Bilateral Branchial Cleft Fistulae
Images


Case Summary
A young adult presented with complaint of intermittent discharge from small openings located over both lateral aspects of the lower neck since childhood. On examination, two small openings were noted, one on each side of the lateral aspect of lower third of the neck along the anterior border of sternocleidomastoid, along with mildly inflamed margins and mucopurulent discharge. No opening was found in the oropharyngeal cavity.
Imaging Findings
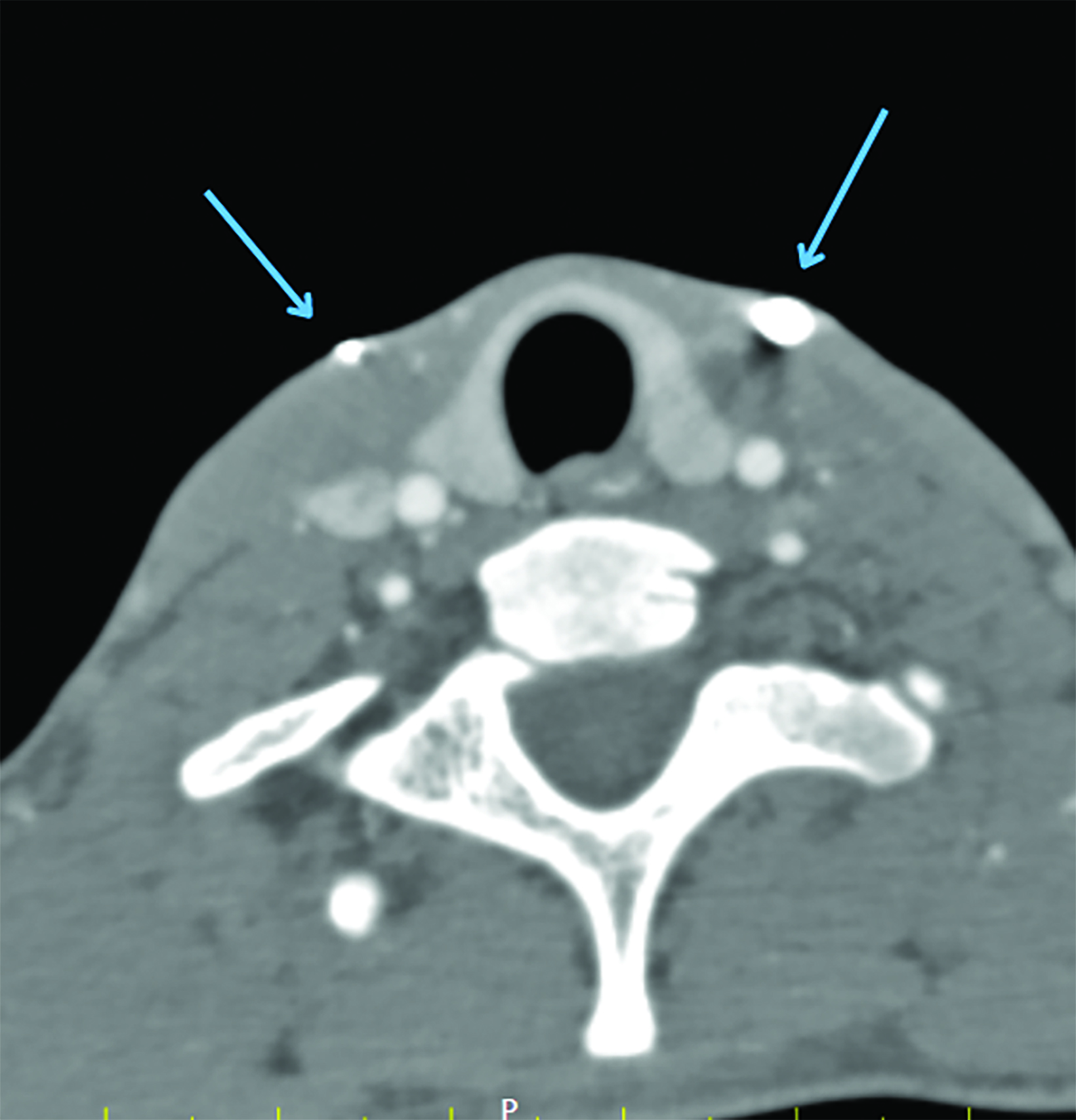
