Developing Breast Imaging Services in Low-Resource Settings
Images
As radiologists and radiology professionals, we find it hard to fathom healthcare without the critical medical imaging routinely utilized in the United States. In a typical breast imaging practice in a high-resource setting, the majority of cancers are diagnosed as stage 0 or stage I, with a 90% cure rate, having benefited from state-of-the-art tools for image-guided detection and diagnosis.1-4 In medically underserved regions, however, this is not the norm.
Breast cancer is the leading cause of cancer death for women worldwide, and its incidence continues to increase, particularly in low- and middle-income countries (LMICs).3
There is relatively higher mortality from breast cancer in LMICs compared to high-income countries (HICs), which may be due to differences in tumor biology, limited awareness about breast cancer on the part of patients or healthcare providers, and lack of access to screening, diagnostic, and treatment services.1,5-8 Without structured screening programs or easily accessible imaging and intervention, breast cancer in LMICs is more commonly diagnosed at a late stage (stage III or IV) compared to HICs.3 While early-stage breast cancer is largely curable with appropriate surgi- cal, oncologic, and radiation therapy, late-stage breast cancer has a much higher morbidity and mortality rate.4,9 Furthermore, late-stage breast cancer requires more advanced therapies, which are difficult to come by in the low-resource setting.
RAD-AID International is a non-profit organization that works to increase access to imaging services worldwide, with programs in 40 countries supporting 91 healthcare facilities. The Breast Imaging section of RAD-AID coordinates with local partners to improve access to breast care in LMICs as well as in medically underserved communities in HICs. The organization’s overarching strategy is to reduce breast cancer mortality in low-resource settings by downstaging disease through earlier detection. While its goals are to improve access to high-quality imaging and image-guided procedures, we recognize that early diagnosis is effective only if it is linked to early treatment. We collaborate with partner organizations and members that work across the continuum of care to ensure that women with cancer have access to treatment and post-treatment surveillance. To achieve earlier detection for larger populations, RAD-AID also supports community outreach, navigation, and patient education.
The RAD-AID Approach
