Giant Breast Hamartoma
Images
Case Summary
An adult lactating patient presented with complaints of asymmetric enlargement of the left breast accompanied by occasional mild pain. The patient had delivered their first child four months prior and initially attributed the enlargement to lactation. The patient’s right breast was unremarkable, and they reported no history of fever, discharge, erythema, or nipple changes. The patient also reported no significant personal medical history and no family history of breast carcinoma. Clinical examination demonstrated a soft, freely moveable lump in the left breast. The axillary lymph nodes were not palpable bilaterally.
Imaging Findings
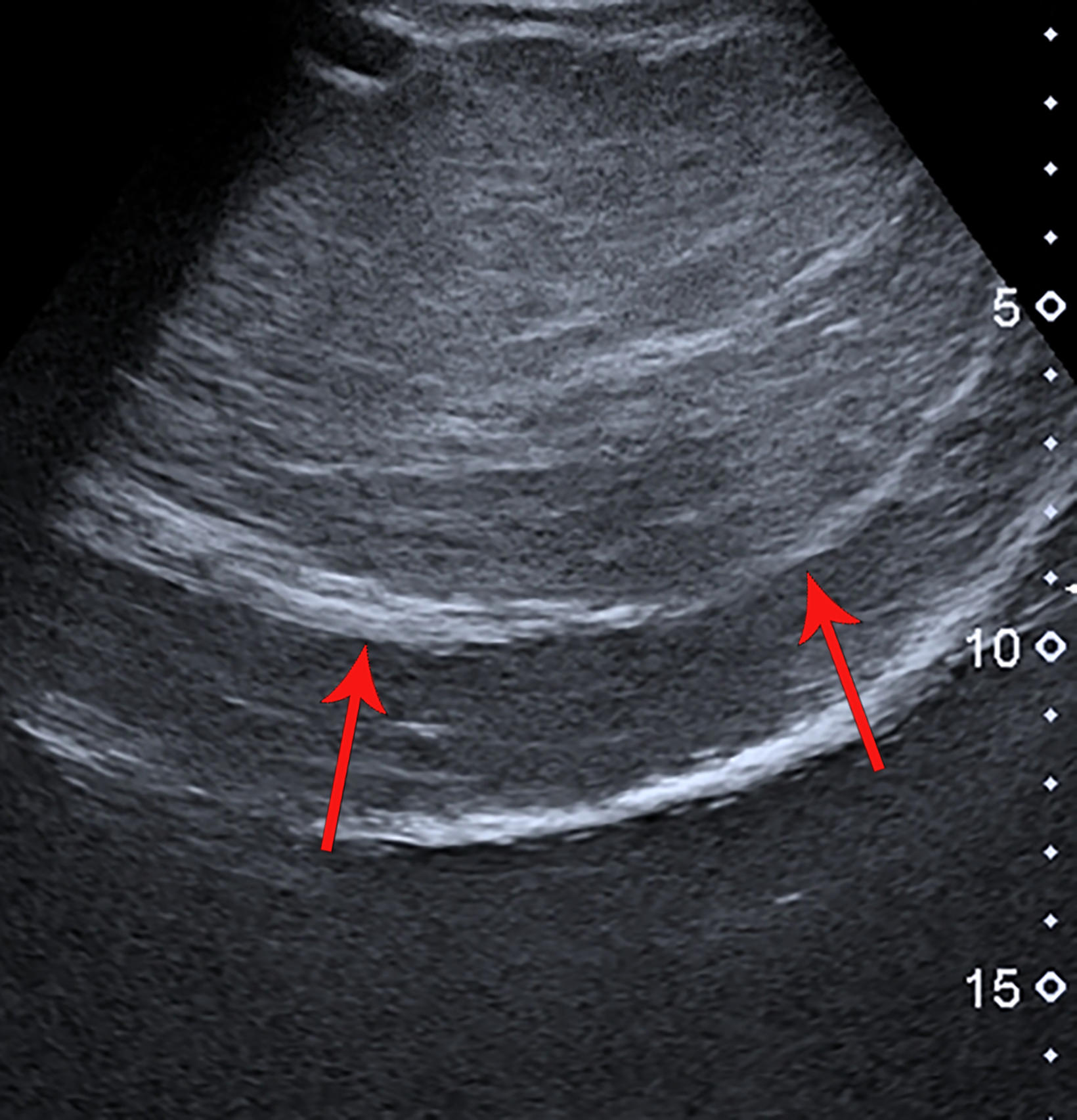
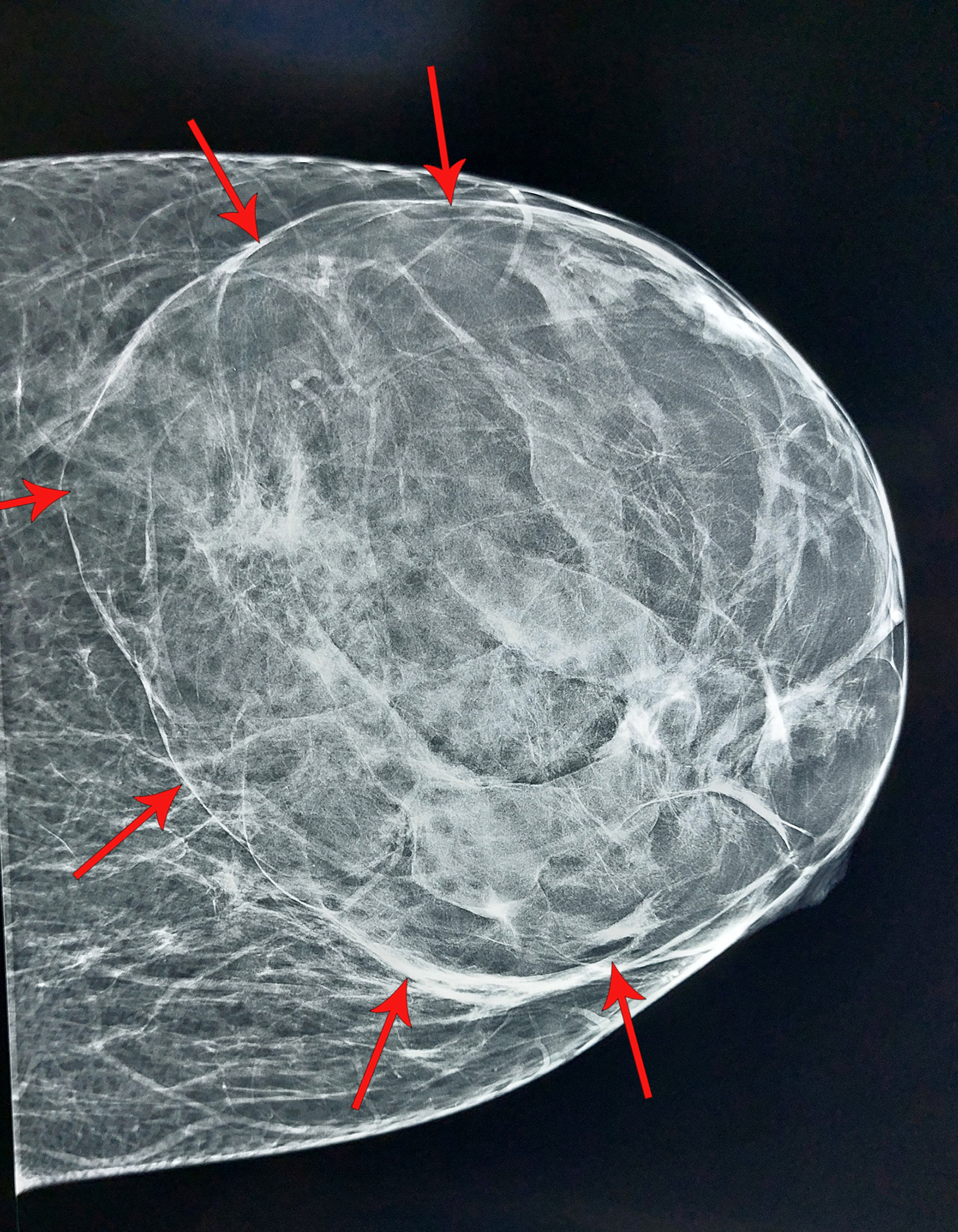
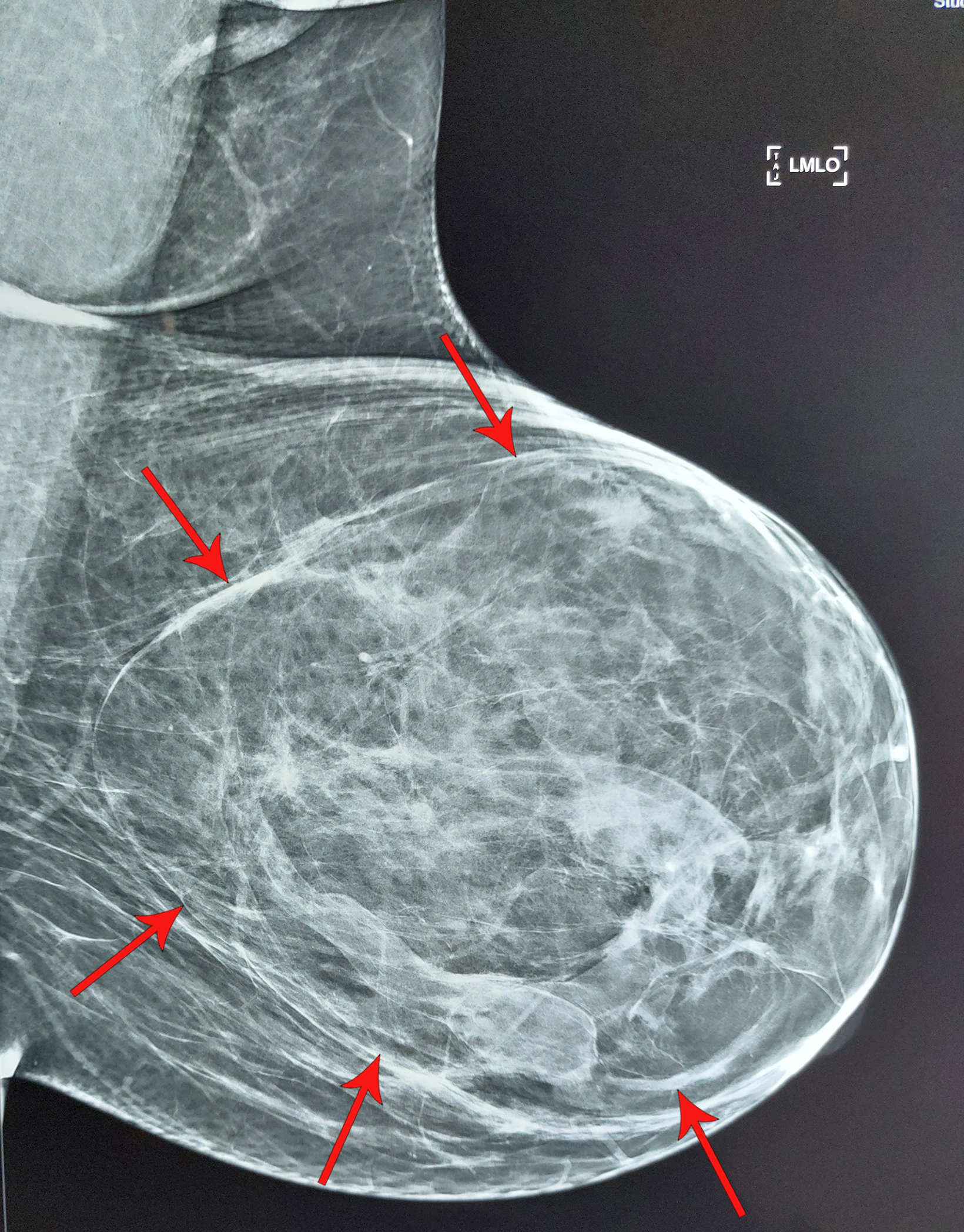
Ultrasound revealed an encapsulated iso- to hyperechoic, large lesion within the left breast parenchyma with a few, focally ectatic ducts showing internal moving echoes/inspissated secretions. No significant vascularity was present, nor were any calcific foci or posterior shadowing seen (Figure 1). Findings were suggestive of a benign etiology with hamartoma as the leading diagnostic con- sideration. A subsequent mammogram revealed a large, encapsulated lesion occupying almost the entire left breast. The lesion was of mixed density, with both fat and soft-tissue components, resulting in a “breast within a breast” appearance. No internal calcification was seen (Figure 2).
