Hand masses: An Essential MRI review
Images

This article is accredited for one SA-CME credit. Visit appliedradiology.org/SAM2 for full SA-CME information.
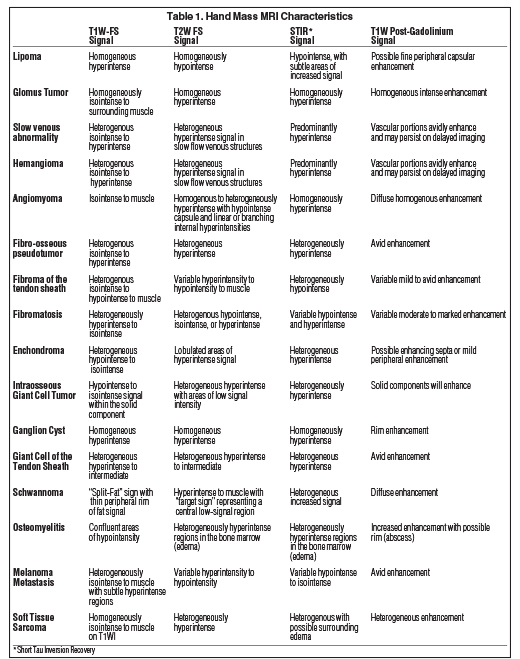
Hand masses, a common clinical entity, frequently prove to be benign; however, nonspecific clinical presentations and overlapping imaging findings often create a dilemma in clinical management. In this review, we systematically discuss and illustrate masses of the hand categorized into neuro-vascular tumors, fibrous lesions, benign primary bone/cartilage tumors, degenerative (reactive) lesions, benign primary soft tissue tumors, as well as primary malignancies, mimics, and metastases. We briefly review pertinent characteristics of each lesion, illustrate magnetic resonance (MR) imaging findings, and correlate with histological findings. The recognition of imaging patterns, size, location, and relationship to neighboring structures significantly narrows the differential diagnosis and helps to guide clinical management in a multidisciplinary approach (Table 1).
Imaging technique
Representative MR imaging studies were performed on either a 3.0-T Siemens scanner (Siemens Corp., Washington, DC) or a 1.5-T Siemens scanner (Siemens Corp., Washington, DC). Standard pulse sequences were performed with small field-of-view (FOV) 10-12 cm, high resolution matrix (320 x 344), and dedicated coil used when possible. Standard sequences included T1-weighted turbo spin-echo (T1W), T2-weighted turbo spin echo with fat saturation (T2WFS), Short Tau Inversion Recovery (STIR), T1 weighted spin-echo without fat-saturated (T1WFS) and IV contrast administration (T1WFS C+) with the use of orthogonal planes through the mass and adjacent structures when necessary. Gadopentetate dimeglumine, 0.1 mmol/kg (Bayer, Whippany, NJ) was used for gadolinium administration.