RAD-AID consistently adheres to a set of guiding principles. First, we always partner with a local healthcare institution or organization that has identified breast cancer care as a priority. We rely on our partner’s knowledge of local culture and local healthcare resources, their relationships with other potential local, regional, and national stakeholders, and their enthusiasm for program building.
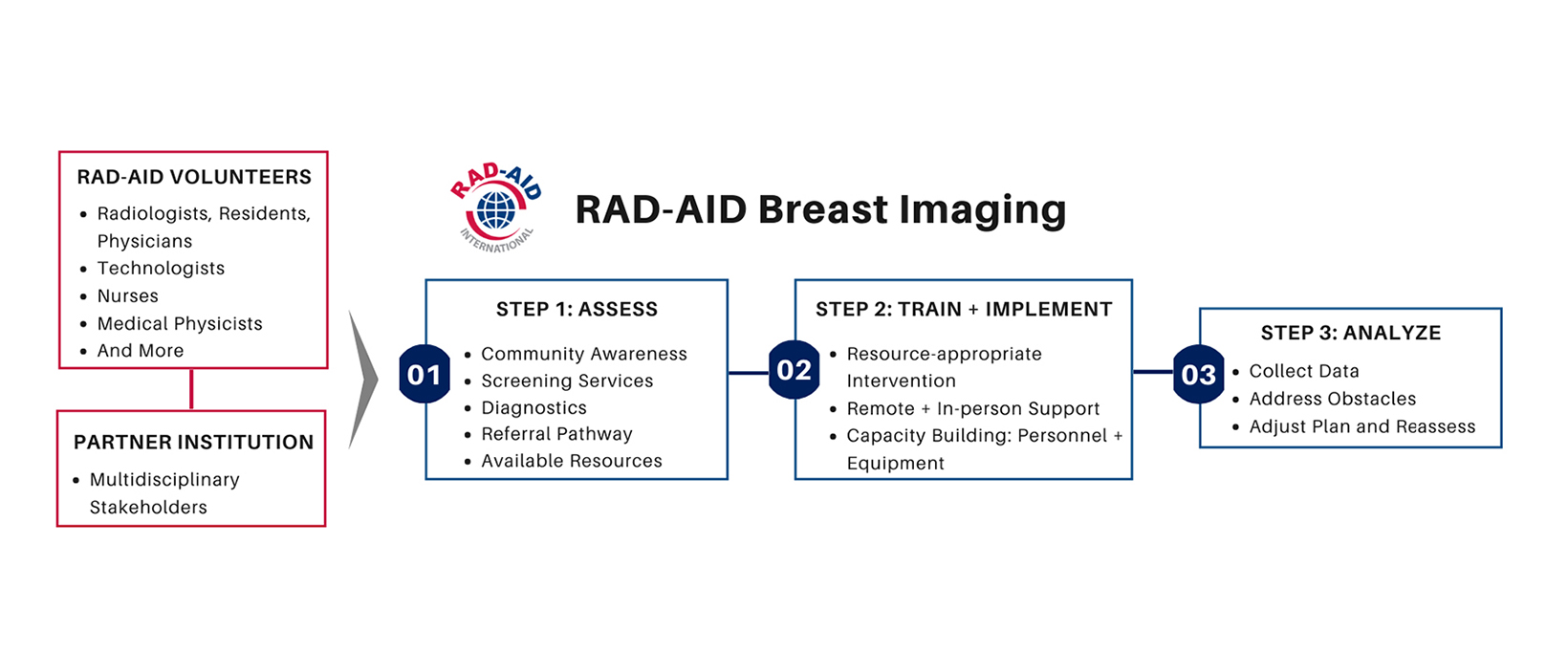
Once we identify a partner, we follow a systematic approach to assessment, planning, implementation, and program evaluation to develop and carry out an intervention that is uniquely tailored to the needs of our partners and the local healthcare landscape (Figure 1).10,11 Evidence has shown that it is absolutely critical to only pursue resource-appropriate interventions. The Breast Health Global Initiative (BHGI) and the National Comprehensive Cancer Network (NCCN) have published comprehensive guidelines suggesting how resources should be allocated toward various
aspects of breast cancer care depending on resource availability.12,13 We also adhere to a phased implementation approach to build capacity gradually without overwhelming our partners.14 Our first step of program planning, therefore, is always a thorough assessment of our target population and the local availability of screening, diagnostic services (imaging, tissue sampling, and pathology) and treatment.
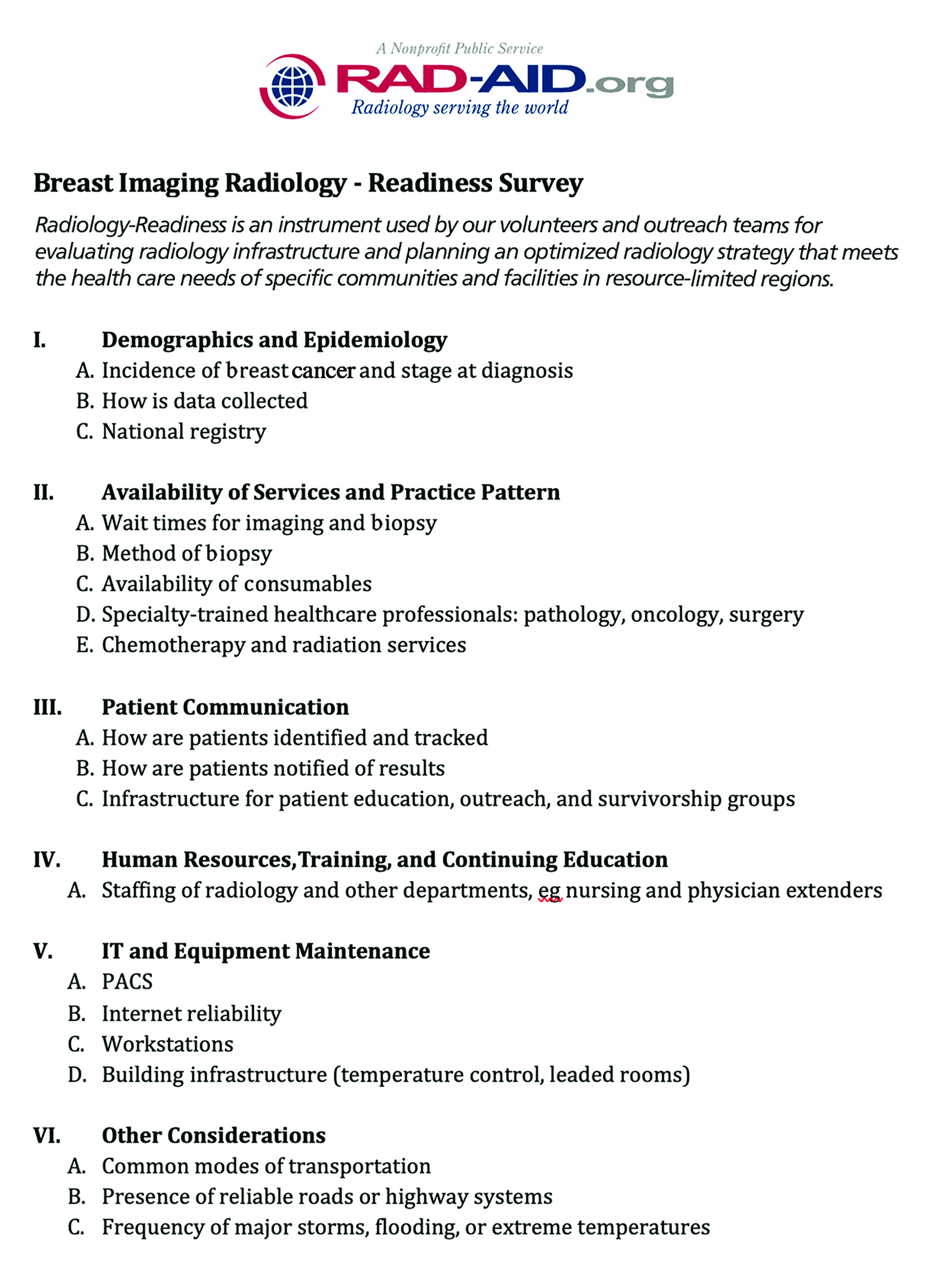
Radiology-Readiness™ is RAD-AID’s data collection and analysis tool, which launched in 2009. The tool received review and input and from the World Health Organization (WHO) in 2012 and has been the cornerstone of RAD-AID’s official relations status with WHO since 2015. The Radiology-Readiness Assessment (RRA) collects detailed information about local healthcare assets, capabilities and radiology services at the specific prospective partner institution in order to optimize allocation of resources for high-yield clinical objectives. RAD-AID Breast Imaging has developed a breast imaging-specific RRA to collect information about available resources related to the entire spectrum of the breast health referral pathway (Figure 2). The Breast Imaging RRA allows us to identify gaps in any service that may affect a patient’s cancer care, including clinical breast exams, imaging, pathology, surgery, radiation and oncologic care, and surveillance during survivorship.
