Gossypiboma
Case Summary
A patient presented with poor healing at the site of a prior tracheostomy. Laboratory work demonstrated a normal white blood cell count.
Imaging Findings
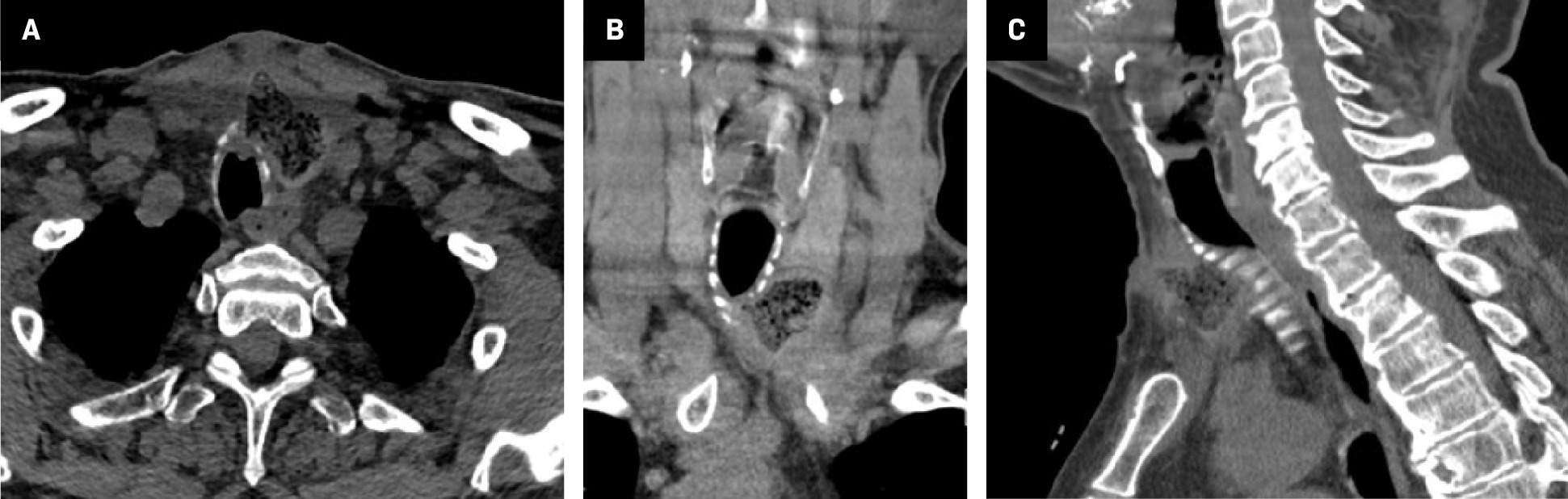
Noncontrast neck CT demonstrated a well-defined region of gas bubbles anterolateral to the trachea and deep to the tracheostomy site, with surrounding soft-tissue thickening ( Figure 1 ).
An axial CT image of the neck ( A ) demonstrates a well-defined collection of gas bubbles anterolateral to the trachea. Coronal ( B ) and sagittal CT ( C ) reformations show soft-tissue thickening surrounding the lesion.
Diagnosis
Gossypiboma.
Differential diagnosis includes abscess and tracheocutaneous fistula.
Discussion
Gossypiboma, also known as a textiloma, is a mass formed of retained cotton foreign bodies from surgical procedures, such as sponges. This hybrid word combines the Latin term gossypium (cotton) and the Kiswahili term boma (place of concealment).1 In our case, the gossypiboma was formed by a 4 × 4 gauze pad.
Despite widespread implementation of preventive measures such as standardized item counts, new gossypiboma cases continue to be reported in the literature. The incidence of retained foreign bodies, including textiles, is difficult to ascertain; however, it is estimated to occur in approximately 1 in every 1000 to 1500 abdominal surgeries.2
Cotton foreign bodies commonly induce either granuloma formation via an aseptic fibrinous response or abscess formation via an exudative response. Objects associated with abscess formation are more frequently detected earlier in the postoperative period than those that lead to granuloma formation. In a case series reviewing 14 patients with gossypibomas, 2 patients showing an exudative response presented at 1 and 22 months following their causative procedure, while those with an aseptic fibrinous response presented between 1 year and 40 years postoperatively.3
Clinical presentation widely varies based on size and location of the retained foreign body. These masses most frequently occur in the abdomen or pelvis, while occurrence in the neck is rare. Between 2012 and 2017, 0.7% of retained surgical sponges reported to The Joint Commission were found within the neck.4 Gossypibomas of the neck may present as a palpable mass, change in voice, difficulty breathing, or draining sinus tract.5 However, they may be asymptomatic and discovered incidentally.
CT is the study of choice for diagnosing gossypibomas. They most commonly present as a low-density, heterogeneous mass with an external contrast-enhancing, high-density wall, with an internal spongiform pattern containing air bubbles.6 Most surgical sponges are manufactured with a radiopaque marker to aid identification; the markings typically appear as curved or banded radiopaque lines within the mass. However, sponges produced before radiopaque markers were commonplace, or gossypibomas that have masking calcium depositions, may not demonstrate a visible marker.7 These calcium depositions have been described as creating a calcified reticular rind sign on CT imaging.
The radiopaque markers in surgical sponges are composed of barium sulfate, which is neither magnetic nor paramagnetic. As a result, these markers do not produce an artifact on MRI. On T1-weighted imaging, gossypibomas most frequently appear as a well-circumscribed, low-signal mass, while on T2-weighted imaging they have high-signal intensity within the core and low-signal intensity on the periphery; the periphery typically contrast-enhances.8
Conclusion
Gossypiboma in the neck is rarely reported, with most cases occurring in the abdomen or pelvis. When presenting in the neck, differential diagnosis includes abscess and tracheocutaneous fistula. With its varied and nonspecific presentation, imaging plays a crucial role in diagnosis. Gossypiboma warrants diagnostic consideration in patients with a surgical history who demonstrate a well-circumscribed mass on imaging.
References
Citation
Wotherspoon T, Bailey K. Gossypiboma. Appl Radiol. 2024; (5):1 - 2.
doi:10.37549/AR-D-24-0036
October 1, 2024