Coronary arteriovenous fistula
Images
CASE SUMMARY
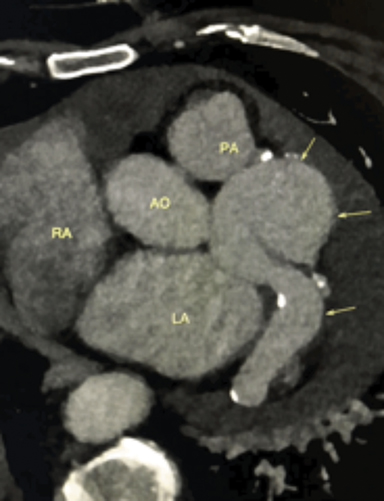
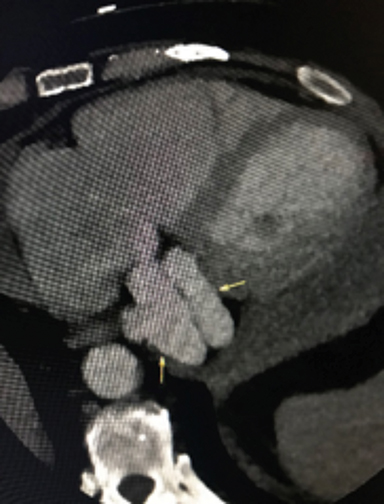
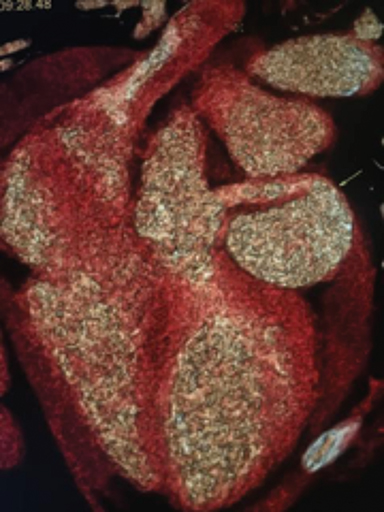
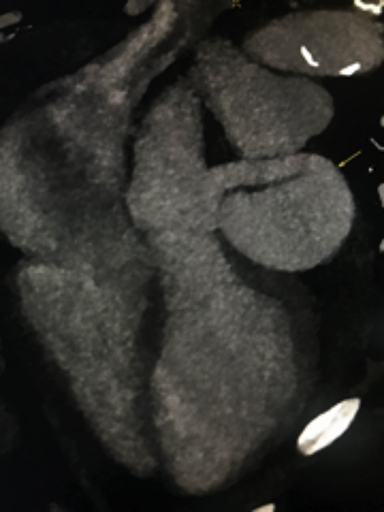
A 65-year-old man with symptomatic atrial flutter was being evaluated for an elective catheter ablation. Preoperative transesophageal echocardiogram (TEE) revealed incidental abnormal cardiac anatomy with aneurysmal dilation of coronary vessels. A cardiac CT angio gram (CCTA) was ordered for further evaluation. The CCTA was acquired with ECG gated retrospective in a 256 slice iCT (Philips) following IV 60 cc of Omnipaque 370 at 5.0 cc/sec. injection. Images reconstructed multiplanar and cMPR at 8mm thickness using iterative model reconstruction (IMR).
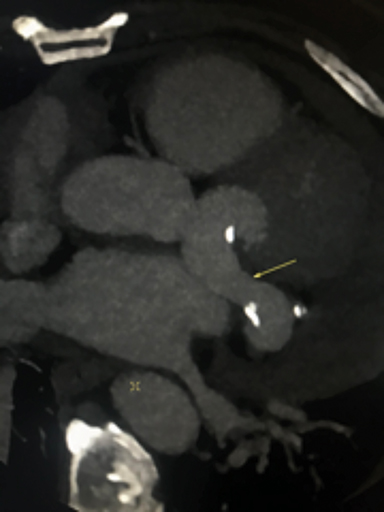
IMAGING FINDINGS
The CCTA demonstrates a large fistula between the proximal left anterior descending coronary artery (LAD) (Figure 1) and great cardiac vein (GCV). The left main coronary artery, LAD and GCV are aneurysmal secondary to the fistula. The markedly dilated GCV drains in to the coronary sinus (Figure 2) and contains multiple atherosclerotic spotty calcifications secondary to chronic systemic arterial pressure (venous arterialization). The left ventricular ejection fraction was calculated at 40%. There was visualized global left ventricular hypokinesis. Patient was referred for surgical consultation and fistula closure.