Benign primary soft tissue tumors
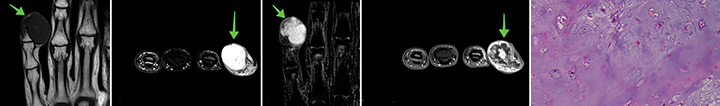
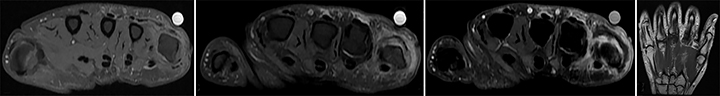
Lipomatous lesions
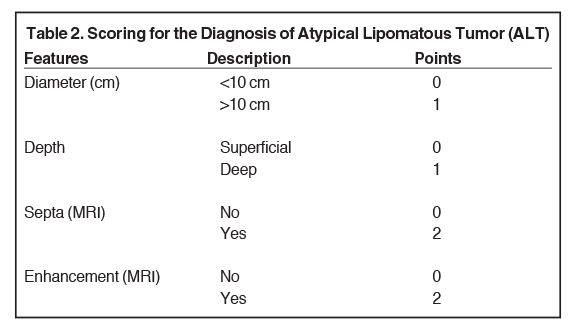
Lipomatous lesions are exceedingly common and comprise nearly 50% of all soft tissue tumors, with the largest prevalence in the 5th-7th decades of life.1 These lesions exist along a spectrum ranging from benign (ie, lipomas) to atypical lipomatous tumors, with the most malignant representing liposarcomas.2 MR characteristics that help establish benignity include a well-circumscribed lesion with hyperintense signal on T1-weighted images (T1WI), hyperintense signal on T2-weighted images (T2WI), homogenous signal loss on fat-suppressed sequences, low signal on short-tau inversion recovery (STIR) or frequency selective fat suppressed images, and limited fine peripheral capsular enhancement.1, 2 MR findings which suggest an underlying malignant process include size >10 cm, thick septae, and globular or nodular soft tissue enhancement. Recent attempts at differentiating lipomas versus atypical lipomatous tumors and underlying malignancies have been developed with an atypical lipomatous tumor (ALT) scoring system to help guide clinical management. ALT incorporates lesion diameter: 0-10 cm (0) or >10 cm (1); depth, superficial (0) or deep (1); septa: no (0) or yes (2); and enhancement: no (0) or yes (2). Lesions with total scores greater than or equal to 3 should lead to biopsy/pathologic correlation due to suspicious features (Figure 1, Table 2).3
Neurovascular masses
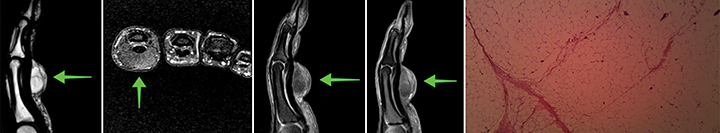
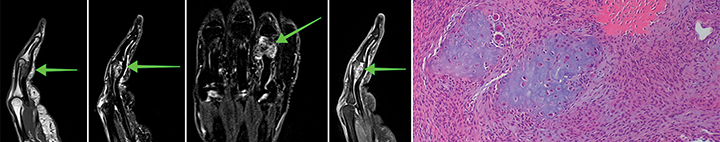
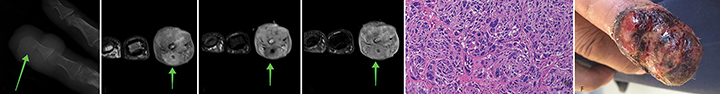
Glomus tumor
Glomus tumors are benign masses arising from the neuromyoarterial apparatus of the glomus bodies, which are responsible for thermoregulation.4,5 Clinically, the tumor presents as a small, reddish mass found in a typical subungual location in 25-65% of all cases and is usually seen in patients between 40 and 50 years of age. Lesions typically cause a triad of pain, sensitivity to temperature changes, and point tenderness.4 -7 Despite the fact patients seek help early, the lesion is often too small to be recognized on physical exam.8 A subungual location in conjunction with homogeneous high signal intensity on T2WI, low or intermediate signal on T1WI, and uniform enhancement after contrast administration are characteristic (Figure 2).6, 7
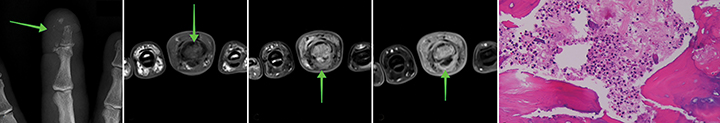
Schwannoma
Schwannomas are benign, slow-growing tumors originating from the epineurium of peripheral nerves and usually affect adults in the third decade of their lives.9 Tumors may grow for years prior to being diagnosed and rarely exceed three centimeters in diameter.10 Clinically, schwannomas present as palpable solitary, painless lesions on the volar aspect of the wrist causing entrapment syndrome with paraesthesia, hypoaesthesia, and pain. Constituting approximately 0.8-2.0% of all hand tumors, schwannomas are considered rare and involve the upper twice as often as the lower extremities.11 Neurofibromas, ganglion cysts, tumors, lipomas, and xanthomas need to be considered as possible differential diagnoses.10 Histologically, schwannomas stain positive for S100 (marker for neuroectodermal cells), and present with an areas of spindle cells and nuclear palisading (Antoni A) next to hypocellular, myxoid regions (Antoni B).10, 11 On MRI, schwannomas show intermediate to low signal on T1-weighted images and increased diffuse signal on T2WI. Contrast enhancement on T1WI is particularly helpful in their diagnosis, with diffuse enhancement and central areas of low signal being characteristic (target sign, Figure 3).10
Vascular abnormalities
Slow flow venous abnormality