When devising a strategy, we take advantage of the breadth of expertise within the RAD-AID leadership and volunteer pool to create teams of nurses, physicians, and technologists, as well as experts in quality assurance, business leadership, informatics, medical physics, and public health. Finally, we plan with an eye toward sustainability to ensure our interventions lead to lasting improvement. While we maintain long-term relationships with our partners, our goal is that the benefits of our partnerships persist even after we have stepped away from directly supporting the site. We aim to build capacity to create meaningful impacts in healthcare.
Reaching Out Through Education, Collaboration
Education and training are a major focus. We mentor institutions to develop breast imaging leaders so that those individuals may go on to increase breast cancer services locally and nationally. Our education model incorporates a holistic approach that focuses on the full continuum of care for breast health, including primary and secondary prevention, screening methods, treatment modalities, and palliative care. Our interdisciplinary teams have led combined didactic and hands-on skills training workshops to teach interventional techniques to physicians, positioning techniques to mammographers, and clinical breast exam techniques to nurses and primary healthcare workers in Ghana, Kenya, Tanzania, Ethiopia, India, Bangladesh, Peru, and Guyana.
During the COVID-19 pandemic, we adapted to restricted travel conditions by shifting to remote teaching and leveraging an online-learning management platform of prerecorded lectures, live webinars, and ongoing regular virtual classrooms with read-out sessions of recent cases. For sites where RAD-AID has donated Picture Archiving and Communication Systems (PACS) — Guyana, Nigeria, and Laos, for example — image-sharing for case consultations and real-time clinical teaching have also been implemented.
To augment breast care resources in LMICs, supporting in-country training programs for radiologists who need specialized breast imaging education is vital. RAD-AID is helping to create breast imaging fellowships in Ethiopia, Kenya, and Ghana. Such fellowships require longitudinal relationships through multiple stages of education program planning, including curriculum development and approval, faculty and trainee recruitment, program implementation, and collection of competency metrics.
In LMICs and HICs, breast imaging outreach can be flexibly implemented to suit local contexts via mobile or fixed-site small clinics, tertiary care institutions, or a combination thereof. RAD-AID is supporting care models across these contexts, including mobile mammography in India, Morocco, and the United States; camp clinics in India, Jordan, Kenya, and the United States; a primary care clinic in Peru; and tertiary care sites in Ethiopia, Ghana, Guyana, Indonesia, and Kenya.
