Brain Abscess
Images
Case Summary
An adolescent presented with a seizure after a 1-week history of progressively worsening headache and left-sided neuropathy. The patient had sinusitis treated with antibiotics about 10 days prior to presentation but was otherwise healthy. On exam, the patient was afebrile and normotensive. Lateral nystagmus was present. Laboratory studies demonstrated moderate leukocytosis (13,400 /mm3) with a left shift and normal blood cultures.
Imaging Findings
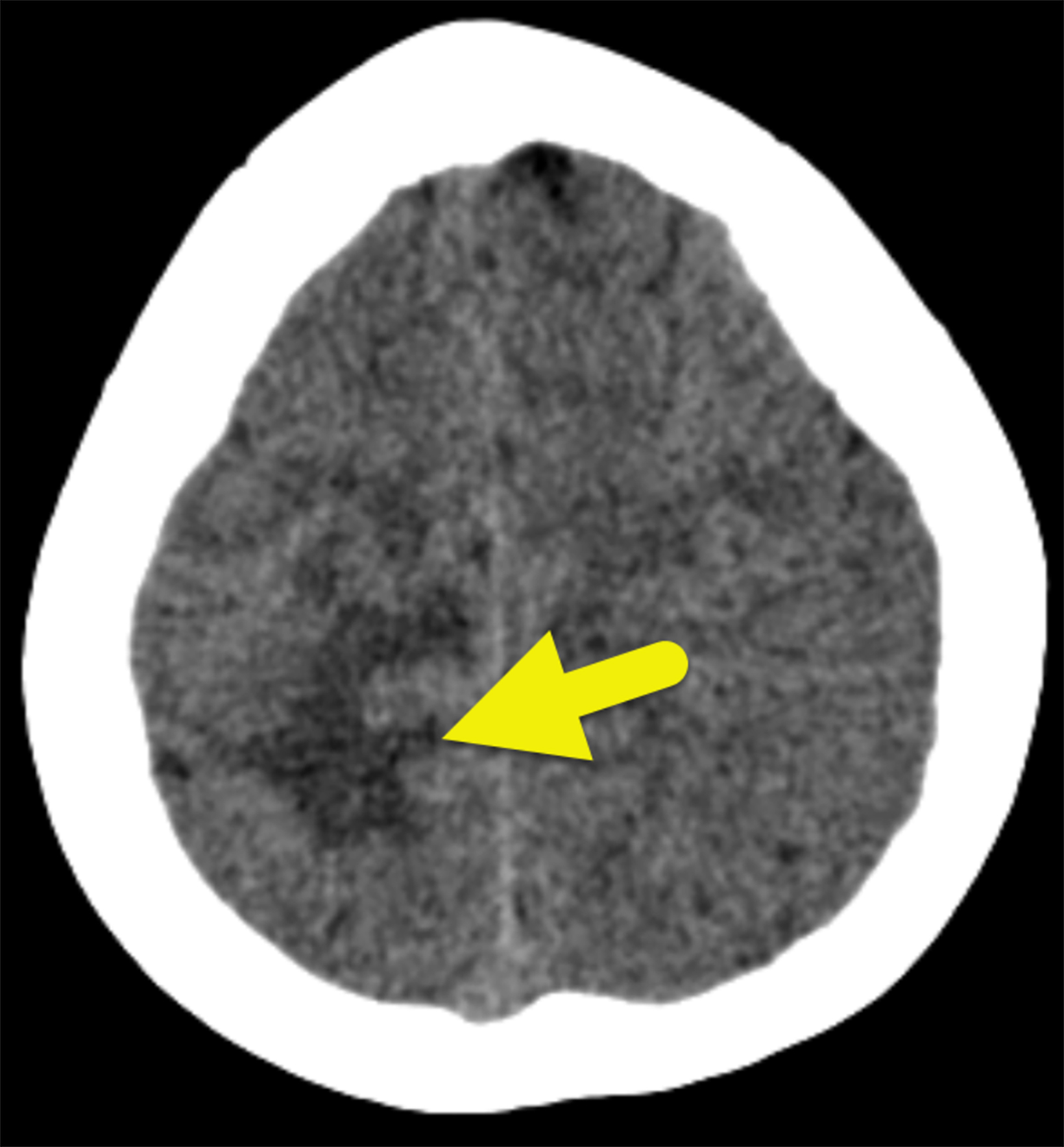
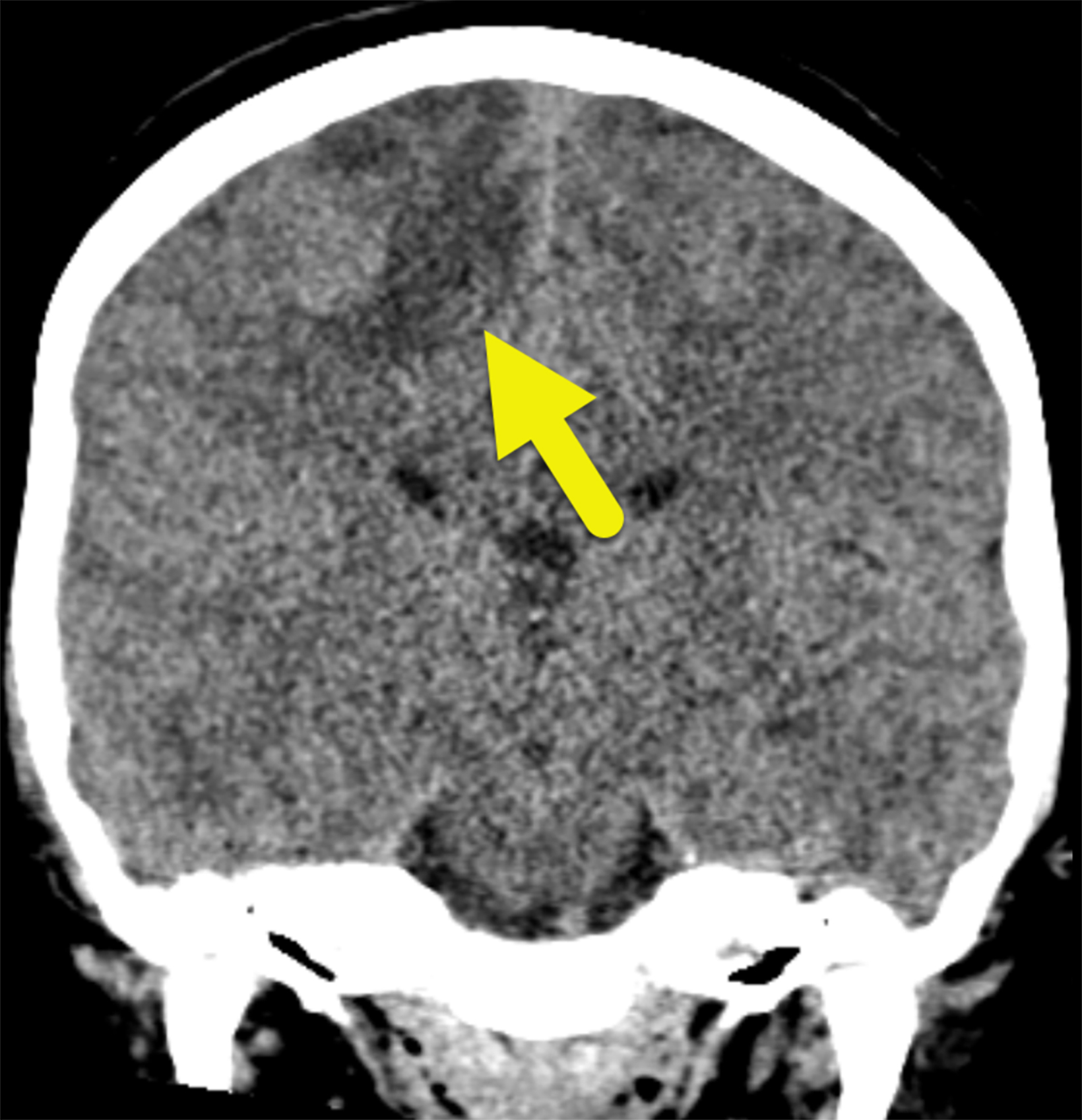
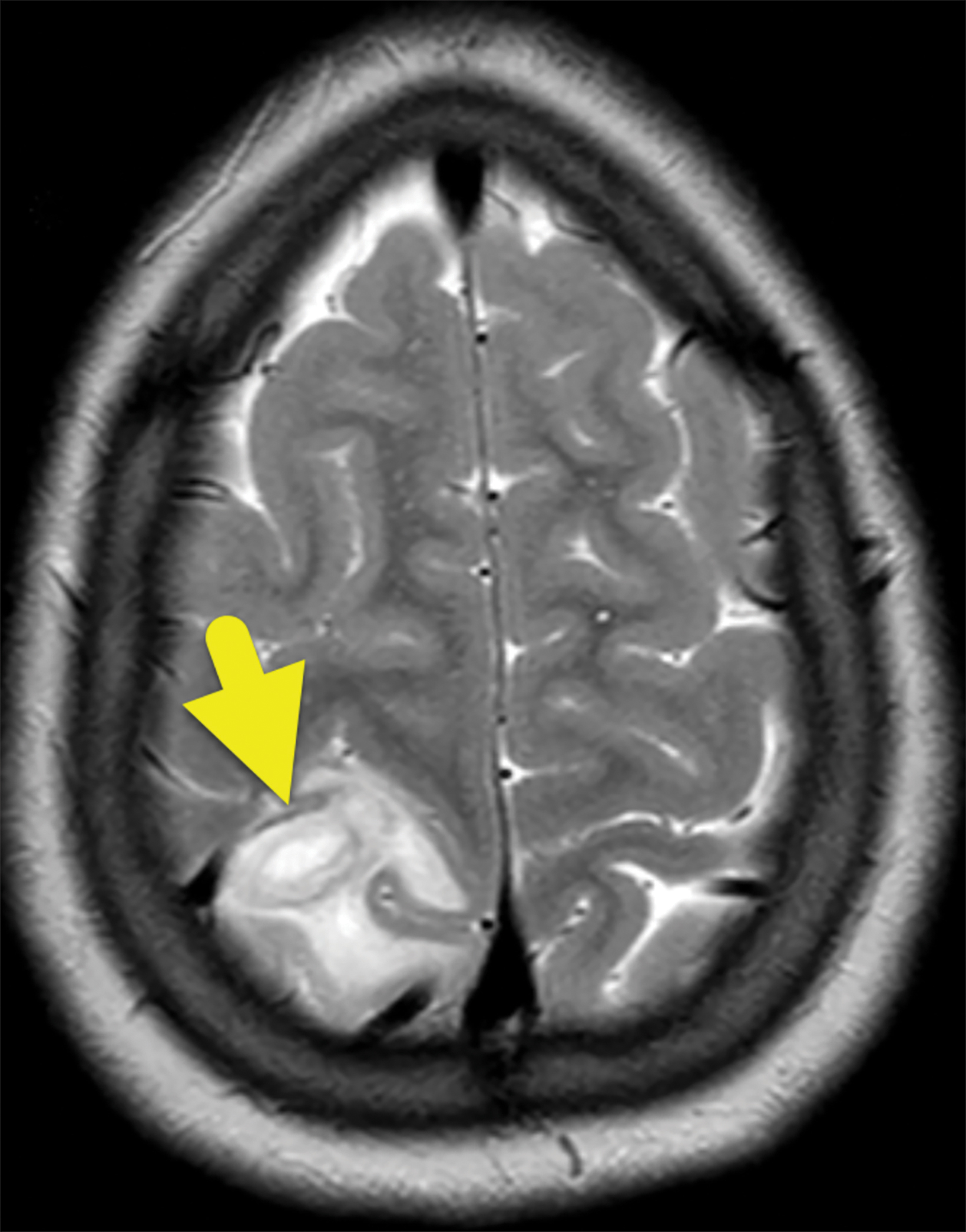
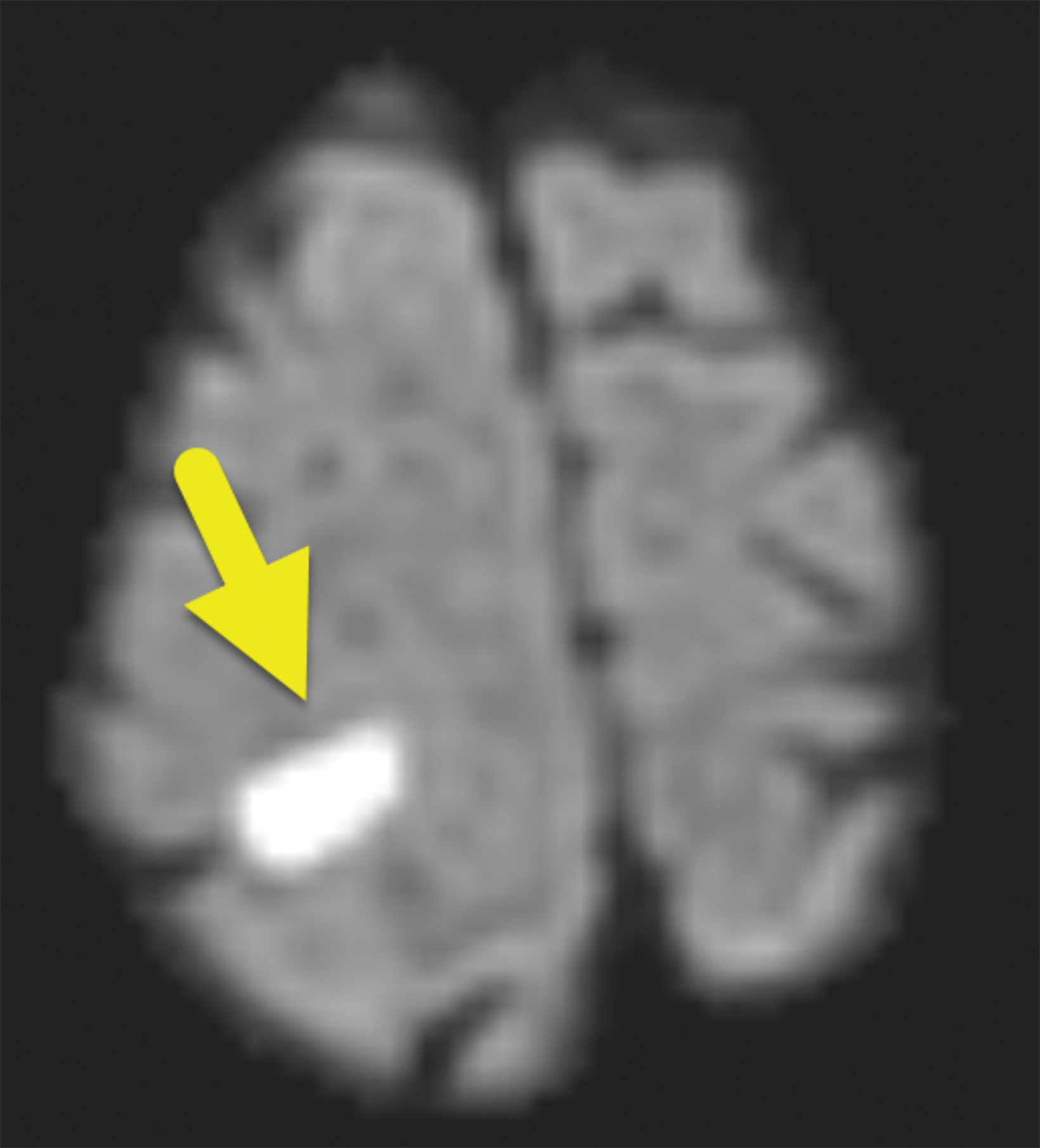
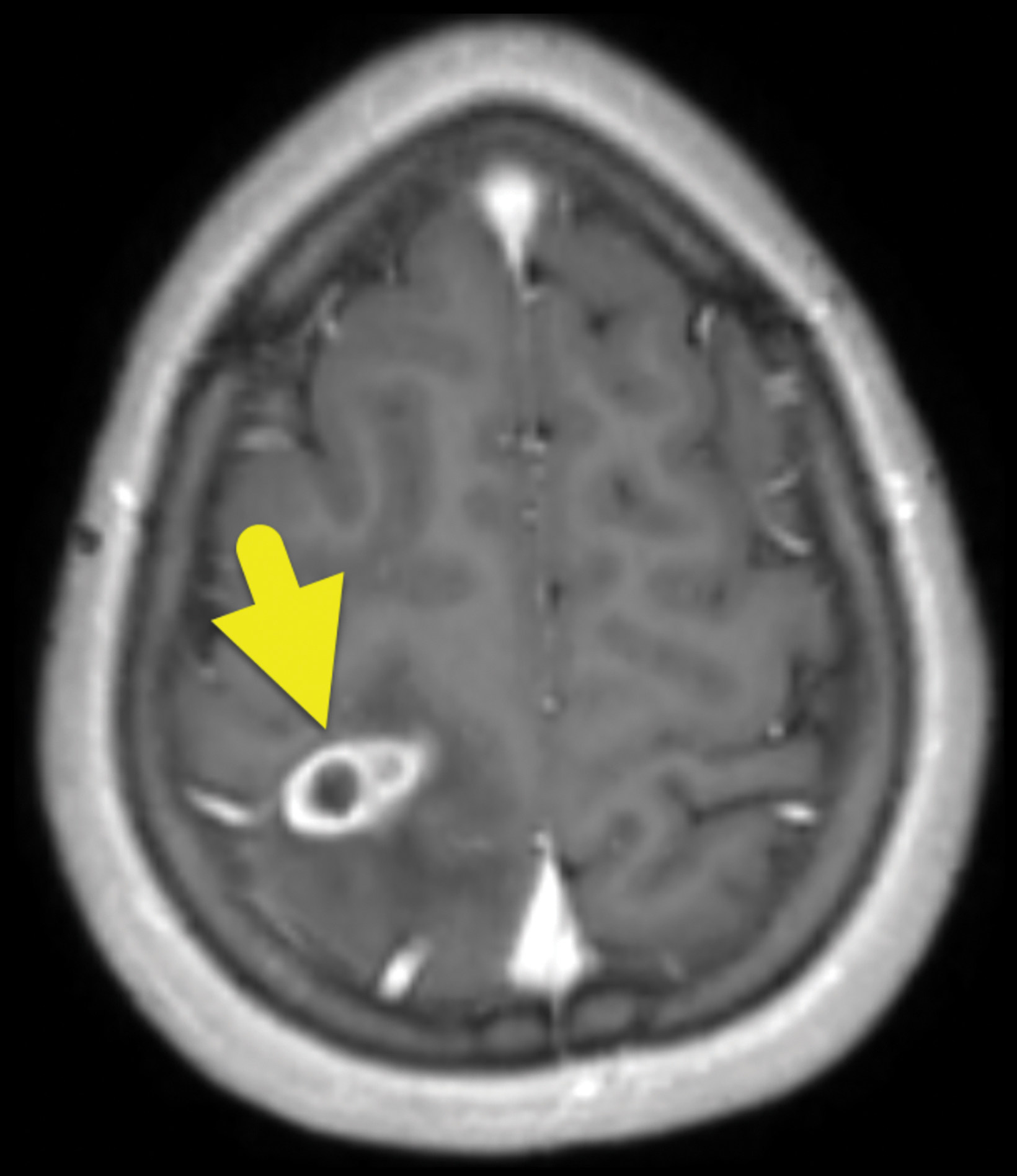
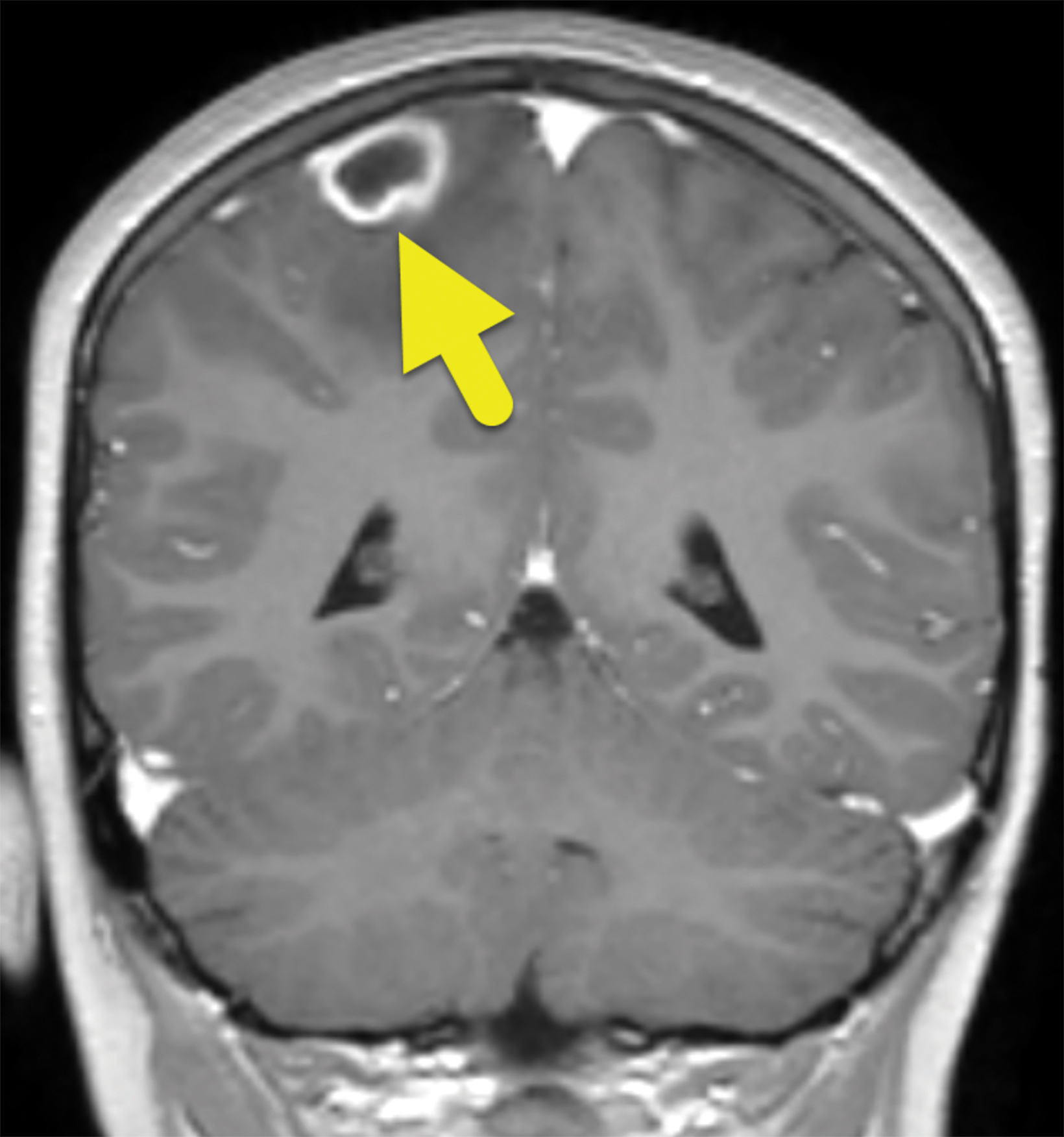
Noncontrast brain computed tomography (CT) showed a right posterior frontal-parietal mass with perilesional vasogenic edema (Figure 1). The mass involved gray and white matter and exerted local mass effect with compression of the local sulci but no midline shift. Magnetic resonance imaging (MRI, Figure 2) the following day demonstrated a 1.3 × 2.4 × 1.7 cm lesion that was centrally hypointense on T1 with a T1 isointense rim and surrounding T1 hypo- and T2-hyperintense white matter signal, the latter representing vasogenic edema. On T2 and FLAIR sequences there was central hyperintensity with a relatively hypointense rim. Restricted diffusion was present centrally. After injection of contrast, there was a ring enhancement and no enhancement centrally.
