Imaging of esophageal emergencies
Images










Esophageal conditions such as obstruction, perforation, inflammation and infection are common and may cause patients to present to the emergency room. The esophagus has traditionally been examined in great detail by contrast fluoroscopy or endoscopy, and subtle pathology may potentially be missed when depending on CT for screening evaluation without the mucosal detail provided by contrast esophagography. The presentation of chest pain without direct trauma should always include esophageal disease as a differential diagnosis. Given the increased use of CT in the emergency room, recognition of the appearance of various esophageal pathologies, with the potential to lead to emergent presentation, is required. Toward this end, this paper will discuss inflammation, infection, obstruction, perforation, trauma, ischemia, and hemorrhage of the esophagus.
Normal esophageal anatomy
The esophagus spans approximately 25-30 cm from the lower border of the cricoid cartilage to the gastroesophageal junction. Usually, it descends along the left of midline in the neck then deviates to the right throughout most of its thoracic course. It returns to the left before entering the diaphragmatic hiatus at T10. Normal esophageal wall thickness is considered less than or equal to 5 mm on CT.1 The esophagus is surrounded by adventitia without a serosa. This lack of serosa permits esophageal pathology to spread more easily superiorly into the neck, laterally into the mediastinum or inferiorly into the upper abdomen.
Esophageal inflammation/infection
Esophagitis
Infection, radiation, gastroesophageal reflux and medications can all cause esophagitis. Esophagitis is inflammation of the mucosa with variable involvement of the deeper layers. The CT findings of infectious esophagitis are nonspecific and insensitive compared to fluoroscopy and endoscopy, which are both considered superior for detailed assessment of the mucosa.1 During fluoroscopy, barium becomes trapped between raised mucosal plaques of candida esophagitis. Herpes esophagitis is visualized when barium pools in multiple small ulcers. Cytomegalovirus and HIV esophagitis present with larger ulcers. Reticular appearing mucosa in the distal esophagus may be seen with reflux esophagitis and Barrett’s esophagus. Long segment mid esophageal esophagitis may be seen in patients with recent mediastinal radiation. In contrast, CT findings of esophagitis – regardless of the underlying cause---include a long segment of circumferential esophageal wall thickening with or without a “target sign.” A target sign is caused by mucosal hyperemia and submucosal edema. However, wall thickening and the target sign were seen in only 55% and 17% of patients with esophagitis, respectively, in one study.1 Because of these nonspecific findings, CT distinction between infectious and noninfectious causes of esophagitis is often difficult.1 Details of clinical history or additional clues such as a radiation port for thoracic malignancy may be helpful (Figure 1). While it lacks the mucosal detail that fluoroscopy provides, CT does offer the advantage of better delineating complications of esophagitis including perforation, functional obstruction or aspiration.
Esophageal ischemia
Esophageal ischemia is rare secondary to a redundant overlapping blood supply. The cervical esophagus is supplied by the thyroidal arteries, the thoracic esophagus is supplied by the aorta as well as the intercostal, tracheal and bronchial arteries, and the abdominal esophagus is supplied by the left gastric artery. Esophageal ischemia is often idiopathic but secondary causes include acute traumatic aortic injury, nasogastric tube trauma, severe esophagitis and gastric volvulus (Figure 2). CT findings of ischemic esophagitis overlap considerably with those of infectious or inflammatory esophagitis, although the presence of pneumatosis favors ischemia.
Esophageal obstruction
Foreign bodies
Most ingested objects pass spontaneously through the esophagus without intervention. While foreign body ingestion occurs across all age groups, esophageal foreign bodies are most often ingested by children and adult patients with cognitive defects. Commonly seen foreign bodies include food boluses, fish or chicken bones, and coins.2 The majority of ingested foreign bodies pass spontaneously, but 10-20% of these require endoscopic removal. Ingested foreign bodies that would prompt endoscopic removal include sharp objects, button batteries, or objects causing obstruction.3 Up to one-third of adult patients will have an underlying esophageal stricture contributing to impaction and approximately 1% of all patients require surgery for removal.4,5 When an appropriate history is obtained, the diagnostic workup usually starts with conventional radiographs, particularly if the object is radiodense or suspected to be in the hypopharynx. Fish bones may become lodged in the hypopharynx, are difficult to visualize with endoscopy, but are well evaluated with CT. The appearance of esophageal obstruction due to foreign bodies on CT is variable given the variety of objects that can be ingested (Figures 3-5). In addition to localization, CT also provides the added benefit of identifying complications.
Esophageal strictures
As discussed above, strictures of the esophagus can cause obstruction which can lead to presentation to the emergency room. Strictures can be benign or malignant in etiology. Longstanding gastroesophageal reflux, radiation, chronic medication-induced esophagitis, nasogastric intubation, epidermolysis bullosa and eosinophilic esophagitis are all possible causes for benign strictures. Benign strictures usually have smooth borders and involve a longer segment of the esophagus. In contrast, malignant strictures typically involve a shorter segment of the esophagus with nodular mucosal-shouldering barium studies can often differentiate benign from malignant strictures, but strictures with indeterminate or malignant features require further evaluation with endoscopy.6 On CT, submucosal soft tissue attenuation thickening can be a clue to underlying malignancy. Advanced stage esophageal tumors with invasion of adjacent structures and lymphadenopathy are well evaluated with CT.7
Esophageal trauma
The esophagus can be injured from intraluminal and extraluminal causes. Blunt and penetrating traumatic injuries to the esophagus are not commonly seen, possibly secondary to its relative flexibility and protected anatomic location for most of its course. Traumatic injuries to the esophagus are associated with serious injuries to the airway, spine and aorta.2 Clinical symptoms that raise the suspicion of esophageal injury include chest pain, especially dysphagia, pneumomediastinum and usually right pleural effusion. The study of choice to detect an esophageal injury is traditionally esophagography with water-soluble contrast followed by barium. The latter is due to its generally accepted increased sensitivity for detecting leaks. However, for patients with blunt or penetrating trauma, CT is the first-line modality as it can simultaneously evaluate all internal organs rather than just the esophagus. In these cases, esophageal wall thickening, mediastinal gas and fluid collections, focal esophageal defects, pleural effusions, and aspiration are signs of an esophageal injury (Figure 6).8 The more specific subtypes of esophageal injury after trauma, ranging from the superficial mucosal tears to more serious transmural perforations, are detailed below.