Vascular abnormalities of the hand and wrist are relatively uncommon and considered non-neoplastic lesions resulting from alterations in signaling during development and vessel morphology.4, 12 They are usually present at birth and grow proportionally with the child but may not be diagnosed until adulthood.4, 12 Congenital vascular malformations account for 2-6% of all upper extremity tumors and are evenly distributed between genders.12 Depending on the vascular components involved, masses can be of capillary, venous, arterial or lymphatic origin and can be classified based on their hemodynamic status as low flow (lymphatic, venous, capillary) or high flow (arteriovenous).4, 12 Venous abnormalities are the most frequently encountered vascular malformation and clinically present as swelling with skin changes, and bone hypoplasia in 33% of all cases.7 Slow flow venous abnormalities present with localized pain that can be intensified by physical activity due to thrombosis and dilatation.12 Vessels resemble dilated vascular spaces with slow flow and septated channels, and appear as hyperintense masses on T2WI. Lesions lack high flow velocity signal voids and are isointense to muscle on T1WI.4 Enhancement of the vascular spaces can be uniform or inhomogeneous.4 Contrasted to arteriovenous malformations, which are more commonly encountered in the head and neck, present on MR imaging as a tangle of vessels with no prominent soft tissue component, vascular shunting, often contain thrombosis, calcification, and possible adjacent lipomatous hypertrophy (Figure 4).
Hemangioma
Hemangiomas are predominantly found in younger patients, occur more often in females, and represent the fourth most common tumor of the hand.8 Distinctly, hemangiomas feature a period of rapid growth with endothelial cell proliferation followed by stagnation and eventually spontaneous involution, a fact that allows distinction from vascular malformations that grow proportionally with the child.12 Superficial hemangiomas present with characteristic skin discolorations, and can therefore usually be easily diagnosed by visual inspection alone. If imaging is needed to classify the mass, hemangiomas are usually hyperintense on T2WI as a result of decreased blood flow and subsequent increased fluid content, and frequently display lobulations and septations.6 Masses are iso- to hyperintense to muscle on T1WI, with larger lesions containing fat, smooth muscle, myxoid tissue, thrombi, hemosiderin, and fluid levels.6 As a distinct feature, muscle atrophy in the periphery of the lesion has been described secondary to chronic ischemia due to a shunting phenomenon caused by the mass (Figure 5).5
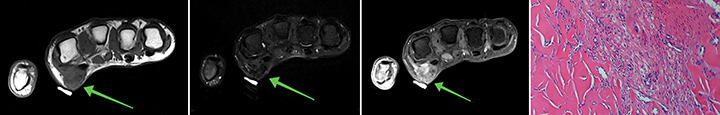
Angiomyoma
Angiomyomas account for 5% of all benign tissue neoplasms, and are characteristically well-defined, grow slowly, found in the dermis, subcutaneous fat, or superficial fascia of the extremities predominantly.9, 13 They represent proliferations of smooth muscle of the venous tunica media and are associated with pain in 58% of patients, which increases in intensity with distal locations.9 Digital masses are more frequently located in the fingers than in the toes with a 4-3:1 ratio, and show an equal gender distribution.9 Digital lesions appear isointense or slightly hyperintense compared to skeletal muscle on T1-weighted imaging (T1WI), hyperintense on T2-weighted imaging (T2WI), and enhance on T1WI after contrast administration.13 A peripheral rim of low signal on T1 and T2WI resembles a fibrous pseudocapsule, and an enhancing vascular structure may accompany the mass resulting in signal heterogeneity on T2WI (Figure 6).13
Fibrous (reactive) lesions
Fibro-osseous pseudotumor
