How we do it: Treatment of a pseudoaneurysm
Images
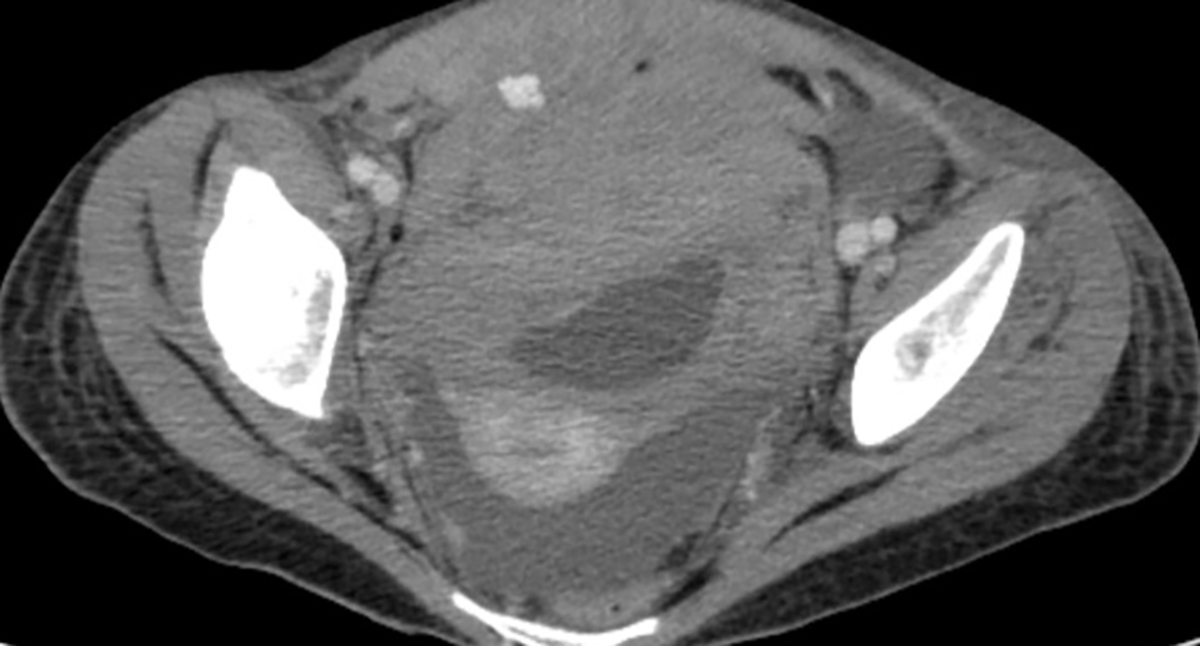
Pseudoaneurysms (PsA) are defined as a collection of blood between the outer two layers of an artery, the media and adventitia. These lesions are uncommon in the pediatric population. The most common causes are penetrating injuries either traumatic or iatrogenic. In contrast, a true aneurysm involves all three layers of the arterial wall and when it dissects, blood tracks between the intima and media. If this blood collection causes sufficient mass effect it may obstruct the vessel lumen. It is likely that in this era of minimally invasive procedures iatrogenic causes are the most common source of PsA, with cardiac intervention the most frequent causation, with up to 8% of involvement of the common femoral artery after a cardiac catheterization with intervention.1-3 Interestingly, PsA are rare in peripheral interventions. This difference is likely due to the presence of one or more predisposing factors in cardiac patient, including: anticoagulant therapy, the use of large devices requiring larger access sheaths that involve a greater percentage of the entry vessel diameter, inadequate compression after removal of the access sheath, not using real-time ultrasound (US) guidance to enter the vessel, and inadvertently entering a femoral artery branch.
