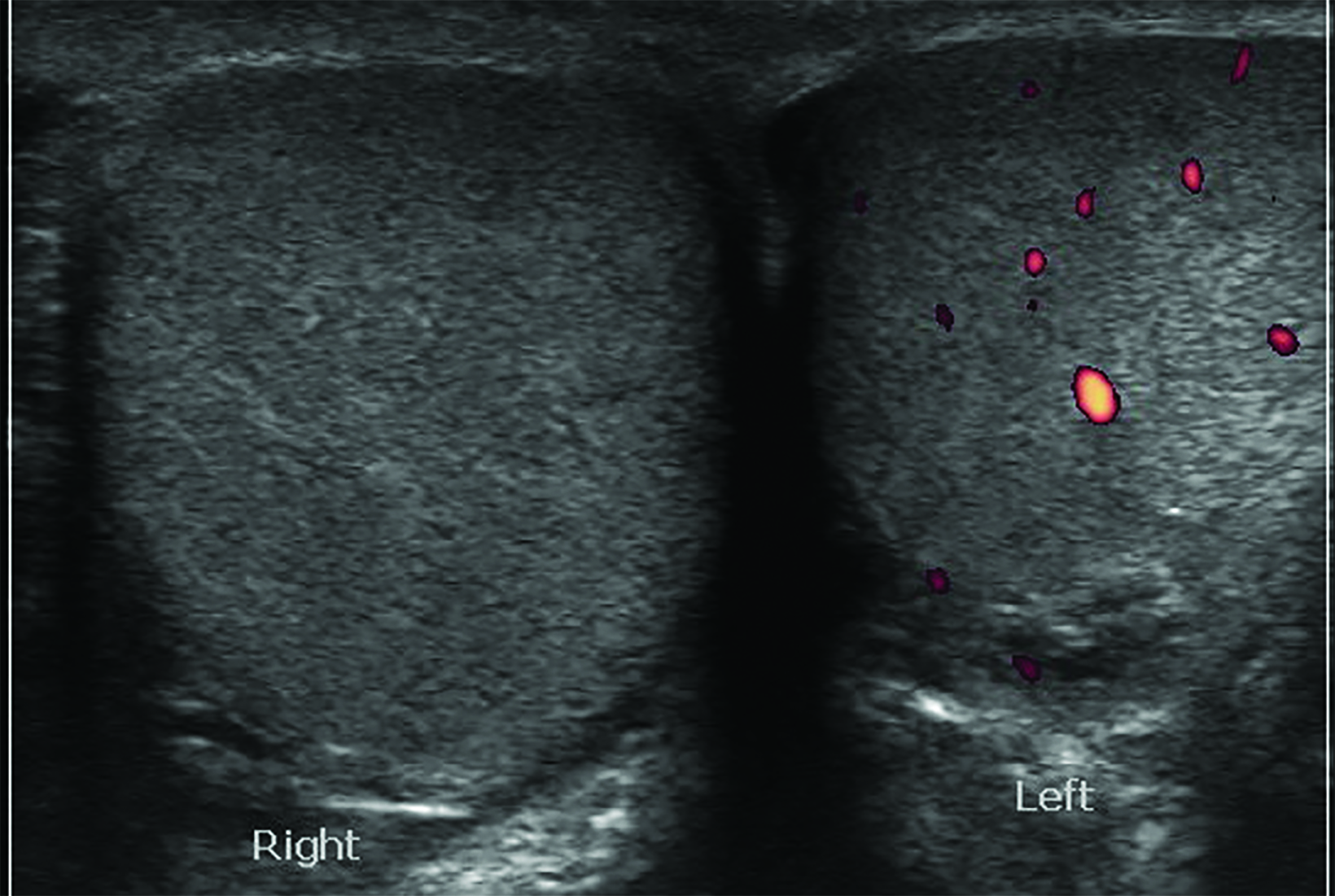
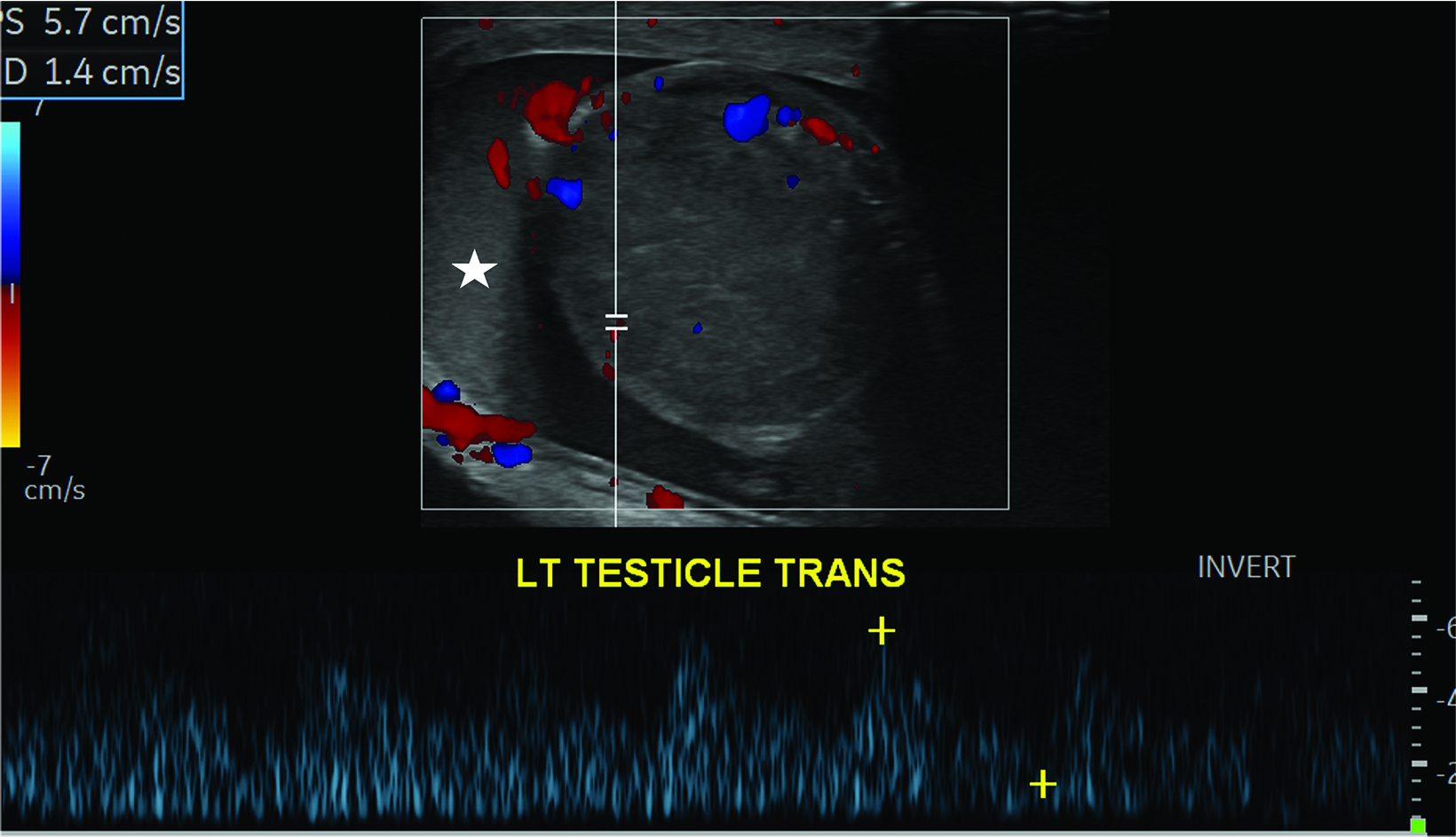
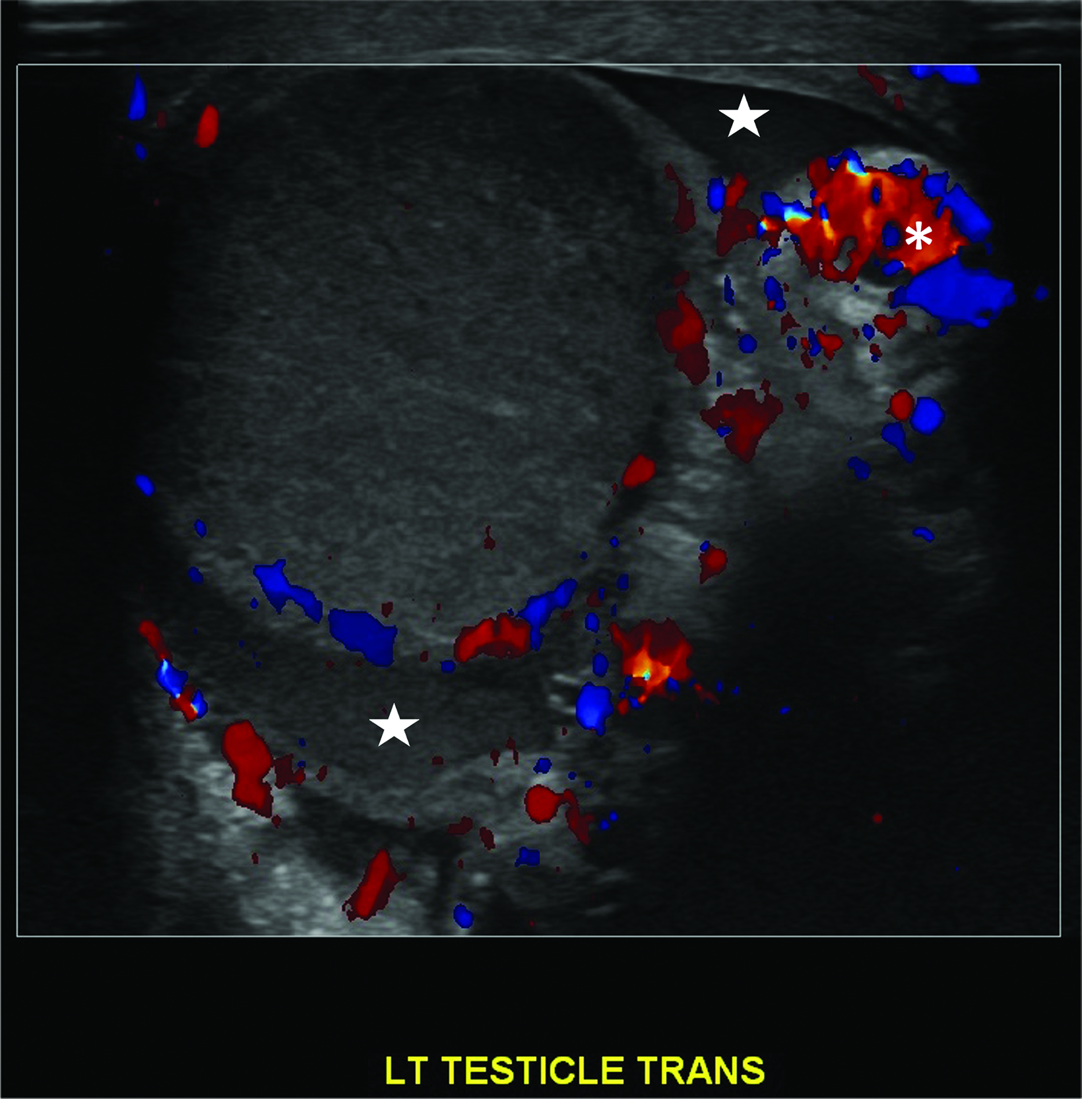
Absent or significantly reduced color Doppler flow in the symptomatic testis compared with the asymptomatic testis is highly predictive of acute testicular torsion (Figures 1, 2). Perfusion of only the periphery of the testis at color Doppler is also abnormal and concerning for torsion (Figure 3). A study in which all patients with an acute scrotum were taken to surgery found these signs to have a sensitivity of 96.8% and specificity of 97.9%.6 Altered testicular Doppler flow indirectly indicates the presence of spermatic cord torsion. Note that in cases of incomplete torsion with preserved flow, color Doppler flow may be decreased, symmetrical or, rarely, even increased.7 For this reason, familiarity with additional signs of testicular torsion is helpful. Additionally, visualization of color Doppler flow has been a reported limitation in boys 2-4 years of age, particularly when the testis is in the inguinal canal.