Fibro-osseous pseudotumors are rare, benign, but locally aggressive ossifying soft tissue lesion with approximately 100 documented cases in the literature, typically found in the digits of young adults. This entity is thought to represent a reactive process (eg, repetitive trauma) rather than a neoplasm, and considered to be a subcutaneous soft tissue variant of myositis ossificans.11,14-16 Lesions are confined to the dermis and subcutis and may cause a periosteal reaction. Clinical diagnosis is difficult and lesions are often misdiagnosed as malignant with subsequent radical excision or amputation.11 Symptoms occur over weeks or months and are associated with pain, redness, and affect functionality.11 Patients in the 4th decade of their lives are more frequently affected with a slightly higher female prevalence.11 Radiologic findings often include a radiolucent band between the mass and cortex as well as a focal soft tissue swelling with associated calcification and may be differentiated from myositis ossificans by a lack of well-defined zoning pattern.14 MR findings are generally of T1W/T2W hyperintensity with mild heterogeneous enhancement. Occasionally, in its earliest phase, the lesion may present with aggressive-appearing features, including periosteal thickening and local cortical erosion, which may favor inclusion of juxtacortical osteosarcoma in the differential diagnosis.14-16 Clinical history, close interval follow-up, and if necessary pathologic tissue correlation may be required to establish benignity (Figure 7).
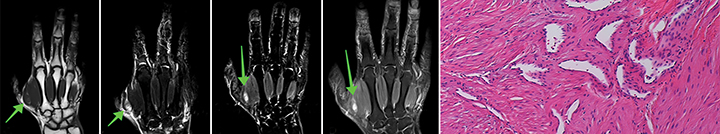
Fibroma of the tendon sheath
Fibromas of the tendon sheath are rare, benign tumors directly involving the tendon sheath thought to be secondary to local reactive processes rather than a neoplastic pathology. Lesions occur most commonly in the hand and wrist in 82% of all cases, and are more frequently found in men (3:1) in the 4th decade of life.2, 8 Fibromas may directly involve the neurovascular bundle, can locally recur after resection, and have no malignant potential. Fibromas of the tendon sheath are often challenging to diagnosis as the lesion typically shares nonspecific imaging characteristics with other tumors of the tendon sheath (mostly giant cell tumors) and soft tissue sarcomas.6,8 MR imaging features include mixed T1W and T2W appearance based on variability in composition (low T1W signal in fibrous regions and heterogeneous T2W signal in cellular/stromal regions), and typically a lack of enhancement. Distinguishing MR features include a lack of blooming artifact on gradient recalled echo (GRE) sequences and no evidence of bony scalloping, both of which are more commonly seen in giant cell tumors of the tendon sheath (GCTTS, Figure 8).2
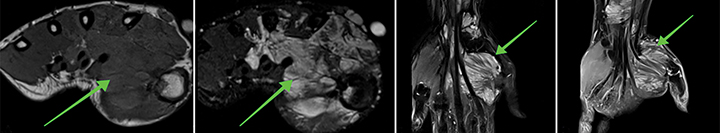
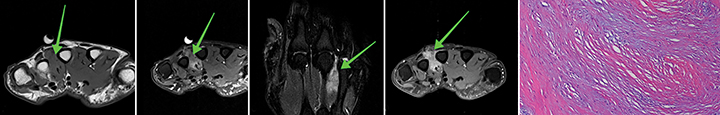
Fibromatosis (pathologic origin)
Fibromatosis is a benign, occasionally locally aggressive and infiltrative lesion without metastatic potential, representing a proliferative disorder of mature fibroblasts.15, 17, 18 Lesions are thought to be multifactorial in pathogenesis (genetic, endocrine, traumatic, and/or microvascular injury) and are categorized as superficial or deep. Superficial locations include palmar and plantar fibromatosis. Palmar fibromatosis (referred to as Dupuytren disease) occurs more commonly in men (3:1) over the age of 65 and plantar fibromatosis (referred to as Ledderhose disease) occurs mostly in men (2:1) aged 30-50 years. Contributing factors include diabetes, alcoholism, and chronic liver disease. Deep fibromatoses occur most frequently in women in the 2nd and 4th decades of life, and tend to be more locally aggressive.17, 19 MR imaging typically demonstrates T1W intermediate to hypointense signal, T2W hyperintense signal with hypointense bands, and avid enhancement in T2 hyperintense regions (Figure 9).