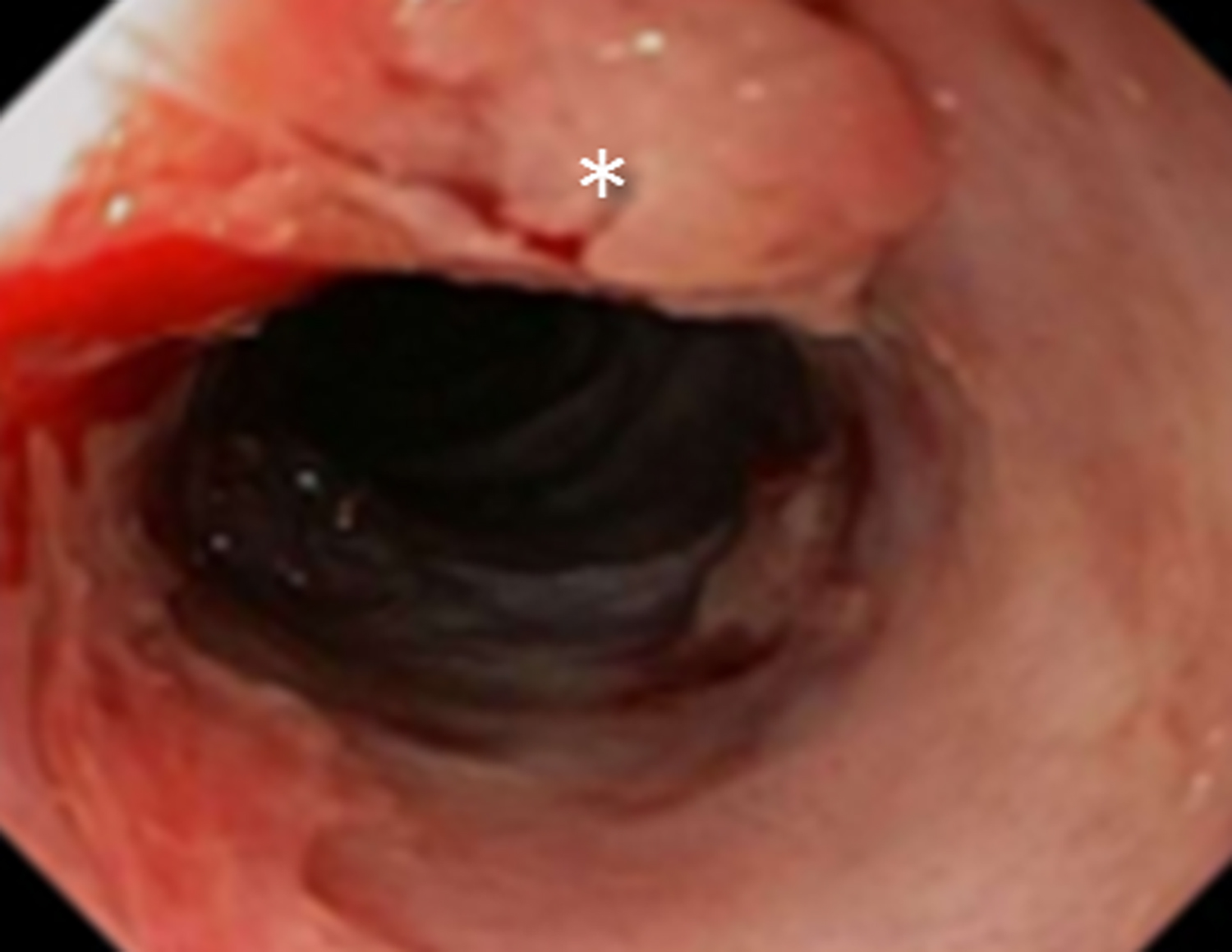
Esophageal perforation
A Mallory-Weiss tear is a superficial mucosal laceration extending longitudinally, often in the distal esophagus. Similar to Boerhaave syndrome, it typically results from increased intraluminal pressure in the setting of emesis. Superficial tears can also occur after stricture dilation or other endoscopic procedures (Figure 7). Hematemesis or “coffee ground” emesis following forceful vomiting is the typical clinical presentation of Mallory-Weiss tears. On barium studies, contrast will form