DIAGNOSIS
Coronary arteriovenous fistula
DISCUSSION
Congenital coronary arteriovenous fistula (CAVF) is a rare anomaly present in 0.002% of the general population, which are often found incidentally during angiographic evaluation.1 CAVF may also be acquired.
Most fistulas are of single origin and arise from the right coronary artery (RCA) or the LAD; left circumflex coronary artery is rarely involved. 90% of the fistulas drain into venous circulation, including right-sided chambers (40%), pulmonary artery (15-20%), coronary sinus (7%) and superior vena cava (1%).1,2 Cardiac catheterization with coronary angiography has been used as the main diagnostic test for CAVF.3 More recently, CCTA has demonstrated to be an excellent, noninvasive diagnostic alternative test for evaluation of congenital cardiac vascular anomalies in adults.4 Most fistulas are small and found incidentally during various imaging studies, requiring additional imaging with CCTA, transthoracic echocardiogram, magnetic resonance imaging or cardiac catheterization to show the presence of concomitant atherosclerosis and other structural anomalies.3,5
Subclinical symptoms are common in the first two decades of life. The most common presenting symptoms include exertional dyspnea or fatigue, angina pectoris and occasionally complications of congestive heart failure, myocardial infarction, pericardial or pleural effusions, cardiac arrhythmias, thrombosis and rupture of dilated aneurysmal coronary arteries.3 The management of coronary fistulas must be individualized based on cardiovascular symptoms, concomitant cardiovascular comorbidities, the size and anatomical location of the CAVF.3 Large fistulas despite symptoms and small-to moderate size fistulas with evidence of arrhythmia, myocardial ischemia, ventricular enlargement or dysfunction should undergo percutaneous or surgical closure based on American College of Cardiology/American Heart Association class 1 guidelines.6-7 Regardless of prior surgical or percutaneous interventions, CAVF draining into the coronary sinus result in a particularly high risk of long-term morbidity.8-9 It is noteworthy that major complications such as coronary thrombosis, myocardial infarction, and cardiomyopathy may occur after closure of CAVF with an incidence of 15%.8
CONCLUSION
Congenital CAVF is a rare cardiac vascular anomaly. Large fistulas, as in this case, are commonly incidentally found during workup of cardiovascular symptoms and complications secondary to the anomaly. Early surgical intervention of CAVF by surgery or transcatheter closure is indicated due to high prevalence of symptoms and fistula related complications.2-3
References
- Zamani H, Meragi M, Arabi Moghadam MY, Alizadeh B, Babazadeh K, Mokhtari-Esbuie F. Clinical presentation of coronary arteriovenous fistula according to age and anatomic orientation. Caspian Journal of Internal Medicine. 2015;6(2):108-112.
- Ata Y, Turk T, Bicer M, Yalcin M, Ata F, Yavuz S. Coronary arteriovenous fistulas in the adults: natural history and management strategies. Journal of Cardiothoracic Surgery. 2009;4:62. doi:10.1186/1749-8090-4-62.
- Albeyoglu S, Aldag M, Ciloglu U, et al. Coronary Arteriovenous Fistulas in Adult Patients: Surgical Management and Outcomes. Brazilian Journal of Cardiovascular Surgery. 2017;32(1):15-21. doi:10.21470/1678-9741-2017-0005.
- Ghadri, J.R., Kazakauskaite, E., Braunschweig, S. et al. BMC Cardiovasc Disord. 2014; 14: 81. https://doi.org/10.1186/1471-2261-14-81.
- Gowda RM, Vasavada BC, Khan IA. Coronary artery fistulas clinical and therapeutic considerations. Int J Cardiol. 2006;107(1):7–10.
- Challoumas D, Pericleous A, Dimitrakaki IA, Danelatos C, Dimitrakakis G. Coronary Arteriovenous Fistulas: A Review. The International Journal of Angiology: Official Publication of the International College of Angiology, Inc. 2014;23(1):1-10. doi:10.1055/s-0033-1349162.
- Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults with Congenital Heart Disease). Developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52(23):e143–263.
- Valente AM, Lock JE, Gauvreau K, Rodriguez-Huertas E, Joyce C, Armsby L, et al. Predictors of long-term adverse outcomes in patients with congenital coronary artery fistulas. Circ Cardiovasc Interv. 2010;3(2):134–139.
- Kiefer TL, Crowley AL, Jaggers J, Harrison JK. Coronary Arteriovenous Fistulas: The Complexity of Coronary Artery-to-Coronary Sinus Connections. Texas Heart Institute Journal. 2012;39(2):218-222.
Citation
A S, C S, M L, J L, V F,. Coronary arteriovenous fistula . Appl Radiol. 2019;(2):46-47.
March 28, 2019