Benign primary bone/cartilage tumors
Enchondroma
Enchondromas are the most common primary bone tumors and account for 12 - 24 % of all benign bone tumors and almost 3 % of all bone tumors overall.10,20 Approximately 35% of all enchondromas can be found in the hand, accounting for almost 90% of all primary hand bone tumors.21 They are considered a proliferation of hyaline cartilage in the metaphyseal-diaphyseal region of bones with endochondral ossification.20 Enchondromas are slow growing, develop in patients between 30 and 40 years of age, and commonly affect the ulnar sided tubular bones with the proximal phalanges most frequently involved.10 They are usually incidental findings associated with pathological fractures in 40-60% of all cases on initial presentation.10,20 On MRI, enchondromas appear as well demarcated masses with intermediate to low signal on T1 WI, high signal on T2WI with decreased signal due to calcifications, and variable enhancement after contrast administration (Figure 10).20
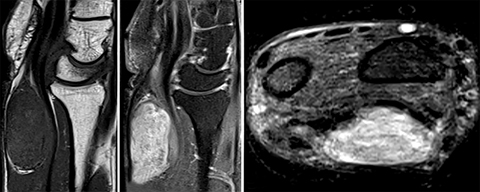
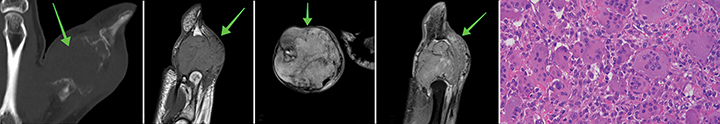
Intraosseous giant cell tumor
Giant cell tumors (GCT) are benign but locally aggressive neoplasms typically found in the epiphysis of long skeletal bones in patients 20 to 40 years of age.22 Only 2% of all GCT are located in the hand, and present with progressive pain, swelling and pathological fracture due to the lytic nature of the lesion, without calcifications, sclerosis, or periosteal reaction.22 GCTs can be classified as Grade 1 (corresponds to a latent, cystic lesion with sclerosed margins), an active Grade 2 (the most common type, characterized by a thin cortex but no extension into the surrounding tissue), and Grade 3 (identifiable by a perforated cortex and invasion of the neighboring tissue).22 The three stages described correlate to aggressiveness and risk of recurrence.22 Intraosseous giant cell tumors typically present with hypointense to isointense signal within the solid component on T1WI, heterogenous T2W signal, and enhancement of the solid components after gadolinium administration on T1WI (Figure 11).23
Degenerative (reactive) lesions
Ganglion cyst
Ganglion cysts make up a large percentage (60-70%) of frequently diagnosed masses of the hand and wrist, are mostly seen in young women in the second to fourth decades of their lives, and resemble degenerated connective tissue as a consequence of chronic irritation or as a result of repetitive microtrauma.4,6,7,24 Clinically, these mucin-filled synovial cysts present as painful lesions that may compress the median or ulnar nerve and are usually between 1-3 cm in size.7,24 Masses appear uni-or multilocular and predominantly involve the dorsum of the wrist (60%), where they often arise from the scapholunate joint.4,6 Volar masses (20%) usually originate from the radio-scaphoid, scapho-trapezial, or metacarpotrapezial joint.4 Involvement of the flexor tendon sheath (10%) and distal interphalangeal joint (10%) occur less commonly.4 Low signal on T1WI and high signal on T2WI are typical imaging findings. Signal may be altered to iso- or hyperintensity on T1 WI due to proteinaceous or hemorrhagic content, and mild enhancement of the capsule and septae can be visualized after gadolinium administration (Figure 12).4, 5
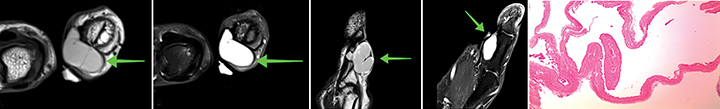
Giant cell tumor of the tendon sheath