While mammography is the mainstay of breast imaging in high-resource regions with large-scale screening programs, it is not a feasible option everywhere. We have found that breast ultrasound is often more easily implemented in early detection programs. For example, in Cusco, Peru, our assessment identified breast health for indigent women as a critical gap in the local healthcare landscape. In partnership with Cervicusco, a non-profit organization that provides cervical cancer services, and the Instituto Nacional de Enfermedades Neoplásicas (INEN, the National Cancer Hospital of Peru), we have taught breast ultrasound to healthcare providers already skilled at performing body ultrasound with an efficient, systematic approach.15,16 In keeping with the BHGI and NCCN guidelines, we focus on ultrasound as a diagnostic tool in these regions. There is also evidence that ultrasound may be a useful screening tool in areas where mammography is unfeasible.17
In the United States, RAD-AID launched a longitudinal collaboration with the Black Women’s Health Imperative (BWHI), National Alliance of Hispanic Health, and Hologic Inc.’s Project Health Equality to bring awareness to and address long-standing healthcare disparities that affect women of color.18 In this initiative, we collaborate with and support primary care centers that are already serving medically underserved women of color as well as tertiary centers interested in improving access to specialty care for women who need it most.
Our partner sites are primarily Federally Qualified Health Centers (FQHCs), primary care providers partially funded by the federal government for the purpose of reducing health inequities.19 Creating access to screening at the point of primary care is one successful strategy implemented by our FQHC partners.20 The approach at each institution is tailored to best meet the needs of the specific target population. Despite the varied tactics, patient navigation and strengthening of the referral pathway are critical components to address the social determinants of health.21,22
Artificial Intelligence Initiatives
We have implemented breast radiology artificial intelligence (AI) tools that provide real-time educational feedback for physicians and technologists. The RAD-AID AI model, called Teach-Try-Use, integrates education, infrastructure, and gradual implementations of AI to locally validate and support AI in low-resource health institutions.23 This effort has been supported by several pro-bono contributions of breast imaging AI software integrated with RAD-AID’s educational initiatives, such as Koios and Densitas. The coupling of AI with radiology education for breast health outreach has been particularly valuable while in-person education had been halted during the pandemic.24
The Koios Decision Support for Breast system uses machine learning to improve accuracy of breast lesion assessment on ultrasound.25 We expect this tool to help general radiologists and non-radiology providers in Guyana, Kenya, and Peru triage breast ultrasound cases so that suspicious lesions are diagnosed quickly and valuable resources are not wasted on typically benign lesions. Densitas® qualityAI™ uses machine learning to provide mammography technologists with real-time feedback on positioning and other critical quality control metrics.26 This has been implemented in Guyana, where mammography is a relatively newly available modality, and continuing education for mammography technologists is not easily available, particularly during the pandemic.
In our preliminary pilot of breast imaging AI using Densitas in Guyana, seven mammography technologists received AI-based quality feedback on over 380 radiology exams. This resulted in approximately 20-point improvements in posterior breast tissue inclusion in screening exams over a ten-week period from October to December 2020. High-quality mammograms are critical for accurate interpretation and early detection of breast cancer. Since the success of any AI tool in a specific setting depends on the applicability of the database from which its algorithms are trained, we anticipate that implementation of AI in the low-resource setting will lead to continued development of AI tools that are able to serve patients everywhere.24,27
Future Directions and Goals
As the pandemic continues in 2022 — placing disproportionate burden on healthcare systems in low-resource settings — we will continue to focus on remote education and support. We aim to develop and expand our breast health curriculum to include the important role of patient navigation.
In the United States, we plan to scale our model of care to other sites and engage policy makers to change healthcare delivery to poor communities. On a larger scale, we plan to carefully move forward with responsible implementation of AI tools that can increase efficiency and capacity, including diligent ongoing analysis and monitoring to ensure that it is able to serve the needs of diverse populations.
We hope that in time we are able to effect change that brings needed resources to breast cancer care globally with a focus on early detection. To that end, the RAD-AID Breast Imaging team eagerly welcomes new volunteers with expertise in any aspect of breast cancer care who are interested in promoting high-quality care to underserved patients.
Participation can include donating educational materials, leading live, web-based workshops, rendering over-read opinions on day-to-day cases, working with our physics and quality teams to ensure appropriate standards, trouble-shooting equipment issues via web videoconferencing, or collaborating with our informatics team to coordinate PACS and AI implementation.