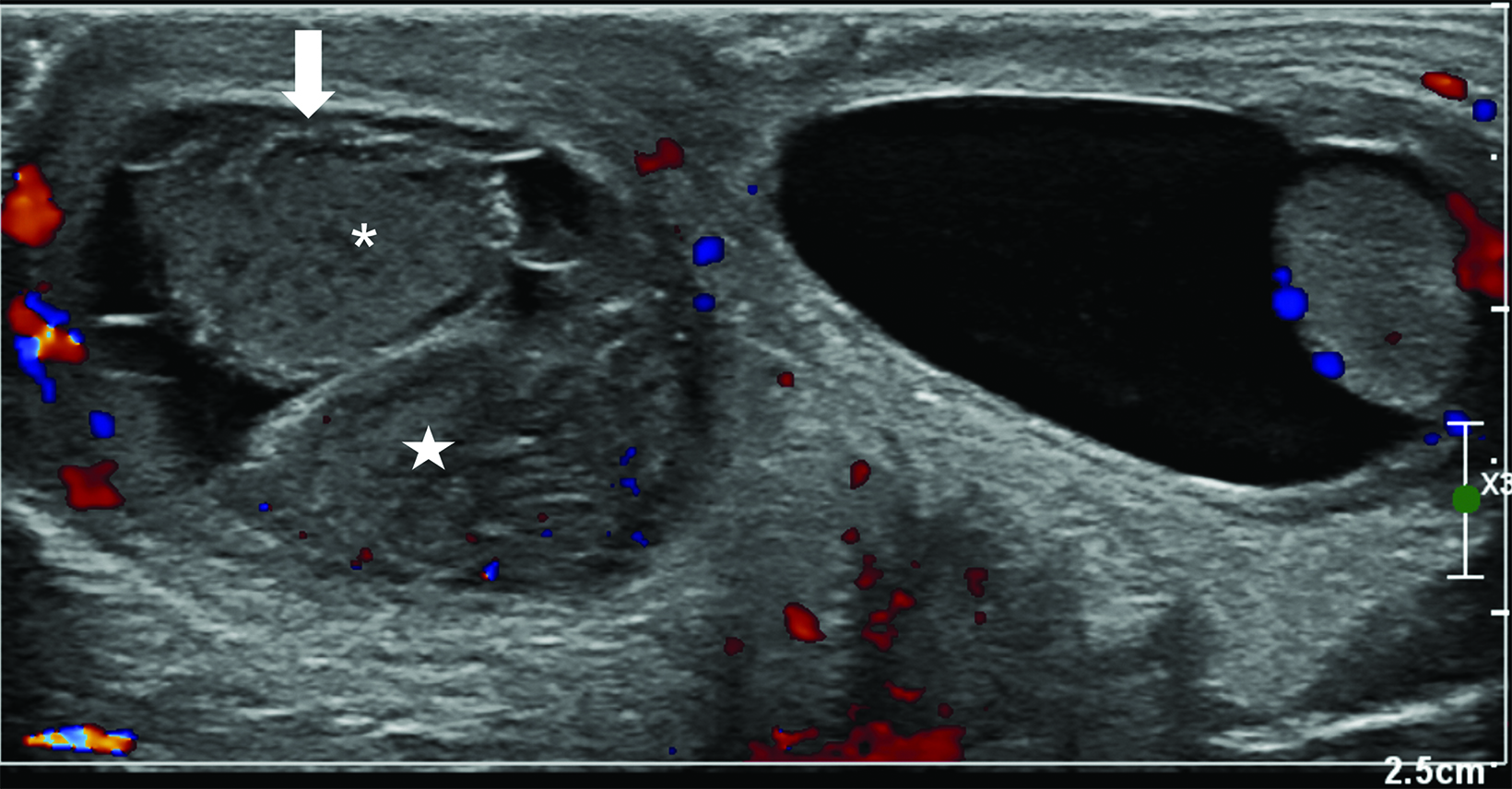
Whirlpool sign
The most reliable sign of testicular torsion is the spermatic cord whirlpool sign, a direct indication of torsion. The whirlpool sign appears as an abrupt, spiral-like change in the course of the spermatic cordon either grayscale or color Doppler US (Figure 1). Sensitivity of 92% and specificity of 99% have been reported In older children.8
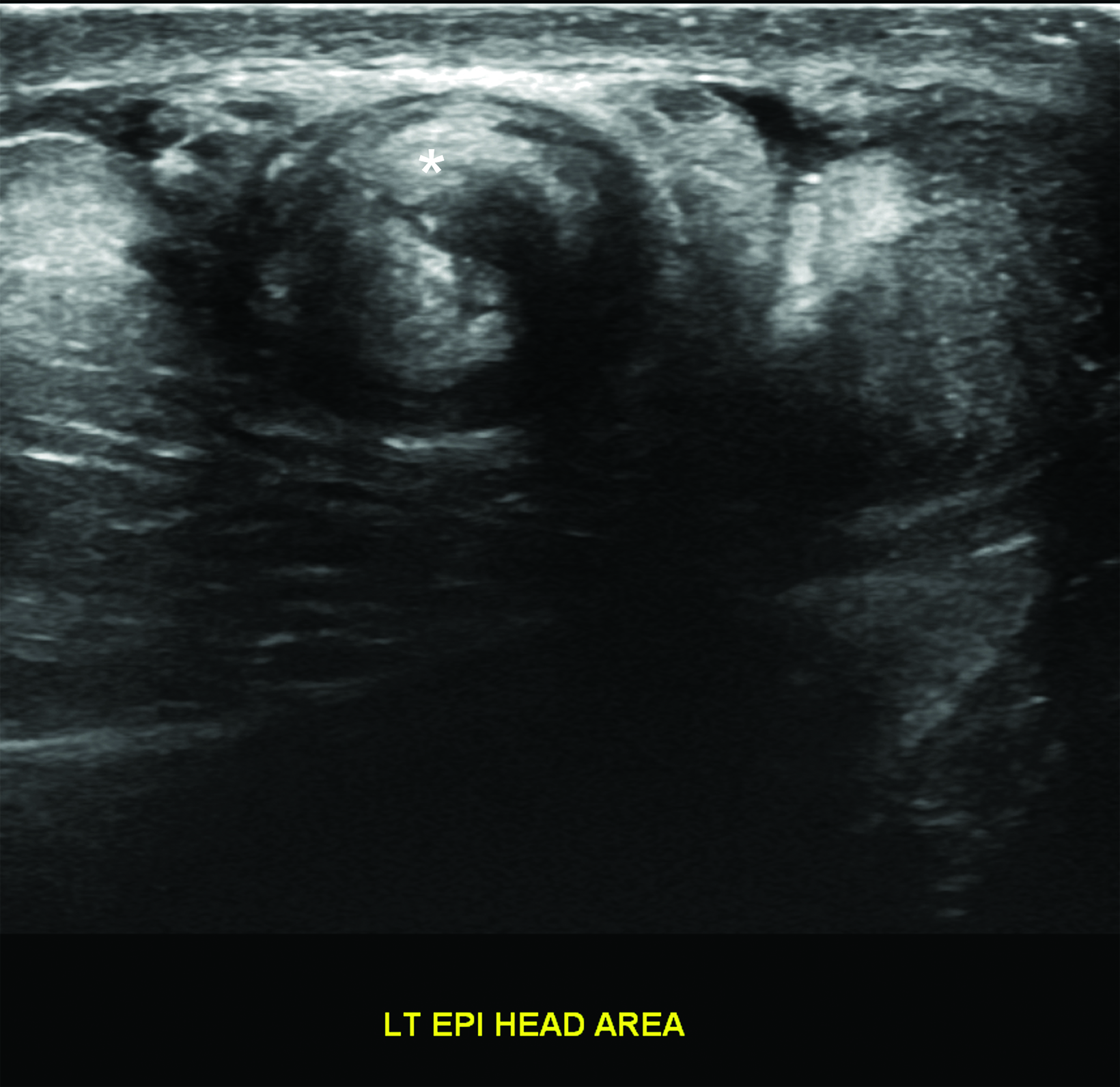
Redundant Spermatic Cord/Torsion Knot
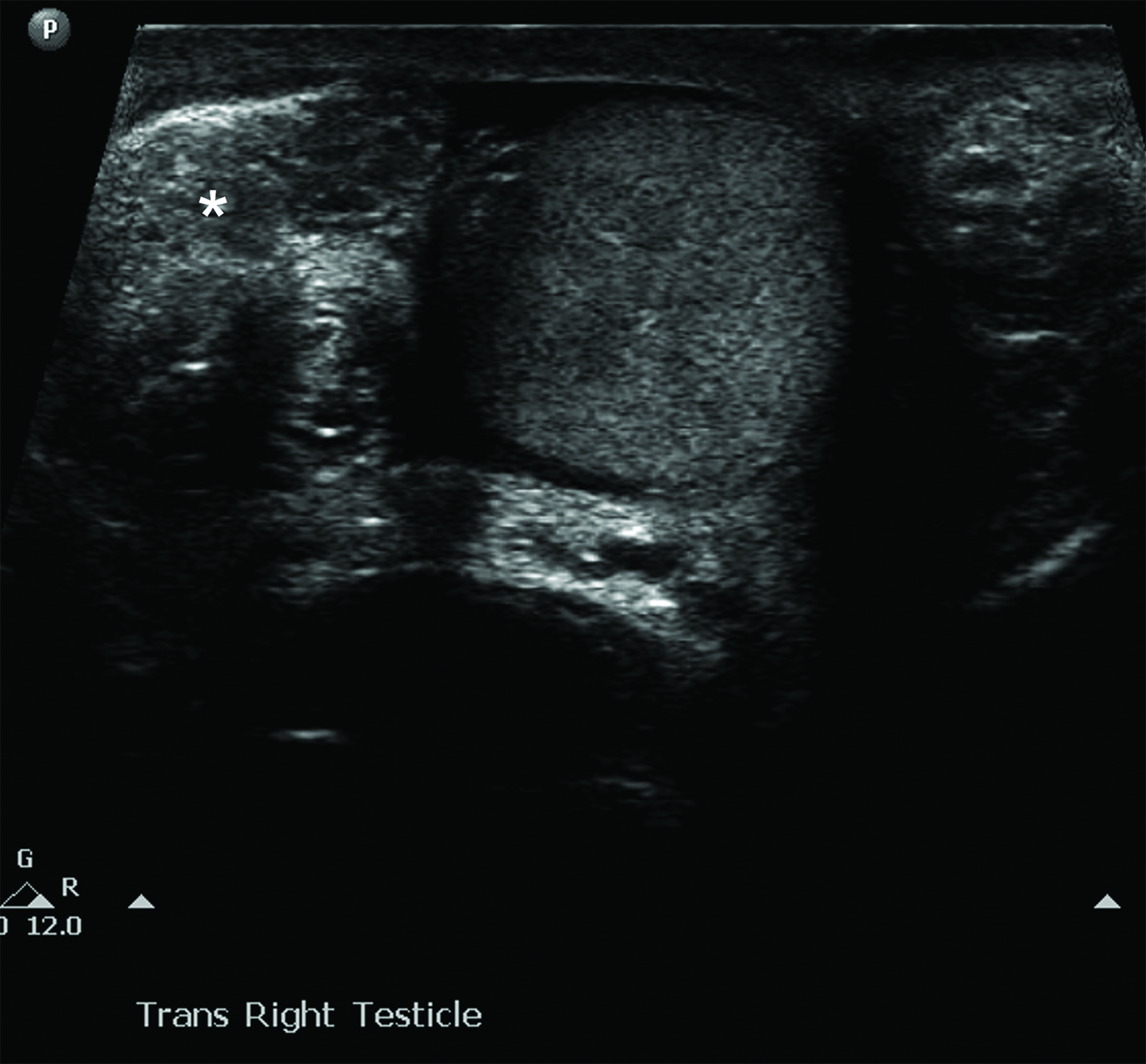
There should normally be no free piece of spermatic cord in the scrotum. The presence of a redundant, wavy piece of cord indicates an anomalous tunica vaginalis attachment (the bell clapper anomaly). In testicular torsion, the redundant, bunched-up