CT-FFR Informs Need for Invasive Artery Treatment
Images
A new study shows that coronary CT angiography (CTA) fractional flow reserve (FFR) can help identify patients with coronary artery blockage or narrowing who need a revascularization procedure. The findings were published as a Special Report in Radiology: Cardiothoracic Imaging.
Doctors use CTA to diagnose narrowed or blocked arteries in the heart. A CTA exam receives a score from mild (0‑1) to moderate (2‑3) to severe (4‑5). Patients with scores above 3 typically require medical treatments and can potentially benefit from stents or surgeries (revascularization) to restore blood flow to the heart.
“CTA tells you the degree to which a vessel is blocked,” said Mangun Kaur Randhawa, MD, a post-doctoral research fellow in the Department of Radiology at Massachusetts General Hospital (MGH) in Boston. “But the degree of blockage doesn't always reliably predict the amount of blood flow in the vessel.”
Doctors have traditionally relied on an invasive procedure known as invasive coronary angiography to image vessels and more recently have added other invasive tests like FFR to identify and assess significant blockages in the vessels.
CT-FFR is a relatively new alternative that non-invasively models a patient’s coronary blood flow using CTA images of the heart, AI algorithms and/or computational fluid dynamics.
To assess the impact of the selective use of CT-FFR on clinical outcomes, Dr. Randhawa’s research team conducted a retrospective study of patients who underwent coronary CTA at MGH between August 2020 and August 2021.
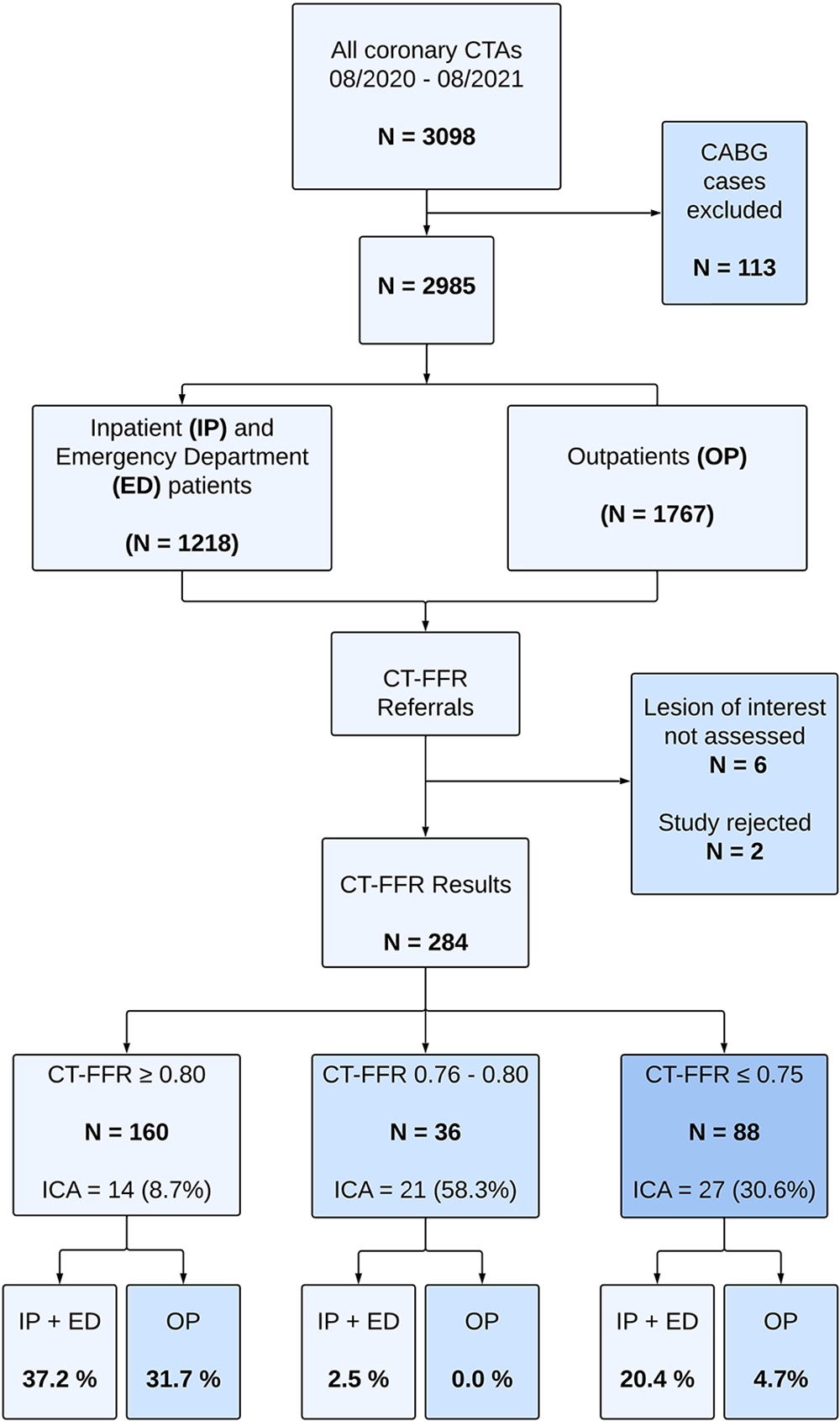
During the study period, 3,098 patients underwent coronary CTA. Of these, 113 coronary bypass grafting patients were excluded. Of the remaining 2,985 patients, 292 (9.7%) were referred for CT-FFR analysis, and eight of these exams were excluded, leaving a final study group of 284.
As expected, most referrals to CT-FFR were patients with scores of 3 or above. CT-FFR was requested in the majority (73.5 %) of patients with a score of 3 (moderate
narrowing/blockage).
“In patients with moderate narrowing or blockage of the arteries, there can be ambiguity about who would benefit from invasive testing and revascularization procedures,” Dr. Randhawa said. “CT-FFR helps us identify and select those patients who are most likely to benefit.”
Out of the 284 patients, 160 (56.3%) had a negative CT-FFR result of > 0.80, 88 patients (30.9%) had a clearly positive (abnormal) result of ≤ 0.75, and the remaining 36 patients (12.6%) had a borderline result between 0.76-0.80.
Patients with significant narrowing/blockages on coronary CTA who underwent CT-FFR had lower rates of invasive coronary angiography (25.5% vs. 74.5%) and subsequent percutaneous coronary intervention (21.1% vs. 78.9%) than patients who were not referred for a CT-FFR.
“CT-FFR helps us identify patients who would most benefit from undergoing invasive procedures and to defer stenting or surgical treatment in patients who likely won’t,” said senior author Brian B. Ghoshhajra, MD, MBA, associate chair for operations and academic chief of cardiovascular imaging at MGH. “CT-FFR makes the CT ‘better’, but we found that the benefits were highest when used selectively.”
Dr. Ghoshhajra added that their CT-FFR analysis was successful in the large majority of patients, regardless of challenging factors such as elevated or irregular heart rates and obesity.
“When you objectively measure coronary artery flow with CT-FFR, you induce fewer patients to be further investigated and treated, because you tend to treat not just what the eyeball sees, but what the physiology supports,” he said.
The researchers said the study results demonstrate the utility of CT-FFR in clinical practice, when used selectively, highlighting its potential to reduce the frequency of invasive procedures in patients with significant coronary artery narrowing or blockages without compromising safety.