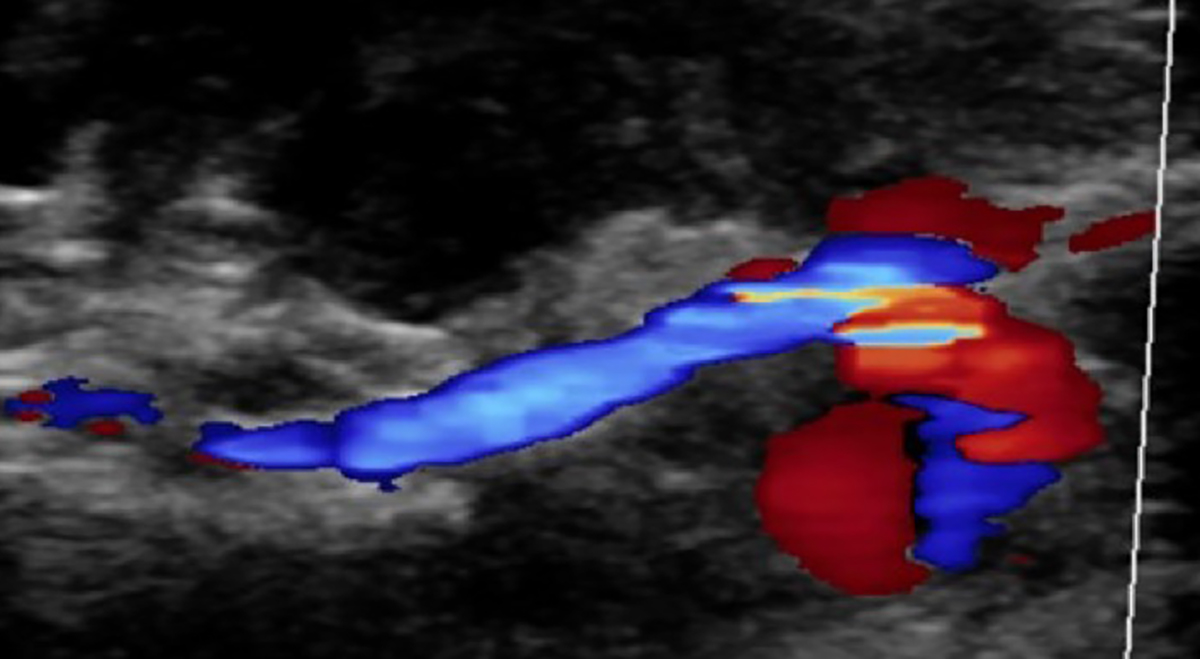
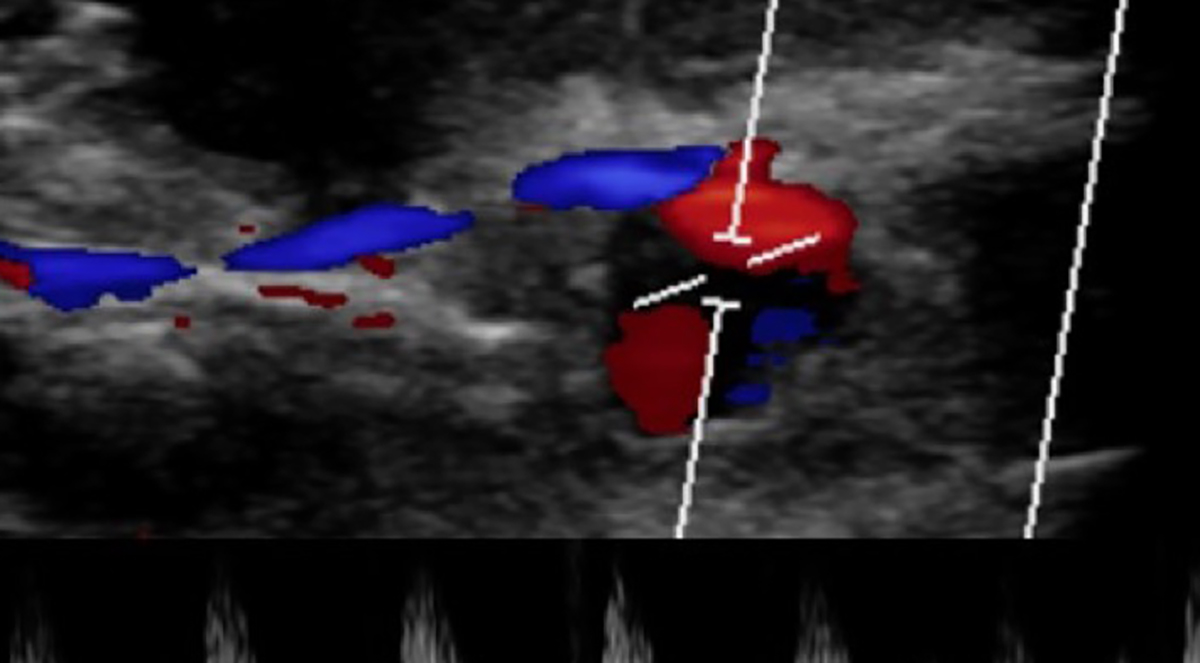
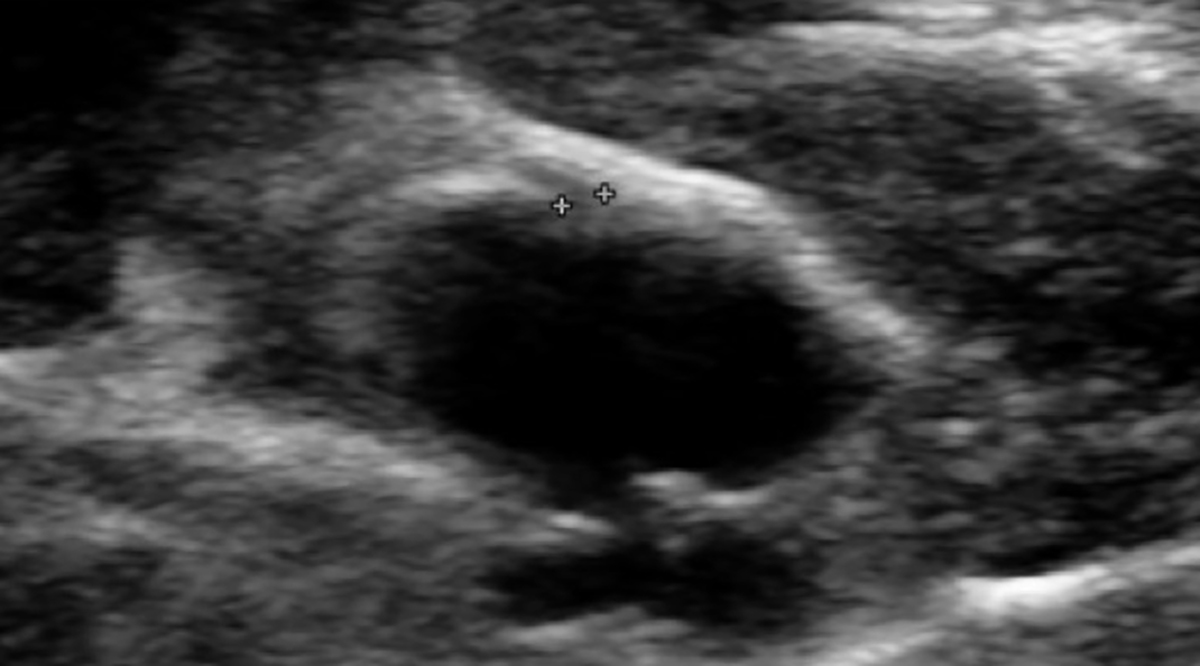
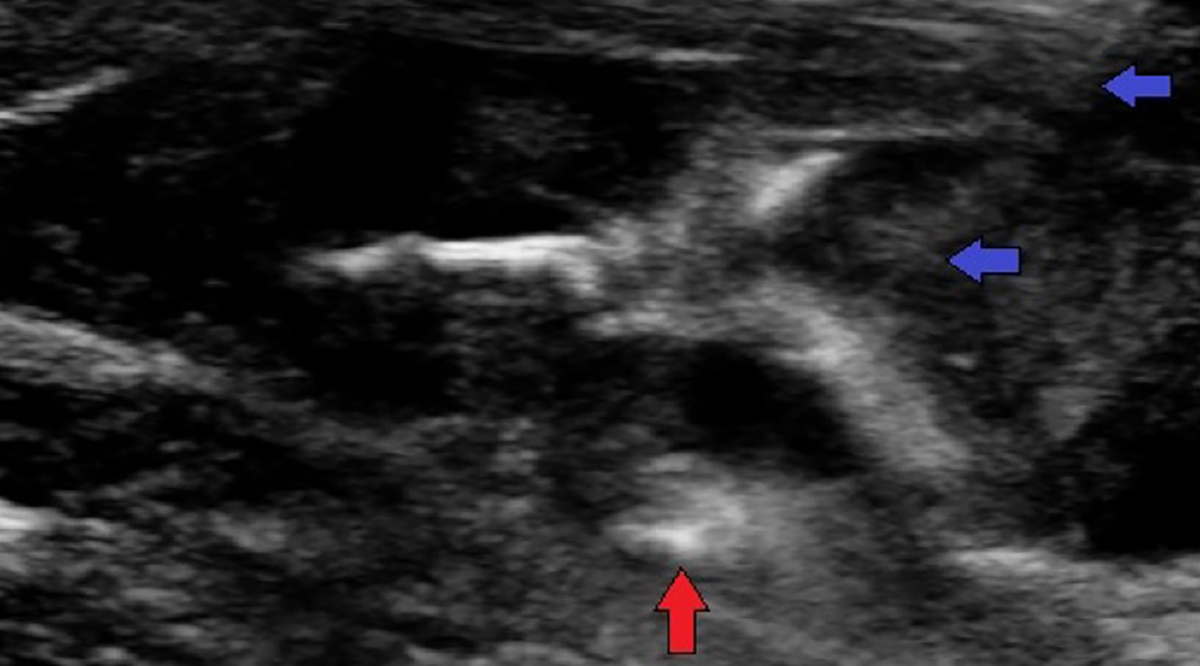
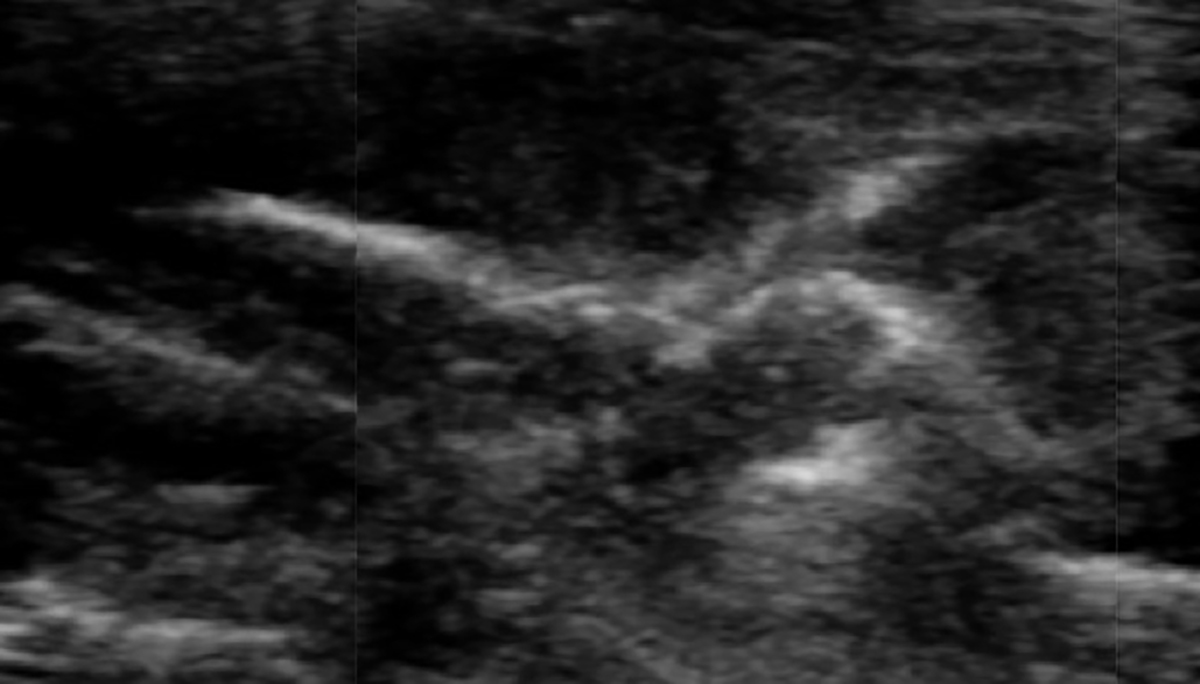
A PsA can occur in any artery in the body.4,5 The clinical presentation of a PsA is usually a tender, pulsatile mass in the region of an artery. There is often associated redness, pain with palpation and warmth of the skin. If there is the suspicion of a PsA, confirmation by US with Doppler examination is indicated. Invariably this study is diagnostic and all that is needed to diagnose and plan therapy. Typically, the US study shows arterial blood flow into the PsA that is chaotic and swirling in its appearance (Figure 1). When a PsA is small it often will spontaneously clot and resolve without therapy; however, larger PAs need therapy since it is unlikely that they will spontaneously resolve. The treatment options for large and/or symptomatic PAs should begin with minimally invasive options. There is literature that shows that compression for 20-30 minutes with an US probe over the neck of the PsA can be effective.1,6 If this choice is pursued it is essential that there is complete occlusion of the arterial