cord may be seen lying freely in the superior scrotum. It often looks like an ovoid, extra-testicular, heterogeneous mass and is known as a “boggy pseudo-mass” or “torsion knot” (Figure 4).7 Flow may be present in some or all of the torsion knot, depending on the degree of torsion. The torsion knot is also a direct sign of testicular torsion.
Altered Lie
Normal testes are oriented vertically with the mediastinum testis located posterolaterally. An altered (horizontal or oblique) lie suggests anomalous tunica vaginalis attachment (the bell clapper anomaly) and also can be associated with intermittent testicular torsion (Figure 5).9
Concerning Nonspecific Findings
The following findings are abnormal but not specific to testicular torsion: globular testicular enlargement; heterogeneous echotexture; epididymal enlargement without hyperemia; and abnormal spectral Doppler flow (decreased or reversed diastolic flow). Hydroceles or hematoceles are common. Normal testicular echogenicity (with or without mild testicular enlargement) is a good sign of viability. Marked enlargement, heterogeneous echotexture, and scrotal wall hypervascularity are signs of testicular infarction and necrosis.10 Hemorrhagic infarction may occur with diffuse, focal, or multifocal testicular hyperechogenicity.10
Extravaginal Testicular Torsion Findings
The testis is usually necrotic at birth and the hemiscrotum is swollen and discolored. US findings vary, but complex hydrocele and calcification of the tunica albuginea are common (Figure 6).