linear collections in any lacerations. (Figure 8).9 Although there are no sensitive CT findings, occasionally small foci of gas or punctate hemorrhage may be present in the distal esophagus to suggest a tear.2
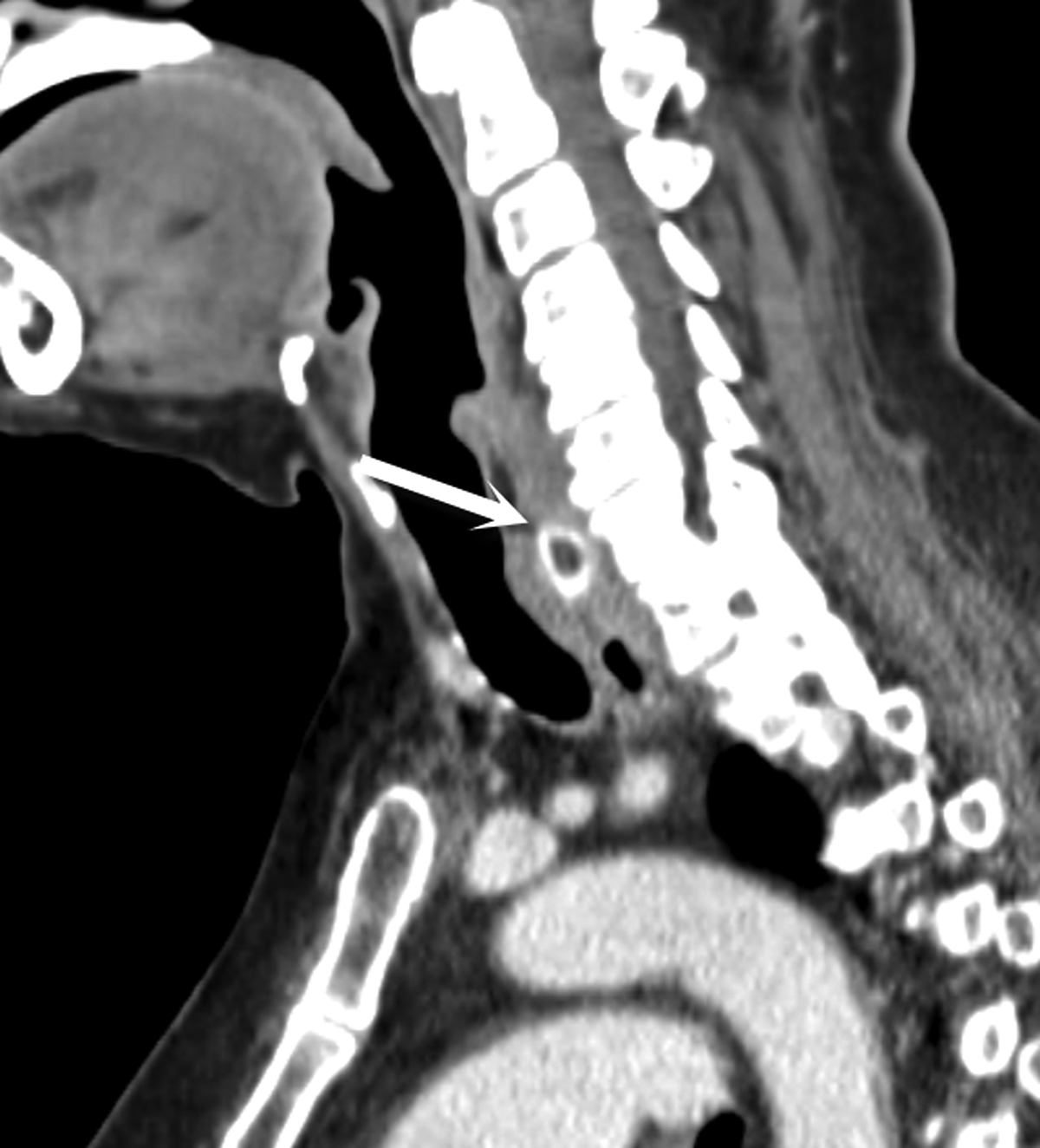
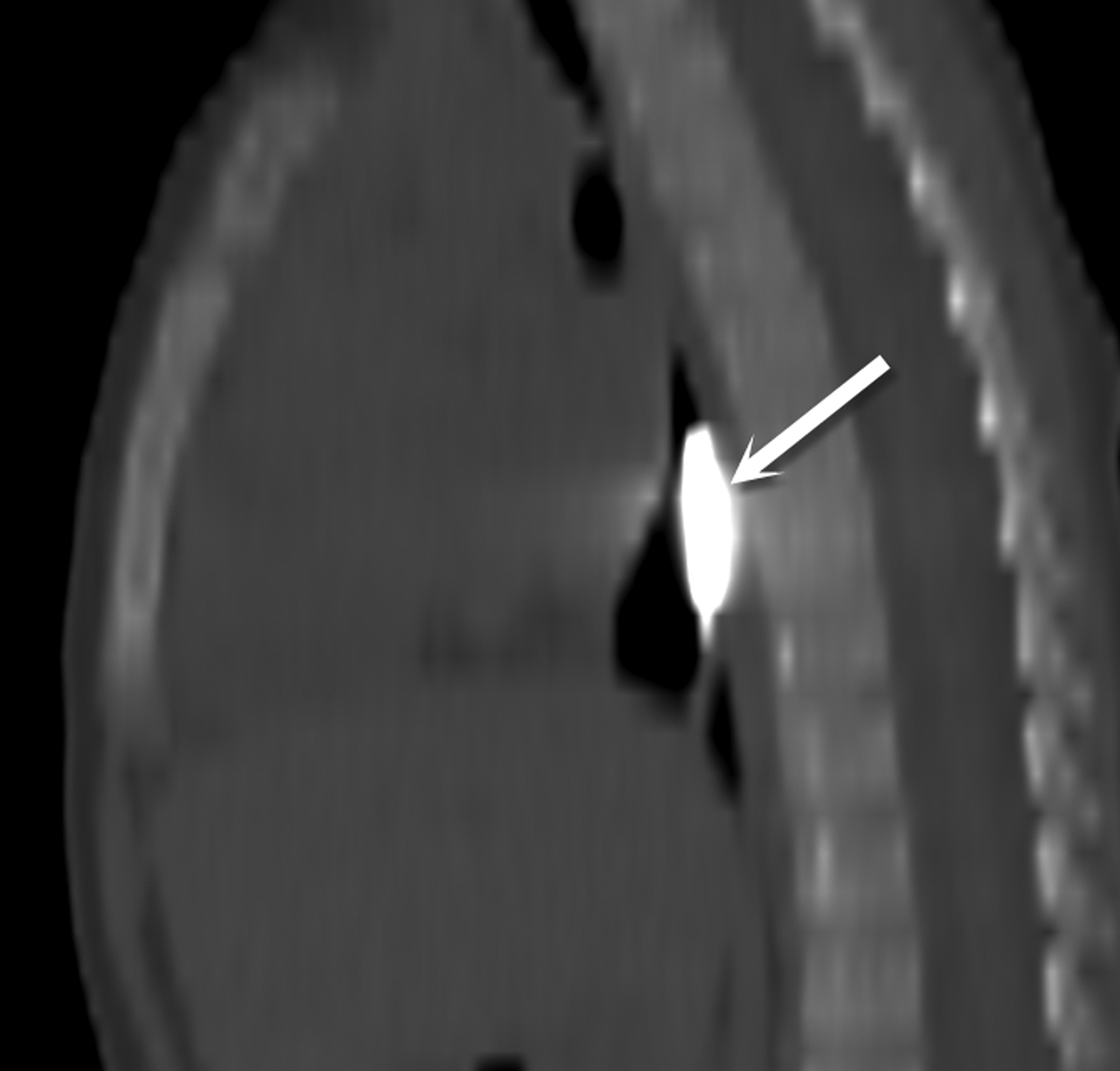
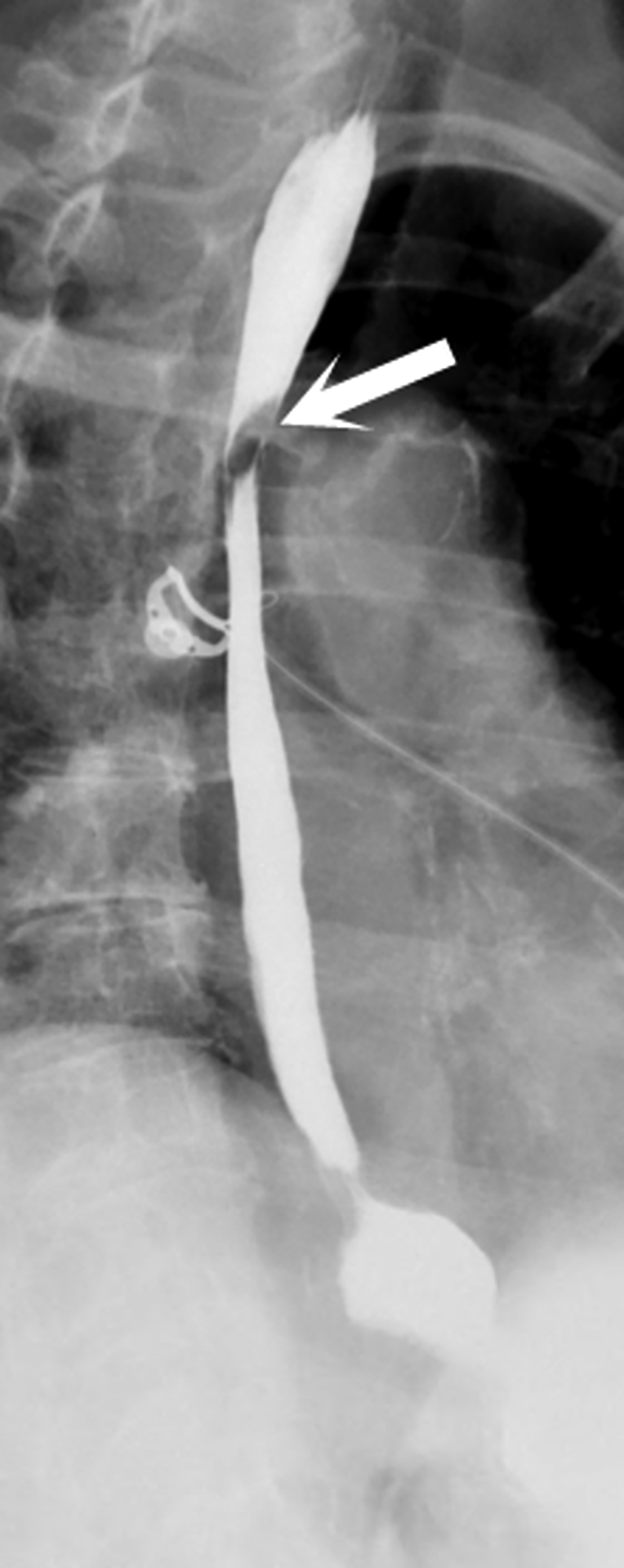
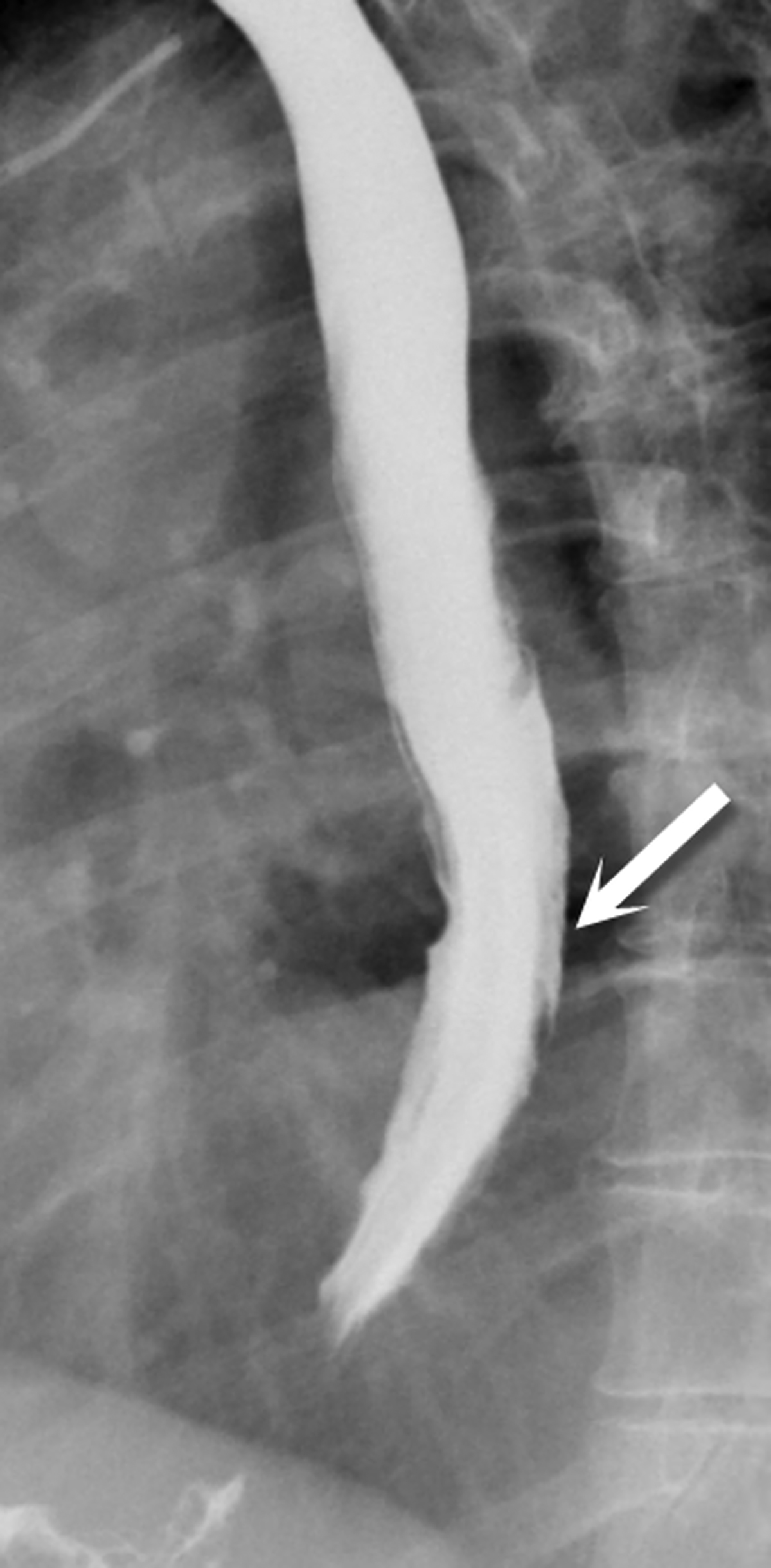
Esophageal dissection
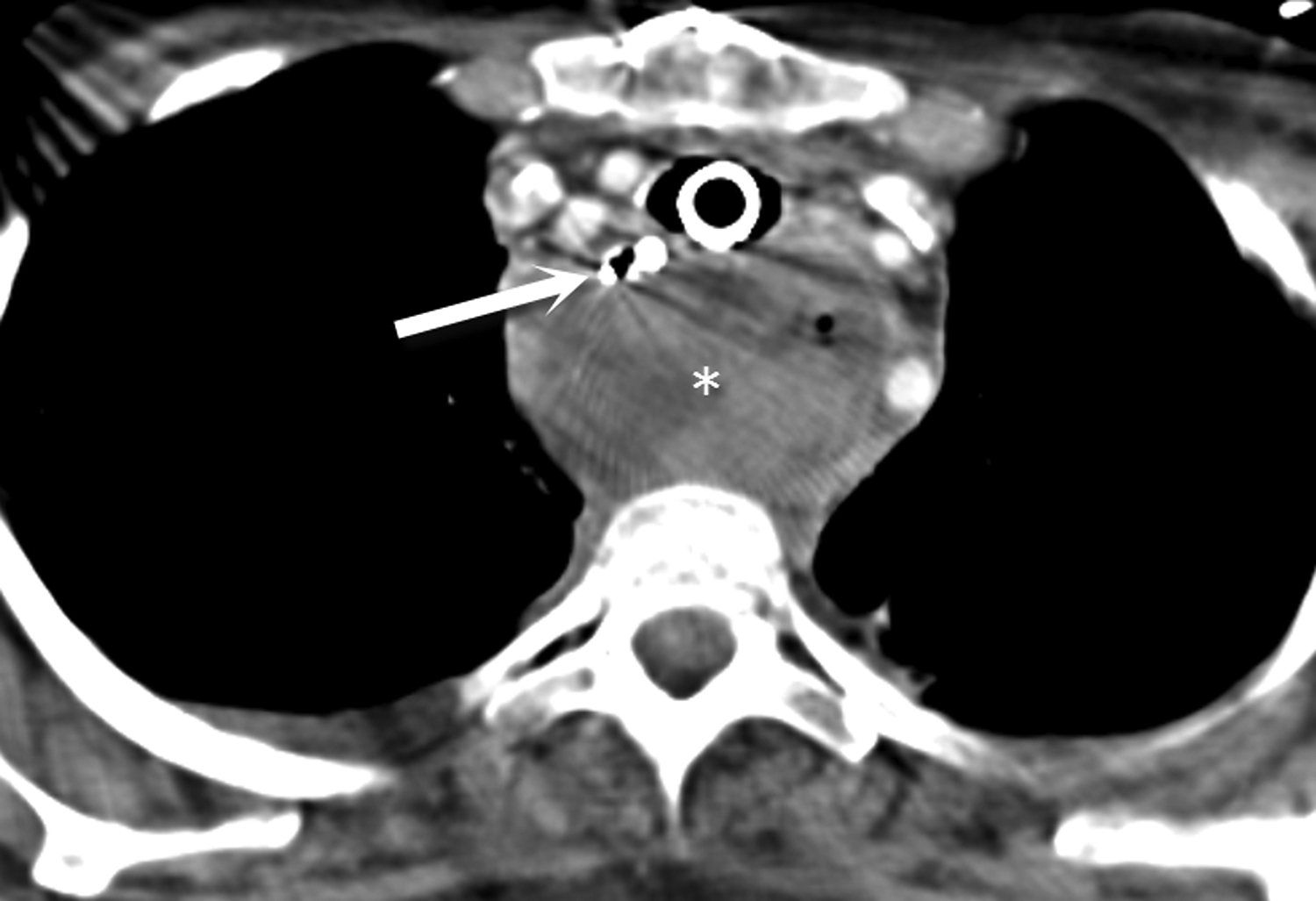
Intramural dissection and/or hemotoma can be considered an intermediate form of injury between a Mallory-Weiss tear and transmural perforation. They are rare forms of esophageal injury, but clinically present similarly to full thickness tears with symptoms including abrupt onset of chest pain, dysphagia or hematemesis. Although there is sparse data on this entity in the literature, the most common cause is recent instrumentation such as endoscopy or stricture dilatation (Figure 9). Imaging features on both esophagraphy and CT may show a submucosal dissection flap or hematoma. The appearance of a dissection flap has been referred to as a “double barrel esophagus” caused by contrast flowing into a true and false lumen. Contrast can accentuate a linear mucosal flap separating the two lumens, which has also been called the “mucosal stripe sign.”2,10 There is a similar appearance on CT. (Figure 10). The false lumen tends to be posterior and often better appreciated on sagittal or coronal reformatted images. Esophageal dissection can be distinguished from intramural hematoma by visualization of contrast in the false lumen, but there is considerable overlap between the two subtypes of intramural perforation (Figure 11).