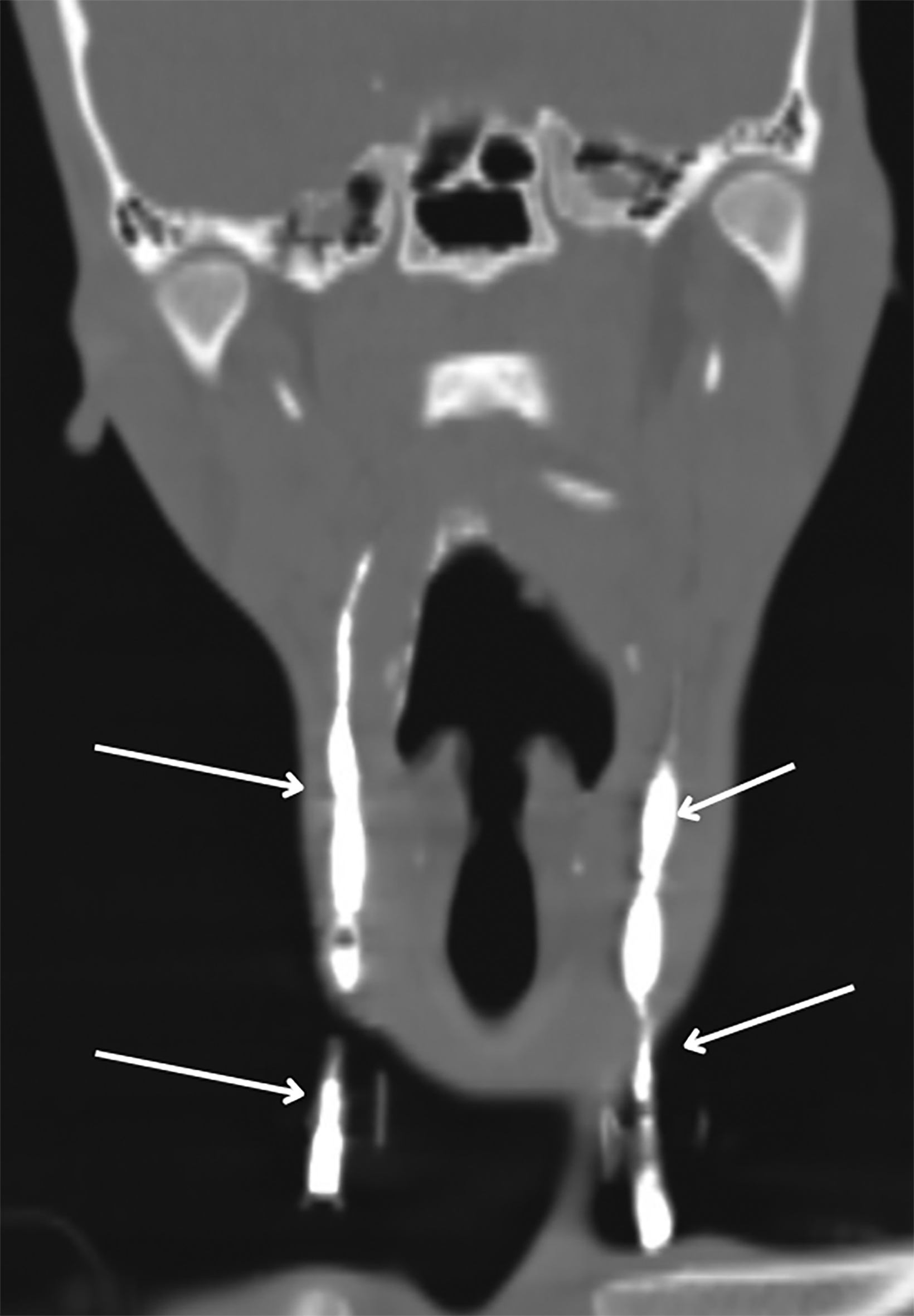
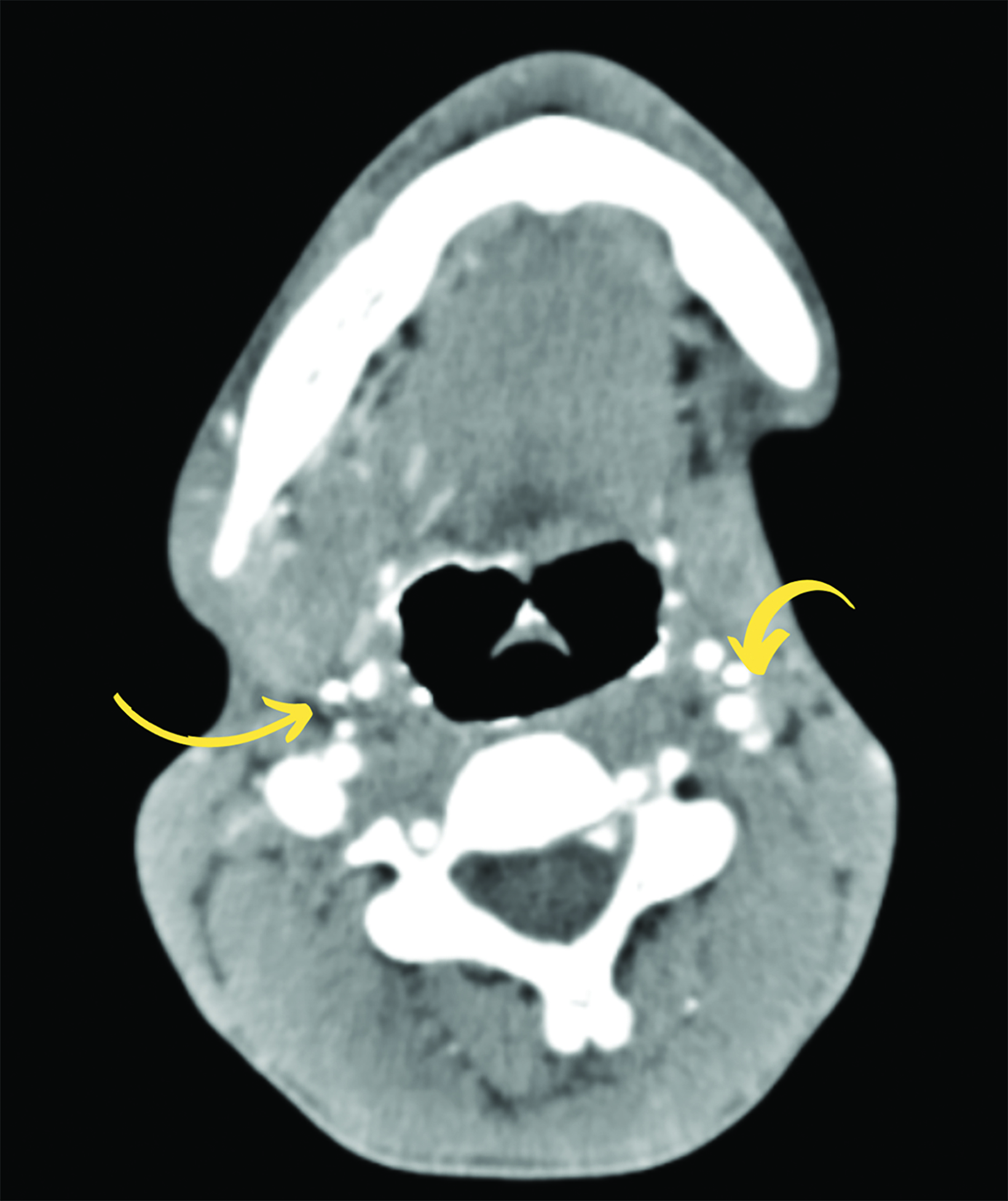
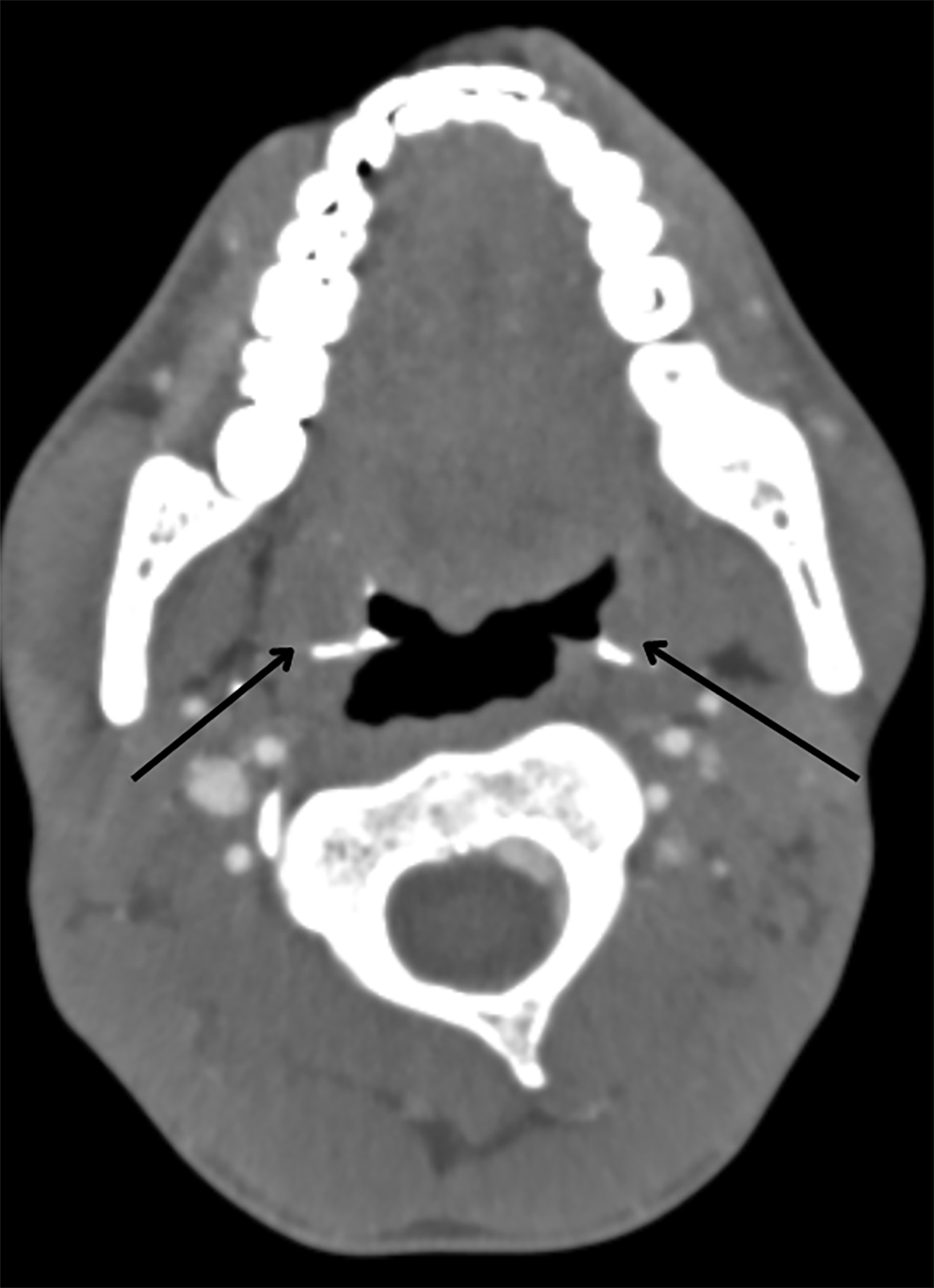
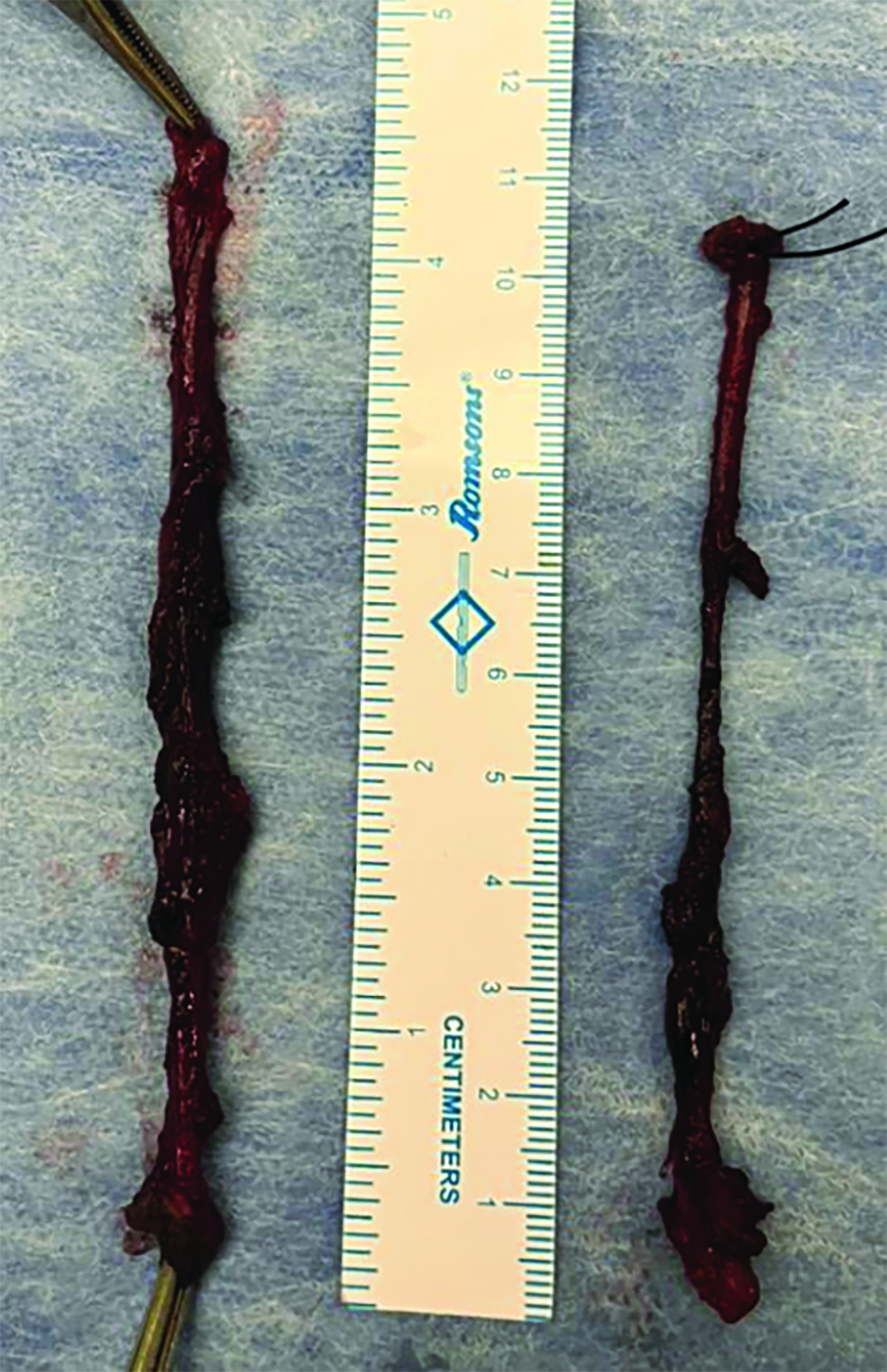
Intravenous contrast-enhanced CT with additional 10 ml of diluted contrast introduced through both openings revealed bilateral linear fistulous tracts in the neck with the external opening in the skin at the lower one-third of the sternocleidomastoid muscle, at the level of C7-T1 (Figure 1). The tracts coursed cranially along the anterior borders of the sternocleidomastoid