Testicular Torsion Mimics
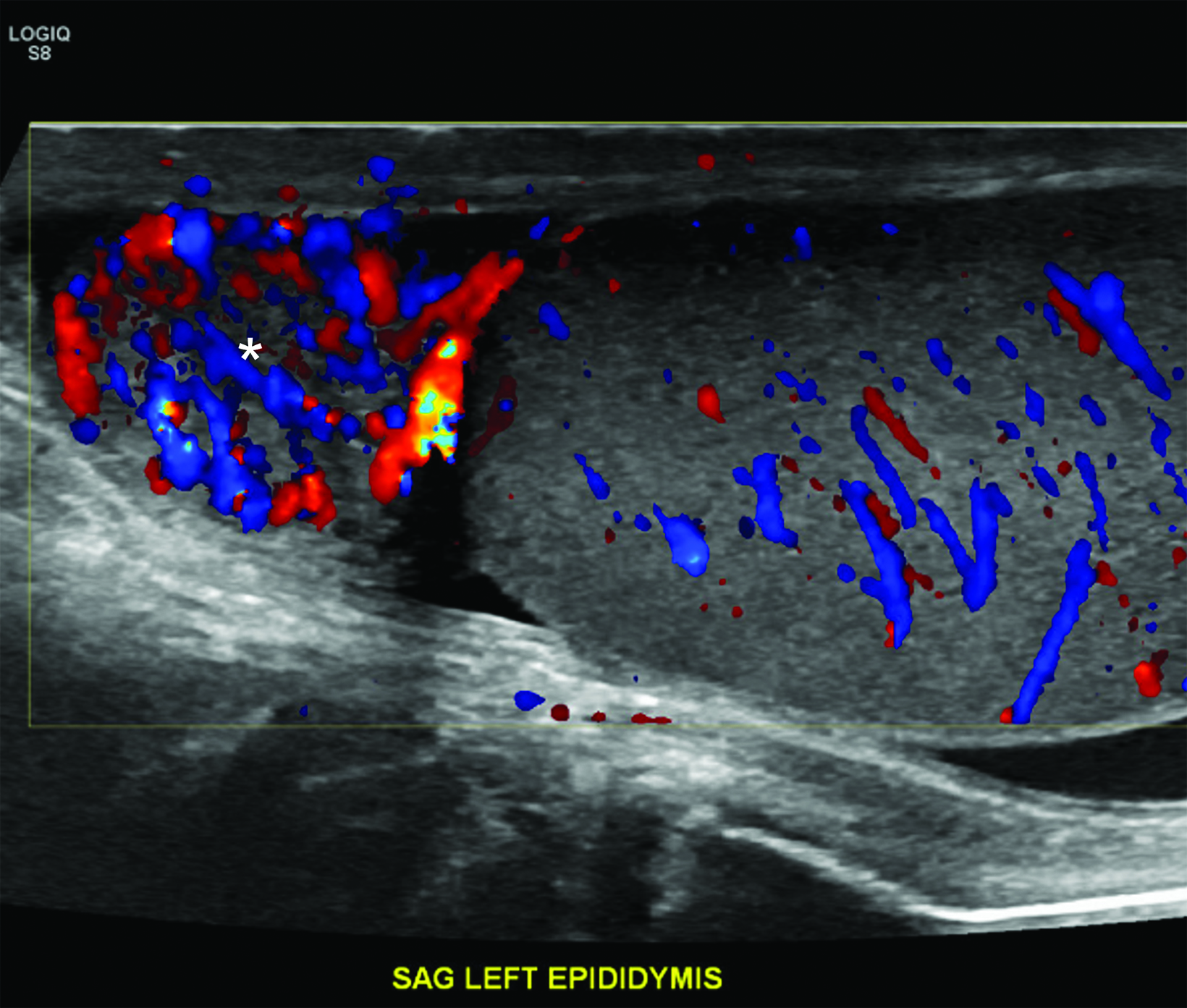
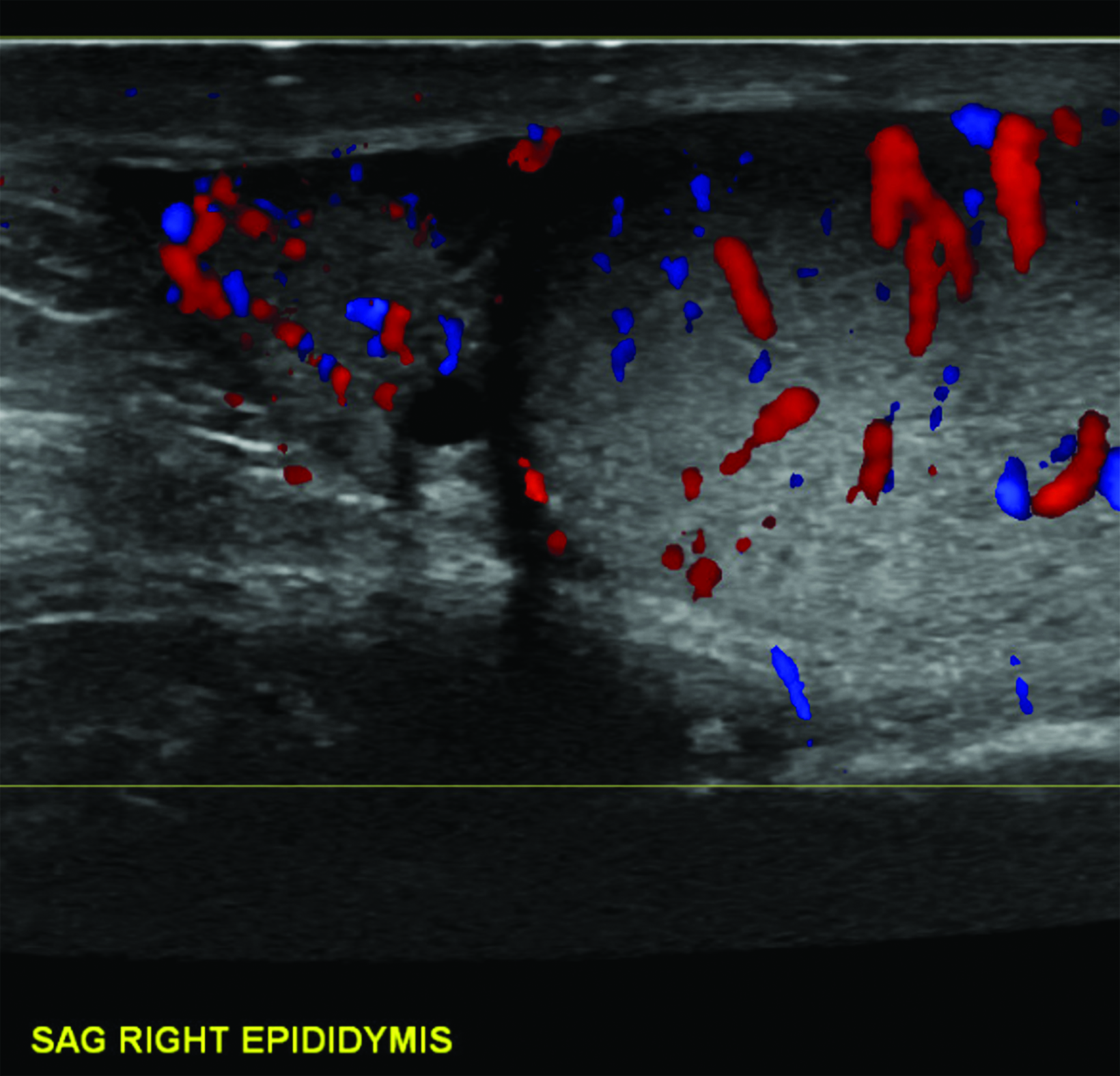
Epididymitis
Differentiating torsion from epididymitis, an infection of the epididymis and sometimes the testis, is important. In an analysis of malpractice claims related to testicular torsion, epididymitis was the most cited misdiagnosis (61%).11 At grayscale imaging, the epididymis is enlarged with variable or heterogeneous echogenicity. The epididymal head is most often affected. Color Doppler flow is increased within the epididymis, testis, or both (Figure 7). Analysis of the epididymal waveform may reveal a low-resistance pattern as compared with the normal pattern.
While absent epididymal vascularity most often results from complete torsion, flow may be maintained and the epididymis enlarged and heterogeneous in cases of incomplete torsion, potentially leading to misdiagnosis. It is critical to pay careful attention to testicular Doppler flow to detect subtle asymmetry, as well as to the spermatic cord to identify a whirlpool sign or a torsion knot. Spontaneous detorsion can manifest as hyperemia of the epididymis and testis. Importantly, detorsion will result in resolution of symptoms.
Appendage Torsion