Transmural perforation
Full thickness tears of the esophagus are the most severe form of perforation. Similar to esophageal dissection, surgery, stricture dilatation, stenting, or thermal ablation procedures may result in transmural perforation. Boerhaave syndrome refers to esophageal rupture that occurs with vomiting secondary to incomplete cricopharyngeal muscle relaxation and increased intraluminal pressure. In addition, primary or metastatic esophageal tumor may perforate, especially after treatment with palliative dilation and stenting. Regardless of the cause, complications are more serious than Mallory-Weiss tears or esophageal dissection and include mediastinitis, pneumonia, empyema and abscess formation. CT findings include pneumomediastinum, mediastinal fluid, pleural effusions and pulmonary findings of aspiration. If oral contrast is used, extraluminal contrast may leak into the mediastinum or peritoneum from the esophagus (Figure 12). In the setting of trauma if pneumomediastinum is seen in isolation, it is unlikely that esophageal injury is the etiology given its rarity in blunt force injury.2,8,11
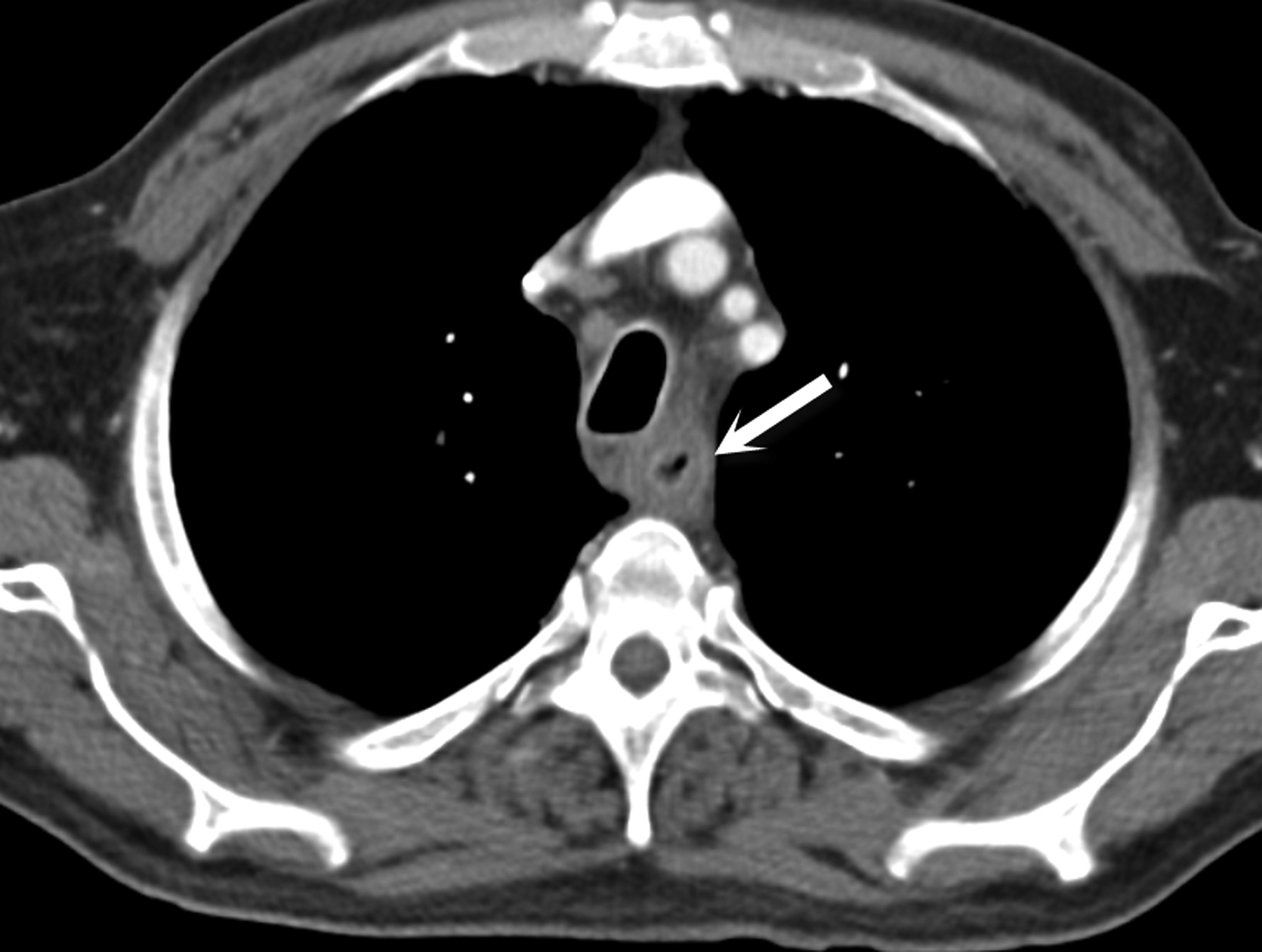
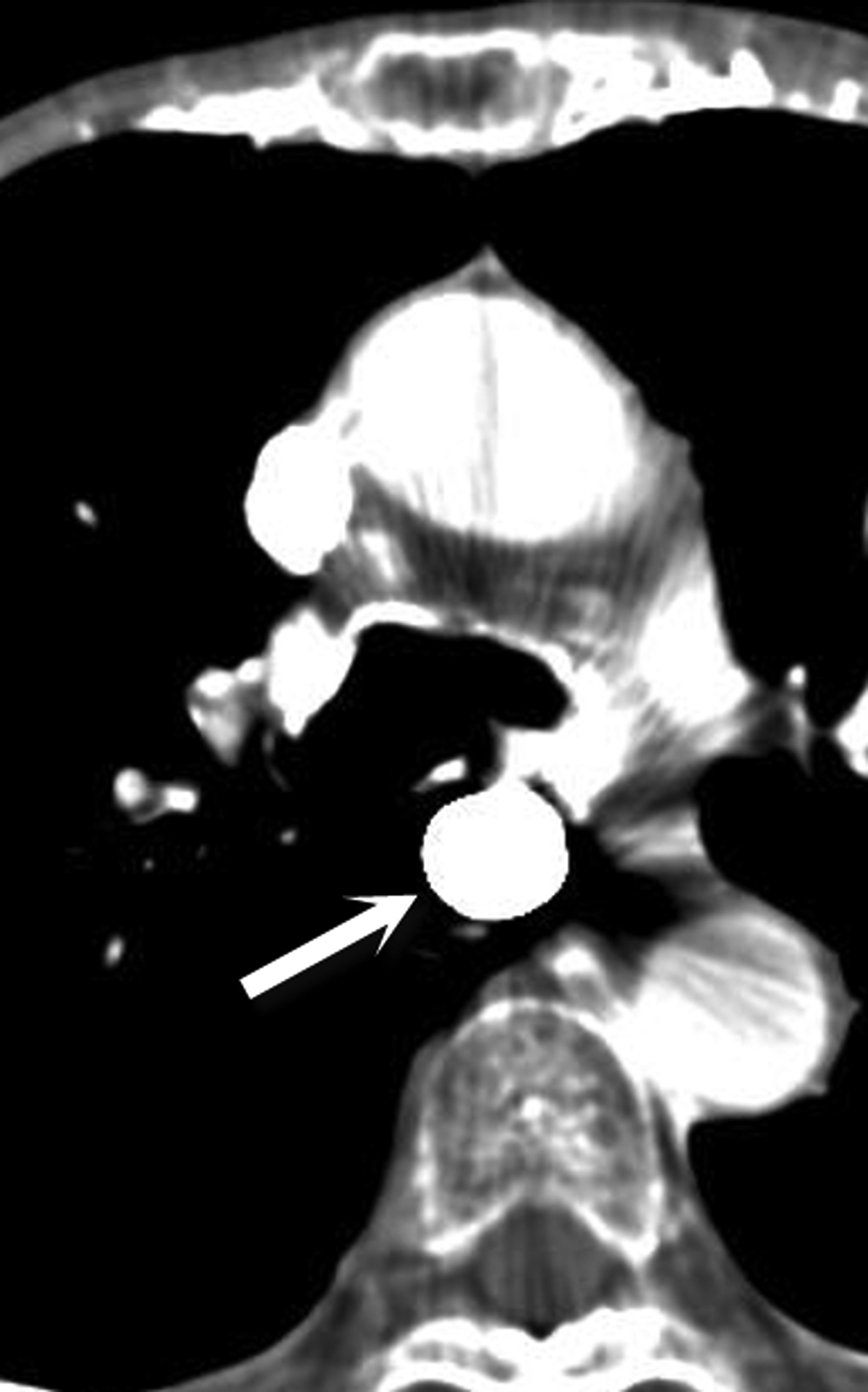
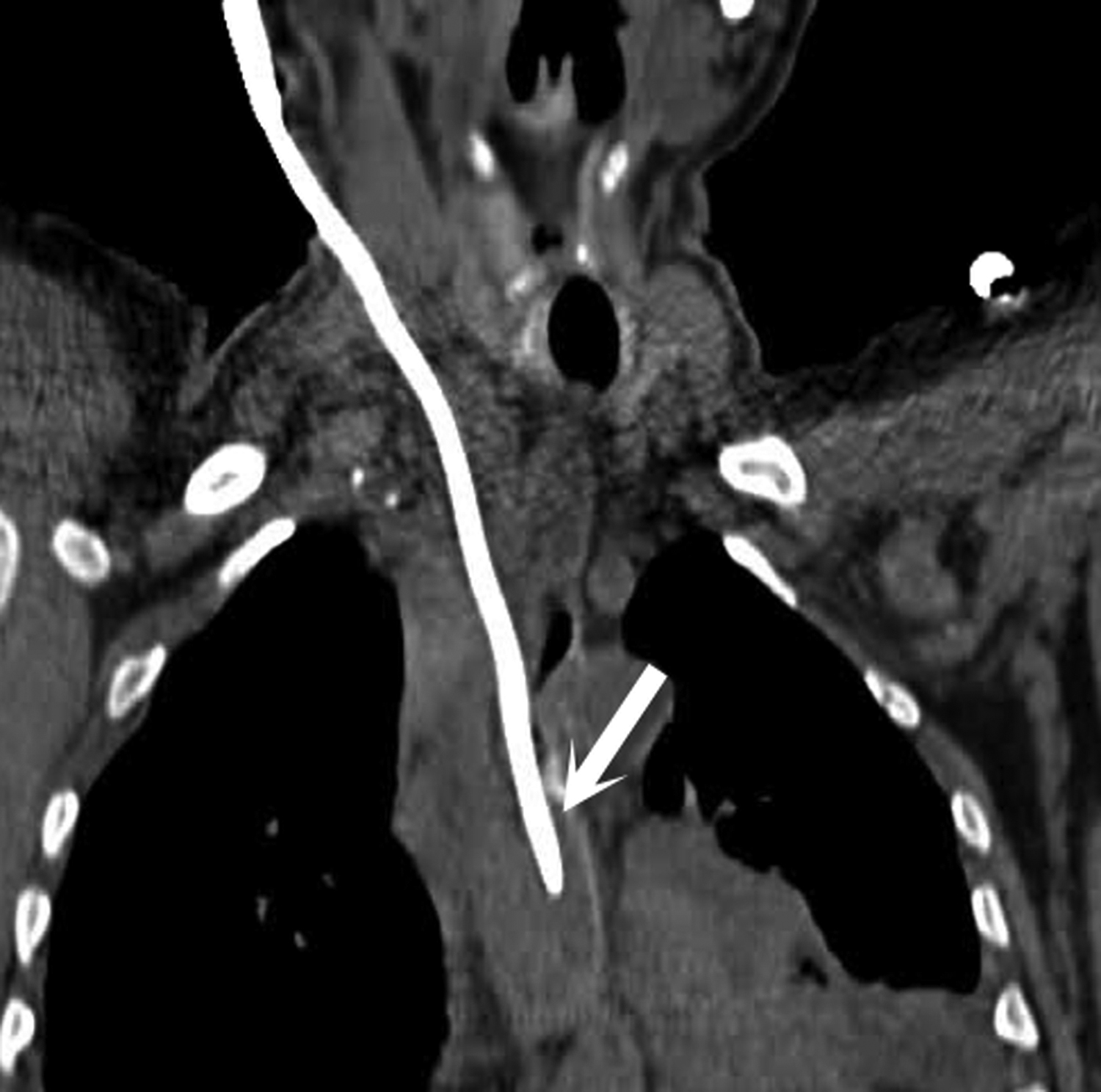
Aortoesophageal fistulas
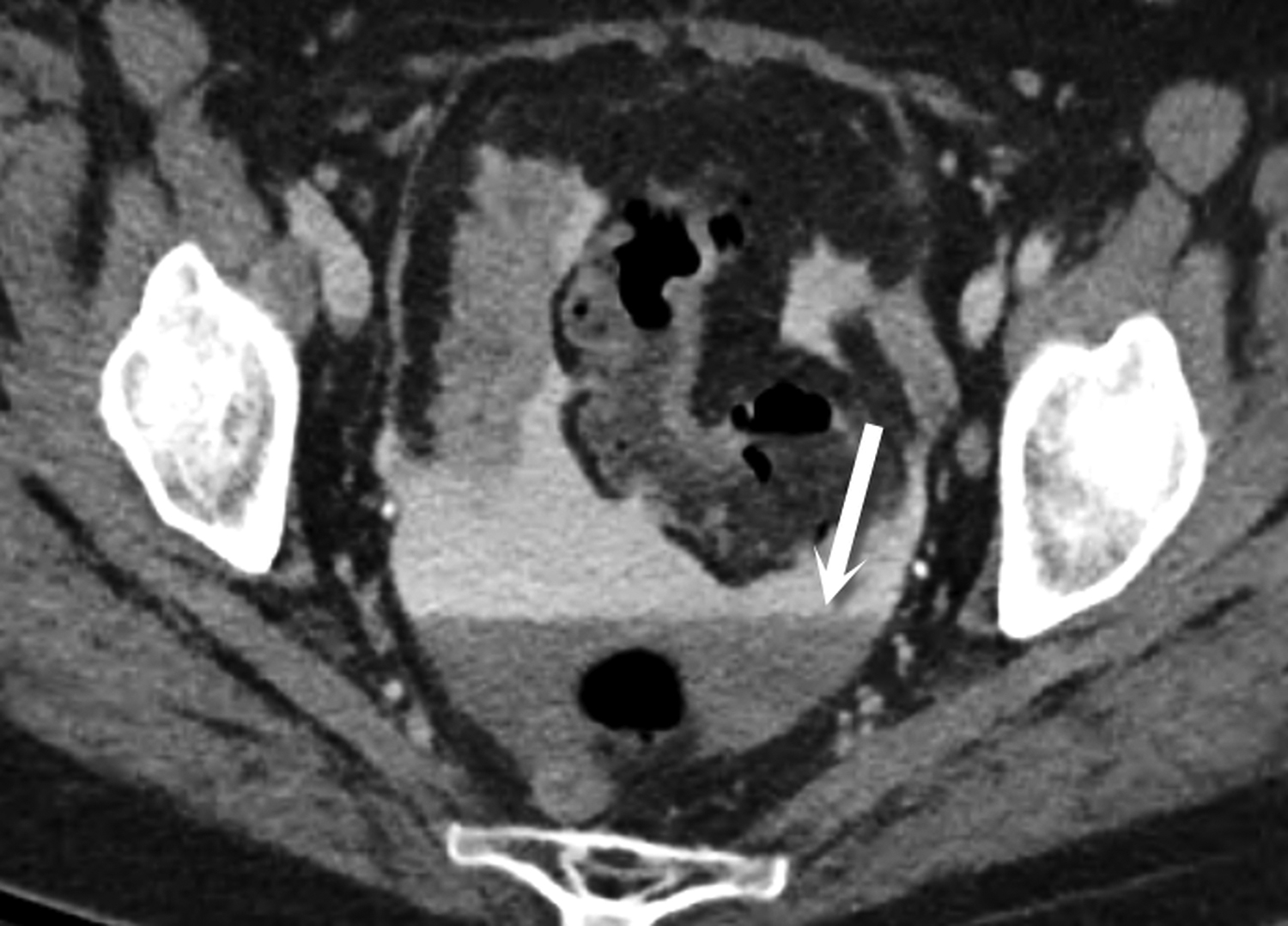
Aortoesophageal fistulas are rare, but may arise from esophageal perforations. Over time, the perforation can result in fistula formation to the aorta, trachea or pleura. Other primary esophageal disorders such as esophagitis, foreign body perforations and advanced esophageal cancer have all been described as underlying causes.12,13,14 More commonly, aortoesophageal fistulas arise from underlying thoracic aortic disease. Ruptured thoracic aortic aneurysms or infected aortic stents can fistulize to the esophagus. Clinically, patients may present with mid-thoracic pain and an episode of hematemesis which is followed by a