inflow to the PsA if success is to be achieved. We do not use this approach because it is quite painful for the patient, has a relatively high failure rate and is time consuming. Our preference is direct US guided puncture of the PsA with thrombin injection into the aneurysm lumen, followed by temporary balloon occlusion for PsA with large necks or those that fail to resolve after thrombin therapy (Figure 2). Alternatively, one can use a covered stent to isolate the PsA with or without thrombin injection, however, this is not an ideal approach for small children since there arterial diameter is small and increasing the risk of arterial occlusion and reduction future arterial growth leading to vessel narrowing. In our experience, a stent is unnecessary since there is a very high probability of success with directed thrombin therapy. As a last resort, there is the option of surgical ligation.
TECHNIQUE
In our experience, the procedure is often performed at bedside in the PICU and the patient is sedated or generally anesthetized. US is used to confirm the patency and location of the PsA. A skin entry site is identified and marked with washable ink. The skin is prepared and draped in sterile fashion and the entry site locally anesthetized with 1% lidocaine with a 27G or 30G needle. Than, using real-time US guidance a 27G puncture needle, 25G angiocatheter or 22G Chiba or spinal needle is guided into the PsA with the needle tip position away from the neck of the aneurysm to minimize the potential for thrombin to enter the arterial lumen (Figure 2A). We often use an angiocath so that the needle can be removed to avoid inadvertent movement of the needle through the far wall of the artery and inadvertent injection in a non-target area. Then, while observing with US, a single drop of thrombin is injected. Almost instantaneously one sees alteration of the flow pattern in the PsA. If, after a minute or two, Doppler shows residual blood flow in the PA the needle is repositioned into this area and a second drop is injected. This is repeated until there is complete cessation of flow. Once flow is no longer identified, it is worthwhile to wait about 5 minutes and re-evaluate the flow with Doppler (Figure 2B). If there is no flow identified the procedure is discontinued. If flow persists, additional thrombin is injected and US follow up is obtained. If flow control is not achieved, alternative options are considered for the following day. It is rare that a PsA remains patent and another therapeutic option is needed.
