Disseminated peritoneal leiomyomatosis



CASE SUMMARY
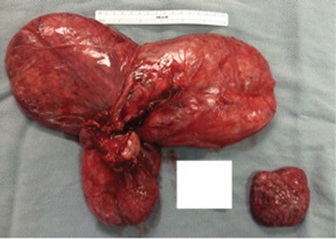
A 56-year-old female presented with abdominal/pelvic pain and fullness. Her history is significant for a large fibroid uterus treated with a hysterectomy and bilateral salpingo oophorectomy (BSO) approximately 10 years previous.
IMAGING FINDINGS
A noncontrast CT scan was ordered and revealed a large lobulated mass filling much of the pelvis and extending into the abdomen. Separate from the large mass were some smaller nodular masses that were initially thought to represent lymphadenopathy. No evidence of omental caking, hepatic metastasis, or ascites was demonstrated.
An MRI of the abdomen and pelvis was then performed with and without gadolinium that demonstrated a large, mildly enhancing, predominantly solid mass that fills the pelvis and extends into the lower abdomen. Other separate nodules were again noted and were initially interpreted incorrectly as lymphadenopathy. On T2-weighted imaging, the mass demonstrates decreased signal with a whorled appearance. No ascites or omental caking is present and there is no metastatic disease demonstrated in the liver or osseous structures.
DIAGNOSIS
Disseminated peritoneal leiomyomatosis
DISCUSSION
Disseminated peritoneal leiomyomatosis (DPL) is a benign rare entity characterized by the presence of innumerable smooth muscle nodules disseminated throughout the peritoneal cavity.1 Wilson and Peale first described DPL in 1952.2 This rare entity appears as multiple small nodules varying in size on or beneath the peritoneal surface, mimicking a malignancy but generally demonstrating benign histological features.1,2
It occurs more commonly in younger women with a history of uterine leiomyomas.1 Over 100 cases have been described, and although the pathogenesis is still controversial, there appears to be a relationship to hormonal factors including pregnancy, oral contraceptives, and rarely, granulosa cell tumors of the ovary.2,3. Laparoscopic myomectomy for treatment of uterine leiomyomas has also been implicated in the development of DPL due to dissemination of the tumor cells along the laparoscopic tract.4,5
While younger pre-menopausal female patients are most commonly associated with DPL, it has occurred rarely in both men and postmenopausal women where no excess of hormonal levels were identifiable. Rare cases of malignant transformation have also been reported.6-8
The most important entity in the differential diagnosis of disseminated peritoneal leiomyomatosis is peritoneal carcinomatosis, which typically manifests with metastatic disease, weight loss, ascites, and rapid progression of disease. Other differential possibilities include malignant peritoneal mesothelioma, and primary peritoneal serous carcinoma.9 The findings of darker fibrous appearing signal on T2-weighted MRI in a whorled pattern and the lack of ascites or omental caking favors DPL as the most likely diagnosis especially when a patient has a coexisting fibroid uterus or has undergone a hysterectomy for a leiomyomatous uterus.
CONCLUSION
While disseminated leiomyomatosis is a rare entity, it should be considered in a patient with a peritoneal mass or masses, especially if the patient has a coexisting fibroid uterus or has had a hysterectomy for a uterine leiomyoma. The peritoneal masses generally have a darker whorl-like appearance on T2-weighted MRI similar to other smooth muscle tumors and there isusually a lack of ascites and omental caking.
REFERENCES
- Tanaka YO, Tsunoda H, Sugano M. MR and CT findings of leiomyomatosis peritonealis disseminata with emphasis on assisted reproductive technology as a risk factor. Br J Radiol. 2009;82(975):e44-47.
- Willson JR, Peale AR. Multiple peritoneal leiomyomas associated with a granulosa-cell tumor of the ovary. Am J Obstet Gynecol. 1952;64(1):204-208.
- Tavassoli FA, Norris HJ. Peritoneal leiomyomatosis (leiomyomatosis peritonealis disseminata): a clinicopathological study of 20 cases with ultrastructural observations. Int J Gynecol Pathol. 1982;(1):59-74.
- Fasih N, Shanbhogue A, Macdonald DB, Fraser-Hill MA, et al. Leimyomas beyond the Uterus: Unusual Locations, Rare Manifestations. RadioGraphics. 2008;1931-1948.
- Kumar S, Sharma JB,Verma D, Gupta P, et al. Disseminated peritoneal leiomyomatosis: an unusual complication of laparoscopic myomectomy. Arch Gynecol Obstet. 2008;278(1):93-95.
- Fulcher AS, Szucs RA. Leiomyomatosis peritonealis disseminate complicated by sarcomatous transformation and ovarian torsion: presentation of two cases and review of the literature. Abdom Imaging. 1998;23:640-644.
- Lausen I, Jensen OJ, Andersen E, Lindahl F. Disseminated peritoneal leiomyomatosis with malignant change, in a male. Virchos Arch A Pathol Anat Histopathol. 1998,417:173-175.
- Yamaguchi T, Imaumra Y, Yamamoto T, Fukuda M: Leiomyomatosis peritonealis disseminate with malignant change in a man. Pathol Int. 2003;53:179-185.
- Levy AD, Arna’is J, Shaw JC, Sobin LH. Primary peritoneal tumors: imaging features with pathologic correlation. RadioGraphics. 2008;28:583-586.
Prepared by Mr. Josh Gottlieb while a fourth year medical student at New York Institute of Technology – College of Osteopathic Medicine, Old Westbury, Long Island, NY; and by Dr. Roy Gottlieb while serving as Medical Director at Rolling Oaks Radiology in Thousand Oaks, CA.