Giant cell tumors of the tendon sheath (GCTTS) are the second-most common hand masses and appear as benign, painless, well-defined masses involving the tendon sheath in the volar aspect of the hand, slightly favoring women 30-50 years of age.4 6,7 GCTTS are thought of as reactive lesions associated with degenerative processes rather than a neoplasm, but expansive growth may result in pressure changes of adjacent structures and affect hand function.6 ,7 Recurrence rates after surgical excision of up to 44 % have been reported.7 Hypointensity on T1WI and T2WI are characteristic imaging findings and may be accompanied by areas of low and high signal intensities on T2WI due to hemosiderin deposits and fluid accumulation.4,6 Susceptibility artifacts on GRE sequences and strong enhancement due to capillary proliferation are typical and can aid in the diagnosis (Figure 13).6
Malignancies, metastases, and mimics
Epithelioid sarcoma
Epithelioid sarcomas are the most common primary soft tissue sarcoma of the hand and are usually diagnosed in young men 20-30 years of age as a firm, nontender tumor of the distal upper extremity.22,25 Epithelioid sarcomas usually have a benign presentation with slow progression, often misdiagnosed as chronic inflammation, necrotizing granulomas, or fibrohistiocytic tumors.25 Lesions are initially solitary but may become multiple with disease spreading along tendons, fascia, and aponeurosis. As the tumor progresses, necrosis, hemorrhage, ulceration, and periosteal bone invasion become characteristic, as well as involvement of regional lymph nodes and metastases.25 Metastatic rates of up to 50% can be seen and predominantly involve the lung.25 Local recurrences within 1-2 years after treatment are common and are usually associated with a worse clinical outcome.25 Histologically, epithelioid sarcomas can be classified as epithelioid, spindled, or mixed and stain positive for vimentin, epithelial membrane antigen, and cytokeratin.25 MRI with contrast demonstrates the hypervascularity of the lesion, the extent of necrosis and involvement of neighboring structures. Epithelioid sarcomas are isointense to muscle on T1WI and hyperintense on T2WI with superficial lesions appearing homogenous with heterogenous deep lesions (Figure 14).22
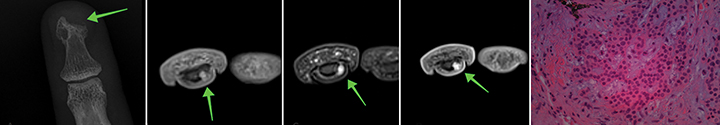
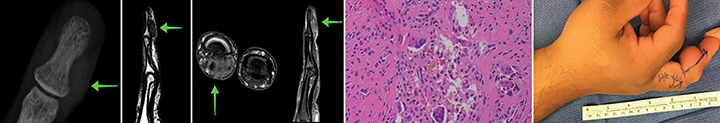
Malignant masses (primary and metastatic melanoma)
Malignant lesions of the hand are rare and often carry a poor prognosis. Examples include sarcomas, malignant nerve sheath tumors, and metastatic lesions with primary tumors predominantly located in the lung, breast, or kidney.2,8,19,26 Malignant tumors characteristically present as destructive lytic lesions, have poorly defined margins, are edematous, lobulated, and show signs of hemorrhage and necrosis.8 Melanomas of the hand account for 3% of all hand tumors.7 Demonstrated in this specific case series, examples of primary and metastatic melanoma have a unique MR imaging appearance. Primary melanoma can be differentiated from metastatic melanoma since primary lesions are contiguous with the skin. Several studies have shown the degree of increased T1W signal often correlates directly with melanin content.26,27 although it has been theorized that bound biologic paramagnetic substances to the melanin may be the causative agent rather than melanin itself.27 T2W signal is often heterogeneous, which may be secondary to hemorrhagic products. Melanoma lesions typically enhance avidly after gadolinium administration (Figure 15).
