Challenges of Workflow Optimization in Mammography
Introduction to Breast Imaging Workflow
Over the last few decades, radiology workflow has changed significantly, fundamentally altering the day-to-day workload of radiologists. With the advent of the picture archiving and communication system (PACS) and transition to digital imaging, most changes have improved efficiency of the average radiologist.1, 2 Despite this, many technical and practical challenges remain when interpreting radiology studies beyond the complexity of the case. Therefore, attempts to improve daily workflow remain, especially in breast imaging.
Workflow Differences Between Diagnostic and Screening Examinations
The process of completing a diagnostic breast examination is a complicated act, with multiple participants and moving parts. This is a phased examination involving many steps, where the images are obtained, the radiologist is consulted for their interpretation, and recommendations for further imaging or follow-up are made, all in the same visit. Similar steps are taken at most institutions for a complete diagnostic examination, illustrated in Figure 1 .
Steps involved in completing a diagnostic mammogram
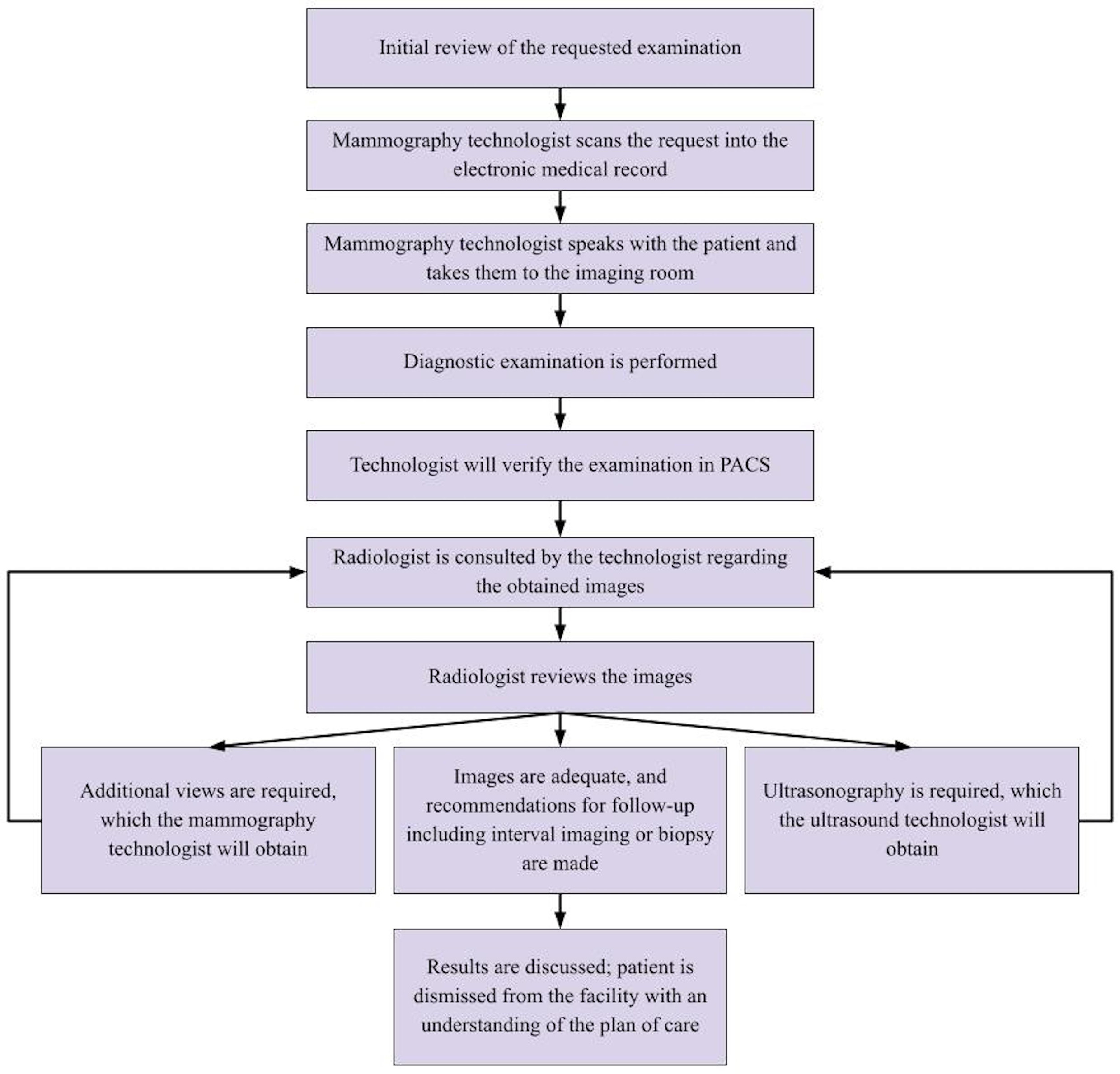
This process allows for examination results to be communicated to the patient prior to discharge from the facility. To facilitate the prompt interpretation of diagnostic studies, coordination between the radiologist and the technologist must be precise, which is difficult in real-life practice. If an issue arises in the steps above, workflow will be disrupted and examination outcome delayed.
In comparison, screening examinations do not require as much immediate oversight. By definition, if further imaging is required, a Breast Imaging-Reporting and Data System (BI-RADS) score of 0 can be assigned and the patient can be brought back for additional imaging. Therefore, screening mammograms are triaged as the least urgent examination in breast imaging, with priority given to diagnostic studies and procedures. As a result, it is not uncommon to see screening mammograms from the prior week on a worklist, especially in busy centers. The Mammography Quality Standards Act (MQSA), which is the federal standard of care, allows for 30 days when reporting the results of screening studies.
