CMS Appropriate Use Criteria for Cardiac Imaging Creates Reimbursement Confusion
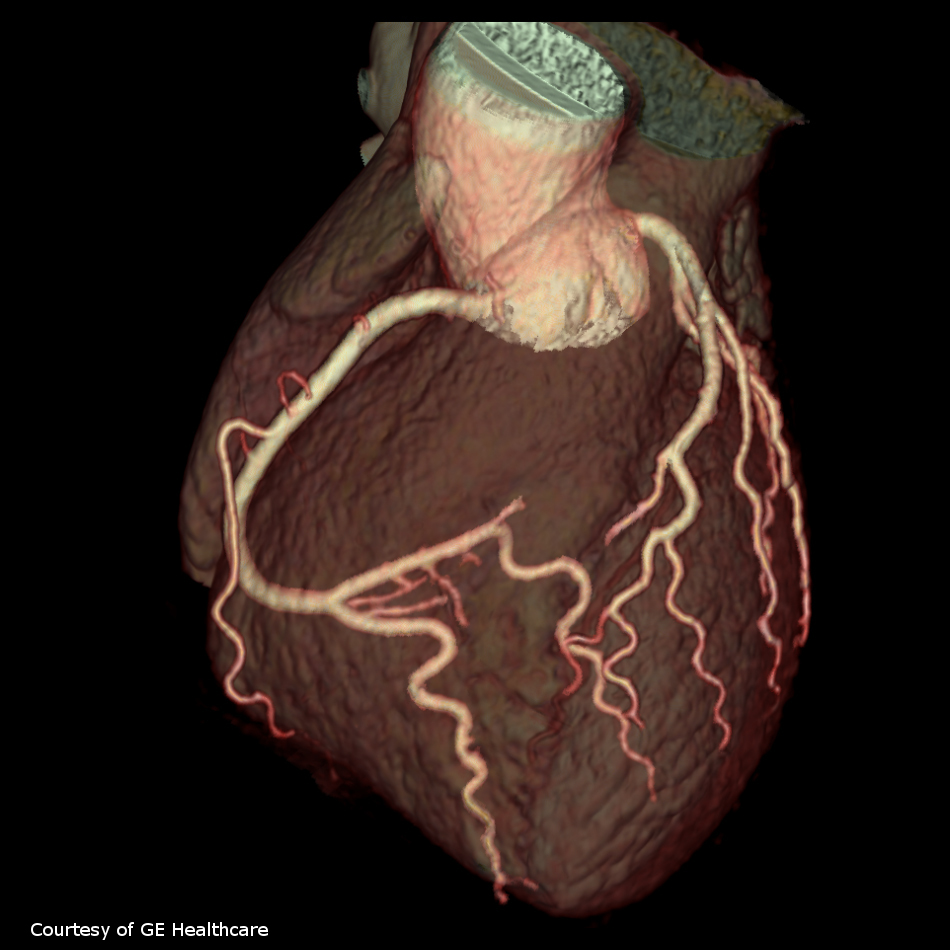
Images
A paper reviewing the Appropriate Use Criteria (AUC) program has found that the limited, currently available criteria for coronary artery disease (CAD) imaging are inconsistent and unclear, potentially leaving clinicians and patients uncertain about whether the care clinicians are delivering will be reimbursed by the Centers for Medicare and Medicaid Services (CMS). The analysis is published in Annals of Internal Medicine.
Congress established the AUC Program to reduce unnecessary advanced imaging studies. The program further stipulates that the AUC used by clinical decision support mechanisms must be developed by CMS-qualified organizations composed of practitioners providing direct patient care, so-called provider-led entities (PLEs). However, some questions remain about the development of AUC and adherence to the requirements outlined in the AUC program.
Researchers from several institutions reviewed website for the authorized PLE’s and found that only a minority have developed AUC related to CAD, one of the identified “priority clinical areas”. The AUC that have been developed for CAD are substantially heterogeneous the methods used and the structure and content of their AUC recommendations. They add that the current patchwork of AUC from different PLEs allows for conflicting assessment of appropriateness that may leave frontline clinicians uncertain about whether the care they are delivering will ultimately be reimbursed by CMS. The authors offer possible modifications to the current program, including: restricting CMS approval of PLEs to medical societies, academic institutions, or organizations with an established track record of producing AUC published in peer-reviewed scientific journals; approving narrower AUCs for a single priority clinical area; or requiring all PLEs for a priority clinical area to work collaboratively on creating a single unified AUC.