CMS Adjusts Nuclear Medicine Reimbursement Policy
Images
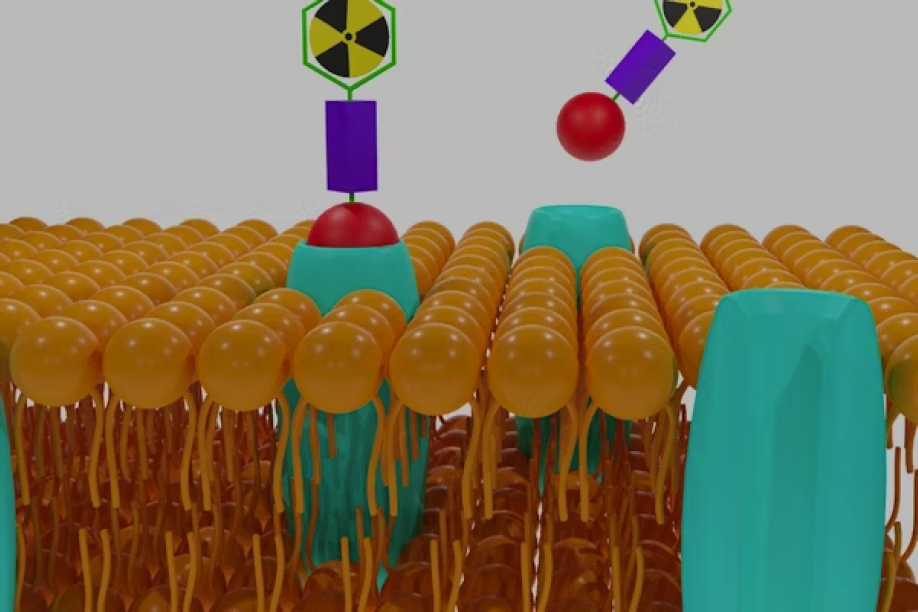
The Centers for Medicare & Medicaid Services (CMS) announced a significant adjustment to the Hospital Outpatient Prospective Payment System (HOPPS) for nuclear medicine reimbursement. Under the new policy, CMS will unpackage and pay separately for diagnostic radiopharmaceuticals with per-day costs exceeding $630, removing financial barriers that have long hindered patient access to essential nuclear medicine diagnostic procedures.
“This decision is a critical victory for patients who need advanced diagnostic care,” said SNMMI President Cathy Sue Cutler, PhD. “We commend CMS for this significant move to improve access to life-saving nuclear medicine scans, ensuring that patients across the country can receive the best possible care.”
Nuclear medicine imaging, including cutting-edge PET and other nuclear medicine scans, is often the most accurate and cost-effective way to diagnose complex diseases, providing critical insights that can inform and shape patient treatment. However, under the previous reimbursement system, diagnostic radiopharmaceuticals were bundled as “supplies,” limiting access in several ways:
- Patients frequently lacked access to nuclear medicine scans that could alter their course of treatment, due to cost barriers.
- Physicians were less likely to administer these procedures due to inadequate reimbursement.
- Hospitals sometimes were forced to discontinue certain nuclear medicine procedures, as Medicare reimbursement did not cover the full cost of these high-value drugs (radiopharmaceuticals).
- Pharmaceutical companies struggle to sustain production of innovative nuclear medicine radiopharmaceuticals due to insufficient reimbursement.
Recognizing the urgent need for change, SNMMI has advocated tirelessly for a more equitable reimbursement structure. In August 2024, SNMMI submitted formal comments to CMS supporting separate payment for diagnostic radiopharmaceuticals at both the $630 and $550 thresholds. The revised policy, which takes effect on January 1, 2025, will now unbundle radiopharmaceuticals costing above $630, helping to ensure these life-changing diagnostic tools remain accessible to patients.
The policy update marks the culmination of SNMMI’s persistent efforts over the past 16 years, which included submitting numerous letters to CMS, coordinating meetings with congressional representatives, organizing grassroots advocacy efforts, organizing Hill Days, and issuing repeated calls to action. This success also effectively removes the need for legislative action under the FIND Act, for which SNMMI members and supporters had strongly advocated in recent years.
“This win is truly a community achievement,” said Cutler. “We are deeply grateful to SNMMI members, patients, healthcare providers, and community advocates who joined us in supporting this important cause. Your voices made a difference.” SNMMI offers special thanks to its partner organizations for their vital support.
SNMMI will continue to work closely with CMS to refine and enhance the reimbursement models, ensuring sustained and equitable access to advanced diagnostic care for all patients.
A webinar will be held for the community about the impact of the decision on coding and reimbursement; stay tuned for details. For more information on this policy change and SNMMI’s ongoing initiatives, please visit SNMMI's official website.