Despite this, patients undergoing screening mammography have shown a preference for obtaining results within 48 hours or even waiting at the breast imaging center for their results.3 Additionally, if the results of screening mammograms are communicated on the same day, in a similar fashion to diagnostic studies, nearly half of the patients would be more satisfied with their cancer screening experience.4 Obtaining results within a short period reduces anxiety and improves compliance with future annual screening studies.5
How Do We Optimize Breast Imaging Workflow?
Efforts to maximize workflow when reading from the breast imaging list have been underway, many of which apply to all imaging modalities and subspecialties; these are known as global workflow changes. Most initiatives specific to breast imaging apply to screening mammograms, which make up the bulk of studies interpreted at our breast center, although some also extend to diagnostic examinations.
Global Workflow Changes
Single PACS . Imaging studies from outside institutions, including those performed at satellite facilities, are shown on a single list. This minimizes interruption from logging into multiple PACS in a day.
Prior studies . Prior relevant studies are automatically pulled by the system for comparison, reducing the time a radiologist spends searching for prior studies individually. However, it is worth noting that errors can occur when PACS automatically retrieves prior studies.
Universal templates . Many of our radiologists use a universal template for reporting a wide variety of imaging studies. Those utilized by our breast radiologists include the information required per BI-RADS standards, with autofilled fields for the date, type of study, reason for examination, individual and familial risk factors, available comparison studies, technique, findings that include a description of the breast composition (eg, “The breasts are extremely dense, which lowers sensitivity of mammography”), impression, BI-RADS assessment category, and follow-up recommendation. The use of universal templates bolsters reporting efficiency, while simplifying and improving consistency of results for requestors and patients.
Workflow Changes Specific to Mammography
Cancer risk assessment models . The use of a cancer risk assessment model is included in the report and the patient’s electronic medical record (EMR) for the radiologist to review. At our institution, the Gail model is used as it is one of the earliest prediction tools of its kind and has been used by radiologists to stratify individual patient risk. Modified versions of the Gail model have been released since its inception, with changes made to improve its application to non-white patients. The model remains insensitive to patients with BRCA mutations and a personal history of cancer.
Trainee-specific improvements . Radiology residents and fellows can mark which studies on the PACS they have dictated, thus alerting the attending physician to not initiate a report on the same study. This step prevents confusion since the attending physicians and trainees read from the same list. Reviewing cases with the trainee can occur in batches after a certain number of cases have been sent to the attending radiologist. For example, depending on the trainees’s level of training, an attending physician may opt to review 10 cases at a time with a trainee, minimizing interruptions while focusing educational efforts.
Artificial intelligence . The use of artificial intelligence (AI) detection software for interpreting mammograms has been an ongoing effort. Computer-aided detection (CAD) can help radiologists detect abnormalities in mammography. However, this technology is still relatively new, and its ability to contribute consistently is questionable. CAD has been shown to demonstrate a high false-positive rate.6
Many of these initiatives are used at other institutions successfully, improving efficiency when reading mammograms. In one study, similar workflow changes were made: the worklist was consolidated, trainees had cases assigned to them, and efforts were made to improve paperwork upload time. The study found a significant reduction in the average time spent on each study and report turnaround time.1
Obstacles in Optimizing Mammography Workflow
The biggest hurdle in the breast imaging workflow involves the real-time radiologist review of diagnostic examinations. This is more striking given the relative complexity of completing a diagnostic mammogram, as compared with a screening study. Issues can arise at any of the steps outlined in Figure 1 , preventing the successful review and dictation of the diagnostic examination. Therefore, any changes made to streamline diagnostic workflow will benefit the radiologist, technologist, and patient.
At our institution, we have made new efforts to reduce workflow interruptions by using the EMR to communicate when diagnostic examinations require review. Using the EMR, the technologist sends a message to the radiologist, including the name of the patient and the reason for the examination, at which point the radiologist reviews the images and provides recommendations. The goal of this initiative is to reduce in-person interruptions, exemplifying an ongoing attempt to optimize workflow wherever possible, although its effectiveness has yet to be definitively proven.
Improvements in dictation efficiency of screening studies have also been pursued. For example, institutions have implemented the use of AI triage software to establish efficient screening mammogram worklists.7 Examinations given high AI scores for cancer detection are placed in an enhanced assessment stream where they receive a more prompt evaluation by the radiologist. The ultimate goals of such an initiative is to convert a positive screening study to a diagnostic study in real time or potentially reduce the need for a radiologist review of studies considered negative by AI; in this study, AI did not miss cancer in women with the lowest 60% of scores.7 However, currently, all mammograms require review by radiologists, given the developing nature of this technology and possible medicolegal implications of using this type of algorithm.
From the patient’s perspective, another potential area for improvement involves the timing between the diagnostic examination and biopsy. Despite the significant stress and importance related to these procedures, clearly defined MQSA standards are lacking regarding the timeliness of breast biopsy.8 Ideally, the diagnostic examination and biopsy would be performed on the same day. However, currently, the average time from diagnostic imaging to biopsy is approximately 7 days, although these wait times have significantly decreased over the past 15 years.9
The Future of Breast Imaging Workflow
The last few decades have demonstrated steady improvements in the daily workflow among breast imaging technologists and radiologists, which have enhanced patient care, timeliness, and availability of examination results. Future advances involving the use of the EMR and AI software integration, for example, will continue to boost overall satisfaction of the patient—and the radiologist.
References
Citation
AM S, CZ T. Challenges of Workflow Optimization in Mammography. Appl Radiol. 2024;(4):16 - 19.
doi:10.37549/AR-D-24-0025
August 1, 2024