We seek partnerships with creative and enthusiastic healthcare providers dedicated to improving the health of women worldwide.
References
- WHO. https://seer.cancer.gov/statfacts/html/breast.html. Accessed January 5, 2022.
- Duggan C, Trapani D, Ilbawi AM, et al. National health system characteristics, breast cancer stage at diagnosis, and breast cancer mortality: a population-based analysis. 2021;22(11):1632-1642.
- World Health O. WHO report on cancer: setting priorities, investing wisely and providing care for all. Geneva: World Health Organization; 2020.
- DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69(6):438-451.
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249.
- DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2015;24(10):1495-1506.
- Ginsburg O, Bray F, Coleman MP, et al. The global burden of women’s cancers: a grand challenge in global health. The Lancet. 2017;389(10071):847-860.
- Galukande M, Kiguli-Malwadde E. Rethinking breast cancer screening strategies in resource-limited settings. Afr Health Sci. 2010;10(1):89-92.
- Society. AC. Cancer Facts & Figures 2021. In: Society AC, ed. Atlanta, GA2021.
- RAD-AID International. https://rad-aid.org/resource-center/radiology-readiness. Accessed January 5, 2022.
- Mollura DJ, Azene EM, Starikovsky A, et al. White Paper Report of the RAD-AID Conference on International Radiology for Developing Countries: identifying challenges, opportunities, and strategies for imaging services in the developing world. J Am Coll Radiol. 2010;7(7):495-500.
- Yip CH, Smith RA, Anderson BO, et al. Guideline implementation for breast healthcare in low- and middle-income countries: early detection resource allocation. Cancer. 2008;113(8 Suppl):2244-2256.
- Jazieh AR, McClure JS, Carlson RW. Implementation Framework for NCCN Guidelines. J Natl Compr Canc Netw. 2017;15(10):1180-1185.
- Ginsburg O, Yip CH, Brooks A, et al. Breast cancer early detection: A phased approach to implementation. Cancer. 2020;126 Suppl 10(Suppl 10):2379-2393.
- Aklilu S, Bain C, Bansil P, et al. Evaluation of diagnostic ultrasound use in a breast cancer detection strategy in Northern Peru. PLoS One. 2021;16(6):e0252902.
- González Moreno IM, Trejo-Falcón J, Matsumoto MM, et al. Radiology volunteers to support a breast cancer screening program in Peru: description of the project, preliminary results, and impressions. Radiologia (Engl Ed). 2021.
- Sood R, Rositch AF, Shakoor D, et al. Ultrasound for breast cancer detection globally: A systematic review and meta-analysis. J Glob Oncol. 2019;5:1-17.
- Hologic. https://www.hologic.com/ProjectHealthEquality Accessed January 31, 2022.
- Health Center Program: Impact and Growth. Health Resources & Services Administration. Published 2021. Updated August 2021. Accessed February 2, 2022.
- Kim CS, Vanture S, Cho M, Klapperich CM, Wang C, Huang FW. Awareness, interest, and preferences of primary care providers in using point-of-care cancer screening technology. PLOS ONE. 2016;11(1):e0145215.
- Brown J, Kaufman RE, Ariail M, Williams DL. Assessing patient navigation as a tool to address equity in cancer early detection. Transl Cancer Res. 2019:S421-S430.
- Roland KB, Milliken EL, Rohan EA, et al. Use of community health workers and patient navigators to improve canceroOutcomes among patients served by federally qualified health centers: a systematic literature review. Health Equity. 2017;1(1):61-76.
- International R-A. RAD-AID Artificial Intelligence. In:2021.
- Mollura DJ, Culp MP, Pollack E, et al. Artificial intelligence in low- and middle-income countries: innovating global health radiology. Radiology. 2020;297(3):513-520.
- Mango VL, Sun M, Wynn RT, Ha R. Should we ignore, follow, or biopsy? Impact of artificial intelligence decision support on breast ultrasound lesion assessment. AJR Am J Roentgenol. 2020;214(6):1445-1452.
- Densitas. The Opportunity to Improve Mammography Quality with Automated, Machine Learning Software. In: Densitas Inc.; 2018.
- Alami H, Rivard L, Lehoux P, et al. Artificial intelligence in health care: laying the foundation for responsible, sustainable, and inclusive innovation in low- and middle-income countries. Globalization and Health. 2020;16(1):52.
References
Citation
EB P, G A, P D. Developing Breast Imaging Services in Low-Resource Settings. Appl Radiol. 2022;(2):28-32.
March 4, 2022