Right parietal craniotomy was performed for drainage and washout of the abscess. Intraoperative cultures grew Streptococcus intermedius.
Diagnosis
Brain abscess involving the right parietal lobe caused by Streptococcus intermedius.
The differential diagnosis of a ring-enhancing brain lesion is broad and includes a variety of infections (bacterial, tuberculoma, neurocysticercosis); primary (lymphoma, high grade glioma) and metastatic brain tumors; demyelinating conditions; and radiation necrosis. DR MAGIC serves as a pneumonic for the differential diagnoses of supratentorial ring enhancing brain lesions: D=Demyelinating disease, R=Radiation necrosis, M=Metastases, A=Abscess, G=Glioblastoma and other tumors, I=Infarction, C=Contusion.
Discussion
Brain abscesses are rare in children, occurring with an incidence of 0.3 to 1.3 per 100,000.1,2 They most commonly occur via direct spread of infection from sinusitis or mastoiditis. However, they can also result from hematogenous spread of infection. In patients with hematogenous spread, endocarditis or a congenital right-to-left cardiac shunt should be considered.
The presentation of a brain abscess depends on the patient’s age and the affected brain region. The classic clinical triad of fever, headache, and neurological deficit is present in only 20% of cases, but a brain abscess should be considered in a child with new-onset acute headache or first-time seizure, especially in the setting of an associated focal neurologic sign, fever, and elevated white blood cell count.
Patients with a brain infection can present at any stage of abscess evolution. Within 3 days after a cerebral infection begins, cerebritis is primarily characterized by an inflammatory response. On MRI, cerebritis begins with poorly defined increased T2 signal and absence of contrast enhancement.3 Late cerebritis, which presents from the 4th to the 9th day of infection, can show central necrosis and peripheral angiogenesis; the former seen as central T1 hypointensity and T2 hyperintensity while the latter appears as peripheral contrast enhancement. The center may become isointense on delayed imaging.3 The transition of cerebritis to abscess involves the progression of bacterial invasion of the brain parenchyma with liquefaction/necrosis of the involved brain tissue until surrounded by a capsule that indicates maturing abscess capsule formation.4 Thin ring enhancement occurs in the early abscess stage, which typically ranges from day 10 to day 13 of infection. The wall of the ring is usually thinner on the ventricular side of the abscess.3 At this point the central portion of the abscess is liquified and shows restricted diffusion. The rim enhancement reflects blood-brain barrier breakdown; inflammation can result in persistent contrast enhancement of the capsule even after the infection has resolved but resolution of the diffusion restriction indicates clearing of the purulent material.5
On MRI, pyogenic brain abscesses can look like many other conditions (see differential diagnosis). Parenchymal metastases are roughly spherical and also often surrounded by vasogenic edema. Since metastases lack the normal blood-brain barrier, they usually demonstrate avid peripheral enhancement, which is more likely as metastases grow and outstrip the available blood supply, leading to central necrosis. This central necrosis creates the T1 hypointense center, which together with the peripheral contrast enhancement, looks very similar to a brain abscess.5 An abscess rim is typically thicker and more irregular than that of a metastasis and the T2 hypointense rim is much more common with abscess, owing to phagocytic macrophages in the capsule wall creating free radicals.6