Osteomyelitis
Osteomyelitis is most commonly caused by S. aureus and Streptococcus organisms, resulting in pain, swelling, and erythema.28 Soft tissue and osseous infections of the hand are common and can often mimic soft tissue masses. Infection in the hand and wrist are mostly caused by direct inoculation of pathogens after trauma or surgery, but may also result from local or hematogenous spread.29 Spread of the pathogen along the anatomical planes (usually traumatized bone) subsequently results in osseous necrosis.29 Common risk factors for hand infections include immunocompromise, drug and alcohol abuse, inflammatory arthropathy, peripheral vascular disease, and renal failure.30 Careful attention to clinical history and anatomic detail is paramount in investigating a potential hand infection or soft tissue mass. Radiographic findings include identification of soft tissue swelling or ulceration with possible local periosteal reaction or erosions. Osteolysis is present in 70% of all cases, followed by osteopenia (10%), osteosclerosis (10%), and periosteal reactions (10%).28 Identification of osteomyelitis on MR includes confluent regions of low signal intensity on T1W images, increased signal on fluid-sensitive sequences, and avid contrast enhancement (Figure 16).19,30,31
Conclusion
Soft tissue masses of the hand and wrist are common in clinical practice, and while most masses are benign, MR plays a vital role in deciphering the preoperative diagnosis and guiding clinical management. While overlapping MR findings may necessitate the need for clarification with clinical history, follow-up imaging, or additional pathologic correlation, the radiologist should be familiar with various benign, malignant, and potential tumor mimics to develop and narrow the differential diagnosis.
References
- Murphey MD, Carroll JF, Flemming DJ, et al. From the archives of the AFIP: benign musculoskeletal lipomatous lesions. Radiographics. 2004;24(5):1433-1466.
- Lee CH, Tandon A. Focal hand lesions: review and radiological approach. Insights Imaging. 2014;5(3):301-319.
- Nagano S, Yokouchi M, Setoguchi T, et al. Differentiation of lipoma and atypical lipomatous tumor by a scoring system: implication of increased vascularity on pathogenesis of liposarcoma. BMC Musculoskelet Disord. 2015;16:36.
- Teh J, Whiteley G. MRI of soft tissue masses of the hand and wrist. Br J Radiol. 2007;80(949):47-63.
- Morris CJ, Younan Y, Singer AD, et al. Masses of the hand and wrist, a pictorial review. Clin Imaging. 2016;40(4):650-665.
- Lee CH, Tandon A. Focal hand lesions: review and radiological approach. Insights Imaging. 2014;5(3):301-319.
- Henderson MM, Neumeister MW, Bueno RA, Jr. Hand tumors: I. skin and soft-tissue tumors of the hand. Plast Reconstr Surg. 2014;133(2):154e-164e.
- Lee CH, Tandon A. Focal hand lesions: review and radiological approach. Insights Imaging. 2014;5(3):301-319.
- Hammond MI, Miner AG, Piliang MP. Acral and digital angioleiomyomata: 14-year experience at the Cleveland Clinic and review of the literature. J Cutan Pathol. 2017;44(4):342-345.
