Imaging Acute Stroke in the Emergency Room Environment
Images
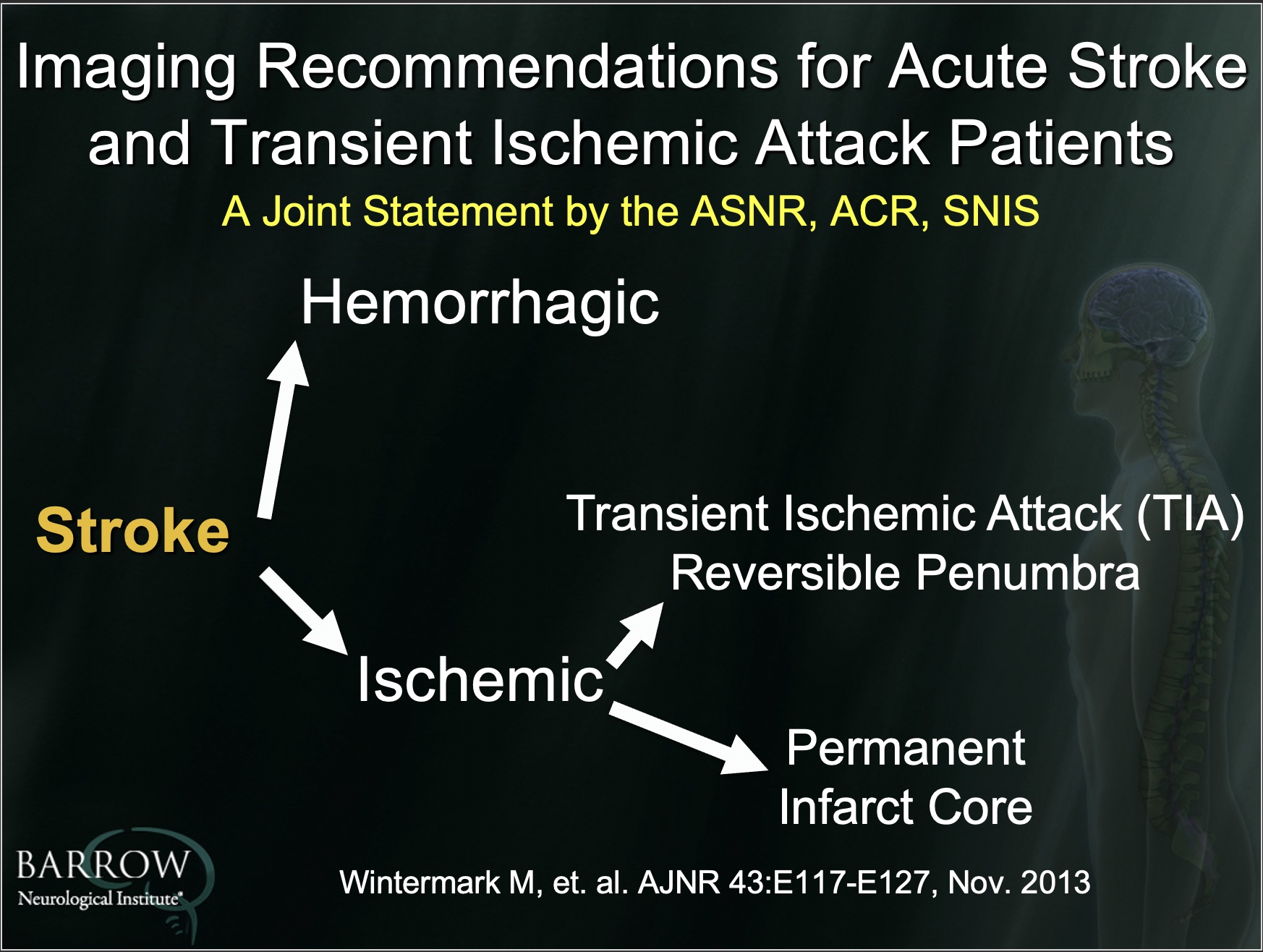
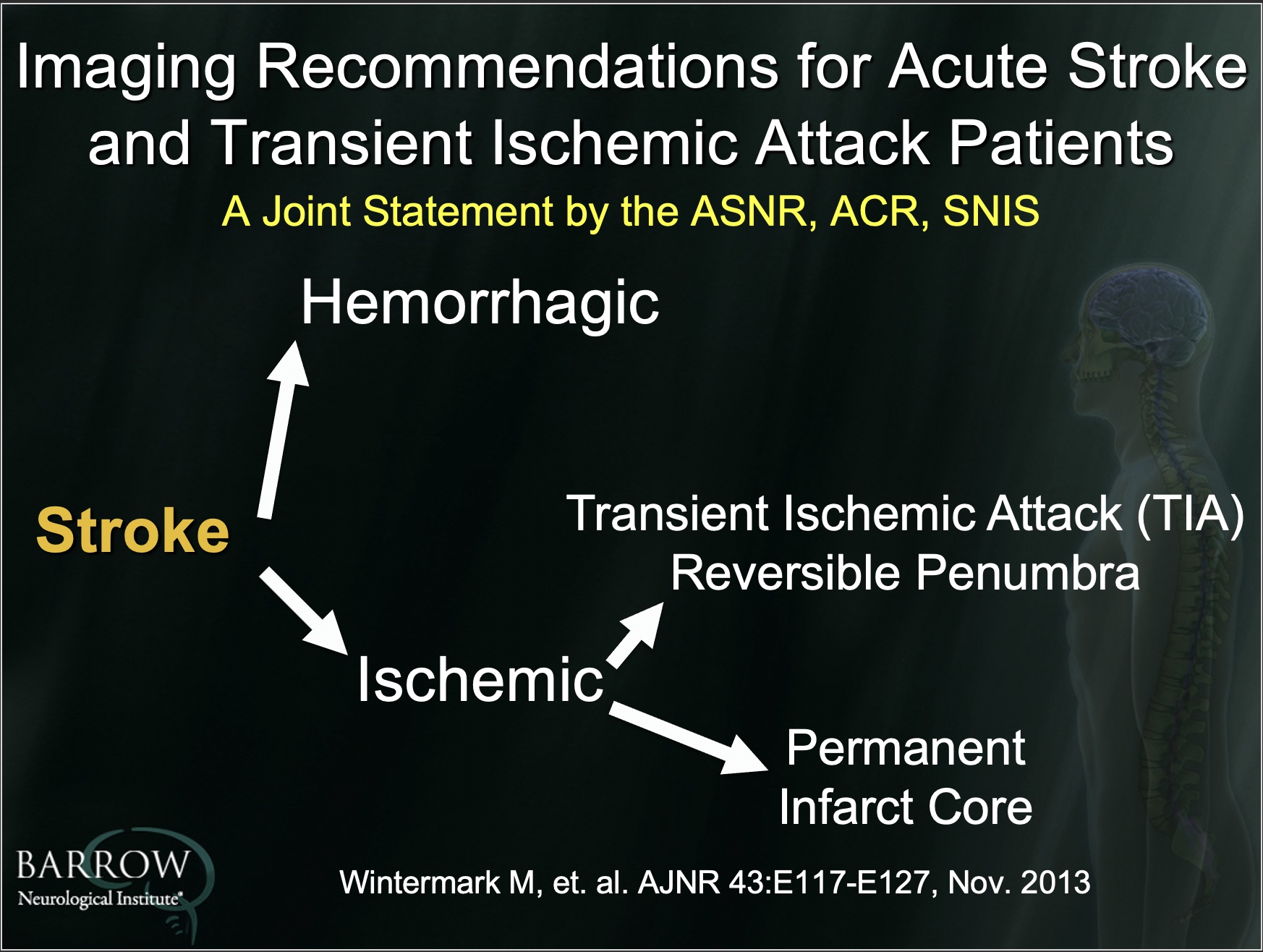
Early identification and intervention in the acute stroke setting can limit neurological damage and vastly improve patient outcomes. In addition to rapidly examining patients presenting to the emergency room with acute stroke symptoms, the goals of imaging should include:
- Differentiating acute ischemic stroke from intracranial hemorrhage;
- Confirming the diagnosis of ischemic stroke versus stroke mimics;
- Identifying whether affected brain tissue is still viable; and
- Identifying the location of vascular occlusion in cases where endovascular therapy is considered.4
That’s according to a recent presentation given by John P. Karis, MD, Director of MRI and Brain Imaging at the Barrow Neurological Institute in Phoenix, AZ.