symptom free interval that leads to massive upper gastrointestinal bleeding. This presentation is known as the Chiari triad.12,13,14 On CT, intravenous contrast does not need to be seen within the esophagus: Active bleeding through a fistula is acutely life-threatening as the patient can quickly exsanguinate. A more common CT appearance includes a focal outpouching of the aorta towards an area of esophageal wall thickening with extraluminal gas abutting the aortic wall (Figures 13 and 14).15
Esophageal hemorrhage
A variety of insults can lead to esophageal hemorrhage including esophagitis with ulceration, esophageal varices, tumor and Mallory-Weiss tears. Esophageal varices and Mallory-Weiss tears are the two most common disorders leading to bleeding of esophageal origin. Endoscopic and pharmacologic treatments have substantially decreased mortality from esophageal bleeding.16 On CT, findings are similar to small bowel hemorrhage: High attenuation blood in the lumen and extravasation of intravenous contrast are the principal signs of active bleeding. (Figure 15).
Conclusion
Although the esophagus traditionally has been evaluated with contrast fluoroscopy, the use of CT in patients presenting to the emergency room with symptoms that suggest esophageal pathology is rapidly increasing. Although some disorders, such as esophagitis, have a nonspecific appearance relative to the underlying cause, other conditions such as esophageal perforation and hemorrhage can and should be readily diagnosed to guide emergent treatment. It is therefore incumbent upon the radiologist in the emergency department to have familiarity with these conditions to provide a timely, accurate diagnosis.
References
- Berkovich GY, Levine MS, Miller WT. CT findings in patients with esophagitis. AJR Am J Roentgenol. 2000; 175(5):1431-1424.
- Young CA, Menias CO, Bhalla S, et al. CT features of esophageal emergencies. Radiographics. 2008; 28(6):1541-1553.