CONCLUSION
Percutaneous thrombin injection is an effective approach to treat PsA of all types. At this time, percutaneous therapy is the procedure of choice.
REFERENCES
- Morgan R, Belli AM. Current treatment methods for post catheterization pseudoaneurysms. J Vasc Interv Radiol. 2003; 14:697-710
- Kassem HH, Elmahdy MF, Ewis EB, Mahdy SG. Incidence and predictors of post-catheterization femoral artery pseudoaneurysms. Egyptian Heart Journal. 2013: 65(3): 213-221. j.ehj.2012.07.003
- Pelchovitz DJ, Cahill AM, Baskin KM, Kaye RD, Towbin RB. Pseudoaneurysm in children: diagnosis and interventional management. Pediatric Radiology. 2005;35:434-439.
- Safavi A, Beaudry P, Jamieson D, Murphy JJ. Traumatic pseudoaneurysms of the liver and spleen in children: is routine screening warranted? J Pediatr Surg. 2011; 46: 938-941.
- Ello FV, Nunn DB. False aneurysm of the inferior epigastric artery as a complication of abdominal retention sutures. Surgery. 1973; 74:460-461.
- Elford J, Burrell C, Freeman S, et al. Human thrombin injection for the percutaneous treatment of iatrogenic pseudoaneurysms. Cardiovasc Intervent Radiol. 2002; 25:115-118.