Despite historical preference for computed tomography (CT) as the modality of choice in detecting acute hemorrhage in the setting of stroke, Dr. Karis said evidence exists showing magnetic resonance imaging equivalence with CT imaging.2 Furthermore, the additional benefits offered by MRI may render it superior to CT imaging in this setting.
In most clinical situations, using CT to confirm an ischemic stroke diagnosis is usually straightforward, but can be unremarkable in the early phases. As noted by Dr. Karis, “this is the area where MRI outperforms CT’s ability… to identify the size of underlying core infarct that's irreversible.” Diffusion-weighted imaging (DWI) is not only more sensitive to ischemic changes within minutes of onset, as well as to ischemic lesions just a few millimeters in size, but its sensitivity for diagnosis increases as time from symptom onset increases.3 With respect to identifying viable tissue, pinpointing the brain area of decreased perfusion is key. Known as the area of penumbra, this area still has the potential for recovery should flow be reestablished; hence, identification by either bolus MR perfusion or bolus CT perfusion is critical to guiding intra-arterial treatment up to 16 hours’ post-symptom onset.1
As for the last goal of imaging, Dr. Karis noted that “CTA [CT angiography] is clearly superior” for identifying the location of vascular occlusion, but that it also “provides more detail than necessary for determining whether carotid or M1 occlusion. For this purpose, he said, evidence suggests that MR angiography (MRA), particularly bolus MRA, is equivalent to CTA.
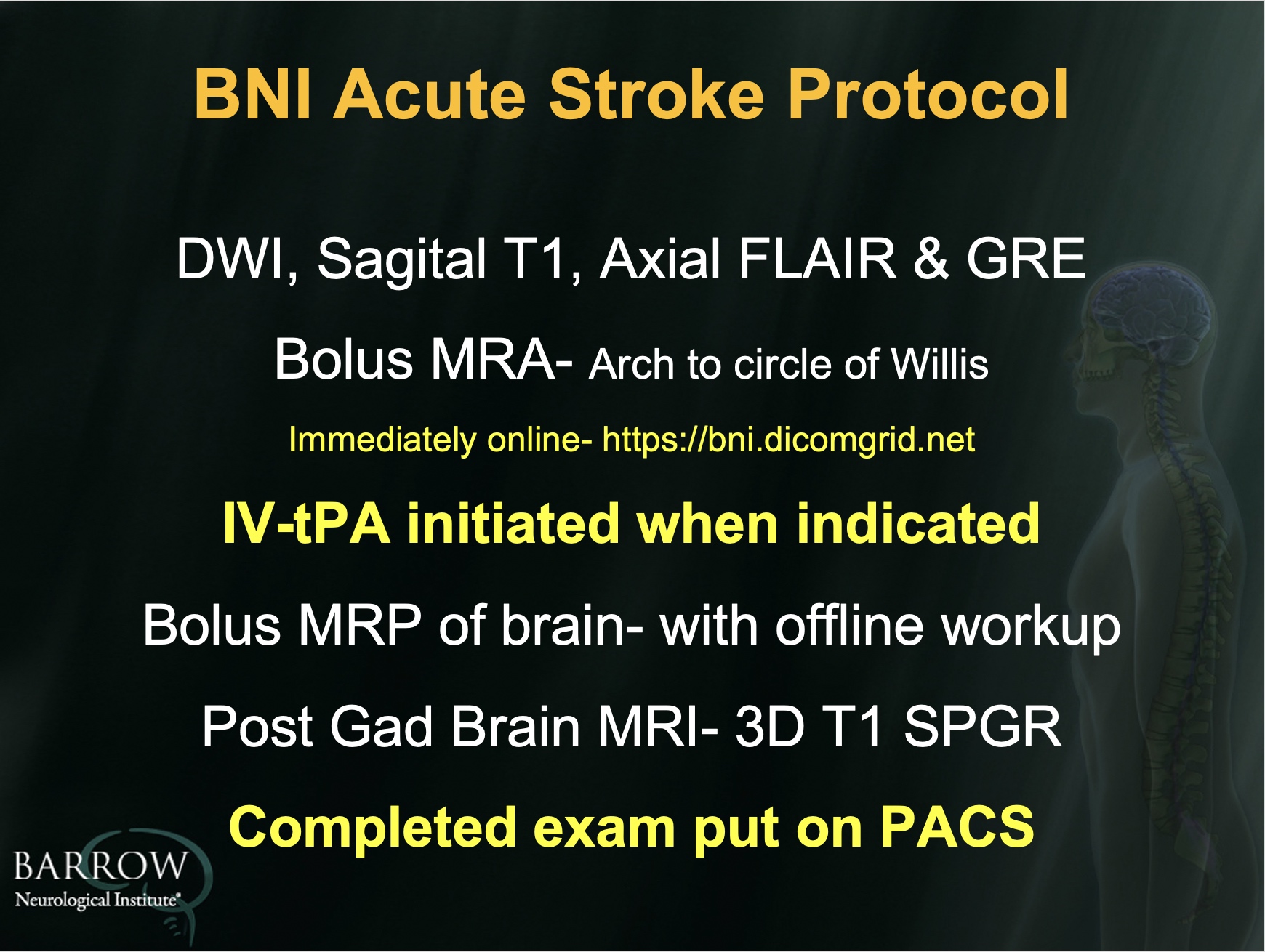
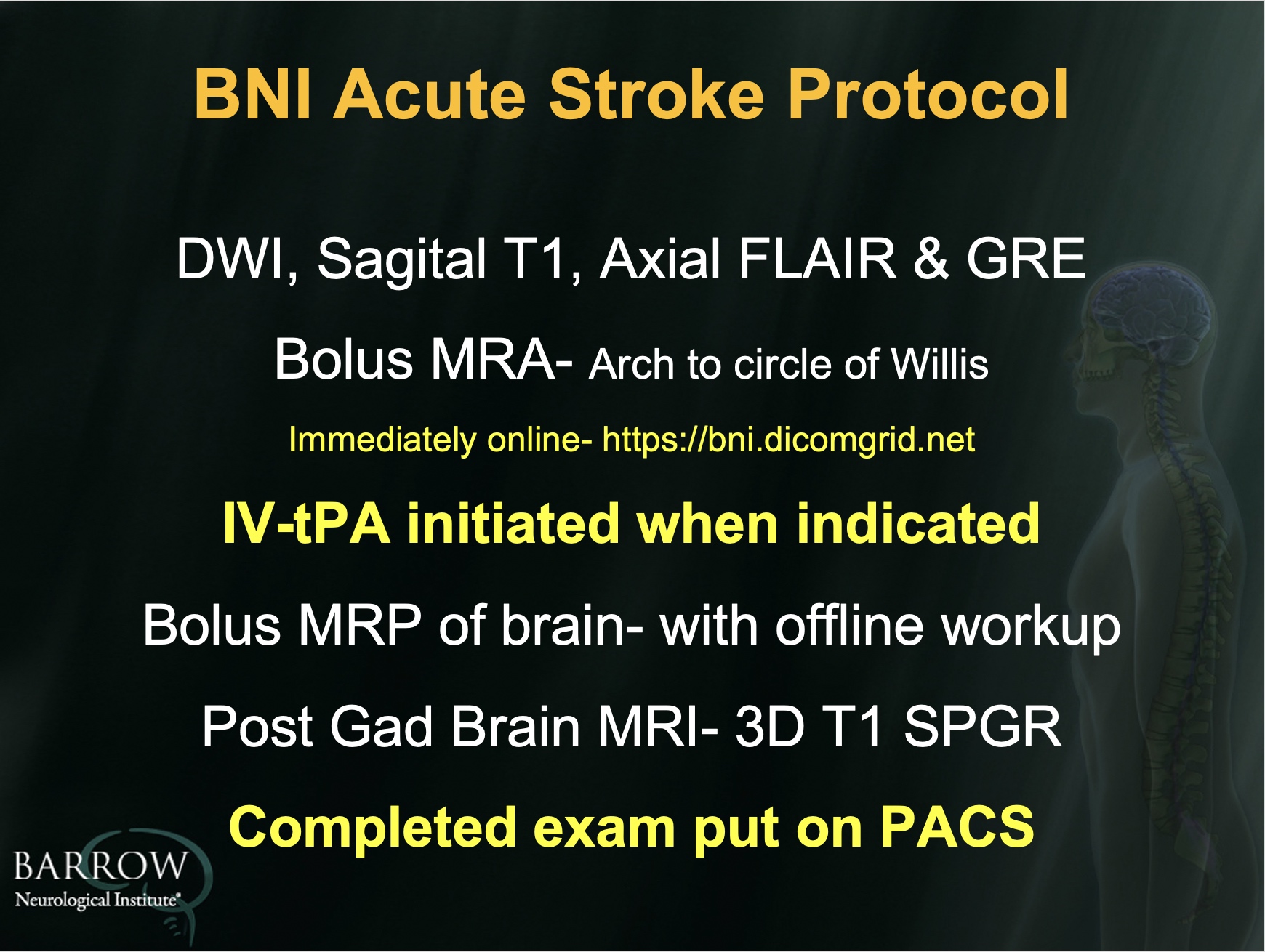
Currently, the Barrow Neurological Institute uses an 8-minute acute stroke MR protocol, which consists of DWI, sagittal T1, axial fluid-attenuated inversion recovery (FLAIR) and gradient-recalled echo (GRE) imaging, followed by a 45-second bolus MRA to determine carotid artery patency through the M1 segments. Imaging is then paused for the clinical team to determine if intravenous tissue plasminogen activator treatment should be initiated. This is followed by bolus MR perfusion, with offline data workup to determine if the patient can potentially benefit from intra-arterial intervention. The Barrow protocol is completed with a post-contrast 3D, T1 scan, which is stereotactically ready for the operating room in event the data are needed.
To successfully implement a rapid MRI protocol for the evaluation of acute stroke in the emergency room environment, Dr. Karis said, the objective should be “to make it fairly indistinguishable in all ways, in terms of turnaround, to a CT scan.” Using a soup-to-nuts approach, he concluded, the infrastructure of the ER environment—from how patients are triaged and transported for imaging to how quickly MR images are interpreted—should be assessed and designed to reduce turnaround times that are similar to typical CT exams for acute stroke.
References
- Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708-718.
- Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007; 369:293-298.
- Sanelli PC, Sykes JB, Ford AL, Lee JM, Vo KD, Hallam DK. Imaging and treatment of patients with acute stroke: an evidence-based review. AJNR Am J Neuroradiol. 2014; 35:1045-1051.
- Wintermark M, Sanelli PC, Albers GW, et al. Imaging recommendations for acute stroke and transient ischemic attack patients: A joint statement by the American Society of Neuroradiology, the American College of Radiology, and the Society of NeuroInterventional Surgery. AJNR Am J Neuroradiol. 2013;34:E117-127.