Torsion of one of the appendages about the testis is a common cause of pediatric acute scrotum.5 The appendages of the testis and epididymis are remnants of the mesonephric and paramesonephric ducts and, as sessile structures, are predisposed to torsion. The torsed appendage appears as a round, avascular extra-testicular structure with variable echogenicity. The epididymis and scrotum may be hypervascular and swollen. Unlike cases of testicular torsion, testicular vascularity is not decreased.
Correlation with the patient’s symptoms is essential to correct diagnosis. Sudden onset of pain and severe nausea and vomiting both suggest testicular torsion. Swelling of the scrotal soft tissues, a finding that occurs only late in torsion, is more common in inflammatory conditions such as epididymitis and appendage torsion.
Conclusion
Radiologists play a critical role in the evaluation of the acute scrotum and must be able to recognize complete and incomplete testicular torsion. Ultrasound is the imaging modality of choice. Incomplete torsion can be difficult to recognize. Careful attention to grayscale spermatic cord findings and color Doppler testicular flow symmetry are keys to the diagnosis. Scrotal exploration should be considered in the presence of high clinical suspicion for testicular torsion, even if the ultrasound findings are nonspecific.
References
Citation
ML F.Imaging Testicular Torsion. Appl Radiol. (6):18-23.
November 3, 2023