Tumefactive demyelination, defined as single or multiple large (usually > 2 cm) brain lesions, can mimic abscess or tumor. These lesions are rare in childhood and usually occur in adult women, often involving the white matter in a periventricular distribution. The classic enhancement pattern is an open ring with the continuous component on the ventricular side, unlike the abscess which is typically thinner on the ventricular side. A variety of other enhancement patterns may also be seen. The apparent diffusion coefficient values may be increased, which can also help distinguish a ring-enhancing tumefactive lesion from a brain abscess or necrotic tumor.7
Computed tomography or MRI imaging can make the diagnosis and help to guide therapy by determining the size and location of the brain abscess. In some cases, lesions of less than 2 cm may be managed with antibiotics alone, while larger lesions can be treated using several approaches including stereotactic-guided aspiration of purulent material or open surgical drainage.8
Although mortality from brain abscesses decreases with earlier diagnosis and treatment, it remains high (5-15%), with some estimates showing up to one-third of survivors developing long-term neurologic sequelae.9,10
Conclusion
Pediatric brain abscess has significant morbidity and mortality despite advances in diagnosis and therapy. Patients may present with fever, headache, and/or neurologic findings, including seizure. Imaging appearances depend on the stage of infection and distinguishing between abscess and other parenchymal lesions often requires clinical context.
References
- Capua T, Klivitsky A, Bilavsky, E, Ashkenazi-Hoffnung L, Roth J, Constantini S Grisaru-Soe G. Group A streptococcal brain abscess in the pediatric pPopulation. Pediatr Infect Dis J. 2018;37(10):967-970. doi:10.1097/INF.0000000000001947
- Rivera K, Truckner R, Furiato A, Martinez S. The diagnostic challenge of the pediatric brain abscess. Cureus. 2021;13(6):e15402. doi:10.7759/cureus.15402
- Feraco P, Donner D, Gagliardo C, et al. Cerebral abscesses imaging: A practical approach. J Popul Ther Clin Pharmacol. 2020 Jul 11;27(3):e11-e24. doi: 10.15586/ jptcp.v27i3.688. PMID: 32757543
- Chang P, Yang E, Swenson D, Lee E. Pediatric emergency magnetic resonance imaging: current indications, techniques, and clinical applications. Magnetic Resonance Imaging Clinics of North America. 2016;24(2):449-480. doi 10.1016/j.mric.2015.11.009
- Cartes-Zumelzu F, Stavrou I, Castillo M, Eisenhuber E, Knosp E, Thurnher M. Diffusion-weighted imaging in the assessment of brain abscesses herapy. AJNR Am J Neuroradiol. 2004;25(8):1310-1317
- Haimes AB, Zimmerman RD, Morgello S, et al. MR imaging of brain abscesses. AJR Am J Roentgenol. 1989;152(5):1073–1085.
- George T, Cicilet S, Hoisala R, Rout P. Multifocal tumefactive demyelination mimicking intracranial neoplasm. J Clin Diagn Res. 2016; 10(3): TD10- TD11. doi: 10.7860/JCDR/2016/15589.7465
- Abdulghani YS, Elzain MA, Ahmed ADS, Abdelhalim SA. Brain abscess burr hole aspiration in children with congenital heart disease in low facility centers: case series. Sudan J Paediatr. 2021;21(1):61-66. doi: 10.24911/SJP.106-1589487269. PMID: 33879945; PMCID: PMC8026005.
- Muccio CF, Caranci F, D’Arco F, et al. Magnetic resonance features of pyogenic brain abscesses and differential diagnosis using morphological and functional imaging studies: a pictorial essay. J Neuroradiol. 2014 Jul;41(3):153-67. doi: 10.1016/j.neurad.2014.05.004
- Yogev R, Bar-Meir M. Management of brain abscesses in children. J Pediatr Infect Dis. 2004;23(2)z;157-159. doi: 10.1097/01.inf.0000110272.67271.a2
References
Citation
A M D C, RB T, CM S, AJ T,. Brain Abscess. Appl Radiol. 2023;(1):56A-56C.
February 1, 2023