Diagnosis
Giant breast hamartoma
Discussion
Breast hamartomas are rare, benign, slow-growing lesions that account for 0.1 – 0.7% of benign breast lesions. First defined by Arrigoni et al in 1971,1 they are most frequently seen in women during perimenopause, but can also be found in men.2,3 Hamartomas consist of a mixture of tissues, including epithelial, fibrous, glandular, and adipose. Diagnosis can usually be made by combin- ing the clinical examination with radiological findings and histological features. Hamartomas are not considered premalignant lesions, but cases of invasive ductal carcinoma within a hamartoma have been reported.4
Hamartomas are well-encapsulated breast lesions that usually range from 2 to 5 cm in size but can grow larger. They usually present as a painless mass or asymmetrical enlargement of the breast without any palpable lump; they may, rarely, develop in the axillary region. Hamartomas are usually soft, mobile, painless lumps on physical examination and can be mistaken for other benign masses.5 Up to 60% are subclinical and missed on palpation.
Ultrasound features of hamartomas vary, owing to their variable amount of fibrous, adipose, and glandular tissue. They usually appear as round or oval, well-circumscribed and -encapsulated masses of inhomogeneous internal echotexture, and without any significant vascularity on Doppler examination. Retrotumor acoustic phenomena are absent, and a thin halo usually separates the lesion from the surrounding breast parenchyma.6
On mammography, hamartomas present as the classic “breast within a breast” appearance, with a thin, radiopaque pseudocapsule formed by surrounding, compressed breast tissue. Hamartomas rich in fibrous tissue appear homogeneously dense, mimicking a fibroadenoma, while hamartomas abundant in adipose tissue may be misdiagnosed as lipomas or fat necrosis. Calcifications are relatively rare.7
Magnetic resonance imaging is not routinely used to diagnose hamartoma. However, MRI might be performed in cases with atypical features on mammography and ultrasound. They usually exhibit type I time-signal intensity curve on postcontrast images.8
Hamartomas do not exhibit specific diagnostic histological features; therefore, the utility of fine needle aspiration cytology and needle core biopsy is limited. Combined clinical and radiological assessment is necessary to avoid misdiagnosis.9
The prognosis for a hamartoma is good with or without surgical excision, but excision is usually recommended, as associated malignancies have rarely been reported. The incidence of recurrence is 8%, and postoperative follow-up is recommended every six months for up to two years.10
Conclusion
Hamartomas are rare, benign breast lesions with a distinctive appearance on ultrasound and mammography. These entities are not considered premalignant, but because of the presence of glandular breast tissue, they may rarely undergo malignant changes similar to normal breast tissue.
References
Citation
S I. Giant Breast Hamartoma. Appl Radiol. 2023; (4):41-42.
June 23, 2023