- Lubahn JD, Bachoura A. Enchondroma of the hand: Evaluation and management. J Am Acad Orthop Surg. 2016;24(9):625-633.
- Zhou J, McLean C, Keating C, et al Fibro-Osseous pseudotumour of the digit: An illustrative case and review of the literature. Hand Surg. 2015;20(3):458-462.
- Ek ET, Suh N, Carlson MG. Vascular anomalies of the hand and wrist. J Am Acad Orthop Surg. 2014;22(6):352-360.
- Yoo HJ, Choi JA, Chung JH, et al. Angioleiomyoma in soft tissue of extremities: MRI findings. AJR. Am J Roentgenol. Jun 2009;192(6): W291-294.
- Javdan M, Tahririan MA. Fibro-osseous pseudotumor of the digit. Adv Biomed Res. 2012; 1:31.
- Kwak, M, Kim S, Lee S, et al. Radiological features of a fibro-osseous pseudotumor in the digit: A case report. J Korean Soc Radiol. 2015; 73(2):131-135.
- Kransdorf MJ, Meis JM. From the archives of the AFIP. Extraskeletal osseous and cartilaginous tumors of the extremities. Radiographics. 1993;13(4):853-884.
- Murphey MD, Ruble CM, Tyszko SM, et al. From the archives of the AFIP: musculoskeletal fibromatoses: radiologic-pathologic correlation. Radiographics. 2009;29(7):2143-2173.
- Zgonis T, Jolly GP, Polyzois V, et al. Plantar fibromatosis. Clin Podiatr Med Surg. 2005;22(1):11-18.
- Teh J, Whiteley G. MRI of soft tissue masses of the hand and wrist. Br J Radiol. 2007;80(949):47-63.
- Larbi A, Viala P, Omoumi P, et al. Cartilaginous tumours and calcified lesions of the hand: a pictorial review. Diagn Iinterv Imaging. 2013;94(4):395-409.
- Cavit A, Ozcanli H, Sancmis M, et al. Tumorous conditions of the hand: A retrospective review of 402 cases. Turk Patoloji Derg. 2018;34(1):66-72.
- van Vliet M, Kliffen M, Krestin GP, et al. Soft tissue sarcomas at a glance: clinical, histological, and MR imaging features of malignant extremity soft tissue tumors. Eur Radiol. 2009;19(6):1499-1511.
- STATDX https://my.statdx.com/
- Gregush RE, Habusta SF. Cyst, Ganglion. Treasure Island, FL: StatPearls Publishing LLC.; 2018.
- Sobanko JF, Meijer L, Nigra TP. Epithelioid sarcoma: a review and update. J Clin Aesthet Dermatol. 2009;2(5):49-54.
- Wu JS, Hochman MG. Soft-tissue tumors and tumorlike lesions: a systematic imaging approach. Radiology. 2009;253(2):297-316.
- Blacksin MF, Ha DH, Hameed M, et al. Superficial soft-tissue masses of the extremities. Radiographics. 2006;26(5):1289-1304.
- McDonald LS, Bavaro MF, Hofmeister EP, et al. Hand infections. J Hand Surg. 2011;36(8):1403-1412.
- Honda H, McDonald JR. Current recommendations in the management of osteomyelitis of the hand and wrist. J Hand Surg. 2009;34(6):1135-1136.
- Patel DB, Emmanuel NB, Stevanovic MV, et al. Hand infections: anatomy, types and spread of infection, imaging findings, and treatment options. Radiographics. 2014;34(7):1968-1986.
- Collins MS, Schaar MM, Wenger DE, et al. T1-weighted MRI characteristics of pedal osteomyelitis. AJR. Am J Roentgenol. 2005;185(2):386-393.
Citation
Hardin N, Laks S, Smith C, Mullins C, Padilla O, Kafchinski L. Hand masses: An Essential MRI review . Appl Radiol. 2019;(3):12-21.
June 7, 2019