- Eisen GM, Baron TH, Dominitz JA, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002; 55(7):802-806.
- Mosca S, Manes G, Martino R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy. 2001; 33(8):692-896.
- Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995; 41(1):39-51.
- Gupta S, Levine MS, Rubesin SE, et al. Usefulness of barium studies for differentiating benign and malignant strictures of the esophagus. AJR Am J Roentgenol. 2003; 180(3):737-744.
- Ba-Ssalamah A, Zacherl J, Noebauer-Huhmann IM, et al. Dedicated multi-detector CT of the esophagus: spectrum of diseases. Abdom Imaging. 2009;34(1):3-18.
- Ho AS, Ahmed A, Huang JS, et al. Multidetector computed tomography of spontaneous versus secondary pneumomediastinum in 89 patients: can multidetector computed tomography be used to reliably distinguish between the 2 entities? J Thorac Imaging. 2012; 27(2):85-92.
- Sparberg, M. Roentgenographic documentation of the Mallory-Weiss syndrome. JAMA. 1968; 203(2):151-152.
- Eisenberg RL. Gastrointestinal Radiology : a Pattern Approach. 2nd ed. Philadelphia: Lippincott; 1990;1053
- Ghanem N, Altehoefer C, Springer O, et al. Radiological findings in Boerhaave’s syndrome. Emerg Radiol. 2003; 10(1):8-13.
- Baron RL, Koehler RE, Gutierrez FR, et al. Clinical and radiographic manifestations of aortoesophageal fistulas. Radiology. 1981; 141(3):599-605.
- Carter R, Mulder GA, Snyder EN, et al. Aortaesophageal fistula. Am J Surg. 1978; 136(1):26-30.
- Hollander JE, Quick G. Aortoesophageal fistula: A comprehensive review of the literature. Am J Med. 1991; 91(3):279-287.
- Longo JM, Lopez-Rasines G, Ortega E, et al. CT demonstration of an aortoesophageal fistula. Cardiovasc Intervent Radiol. 1987; 10(2):84-85.
- Wu JC, Chan FK. Esophageal bleeding disorders. Curr Opin Gastroenterol. 2005; 21(4):485-489.
Citation
S C, CO M, V M,. Imaging of esophageal emergencies. Appl Radiol. 2016;(10):16-22.
October 15, 2016