muscles, anterior to the carotid spaces with medial bends at the C3 level and passed between the internal and external carotid arteries (Figure 2,3). The internal openings were within the tonsillar fossae of the oropharynx with contrast seen pooling in the oropharyngeal lumen (Figure 4). There was no abscess formation. The patient underwent surgery of complete excision of the tracts (Figure 5).
Diagnosis
Bilateral second branchial cleft fistulae. The differential diagnoses include thyroglossal duct fistulae and acquired fistulae secondary to infection.
Discussion
Mesodermal condensations present in the side wall of the embryological pharynx give rise to branchial arches and their pouches. Second branchial arch and pouch anomalies are common anomalies of the branchial apparatus.1 The anomalies of branchial apparatus were first described by Von Ascheron.2
During embryological development, the branchial arch grows caudally, enveloping the third, fourth, and sixth arches and forming the cervical sinus by fusing with skin caudal to these arches. Normally the edges of cervical sinus fuse and the ectoderm within it regresses. Abnormal persistence of this ectoderm gives rise to a cyst. The fistula results from the breakdown of endoderm internally; most commonly this occurs in the second pouch.1,3
While anomalies of the second branchial cleft account for 90% of all developmental abnormalities of the branchial apparatus, complete second arch fistulae are rare and comprise only 2%.4 Branchial cysts and simple sinus openings ending blindly after a variable distance are more common than branchial fistulae.5
Complete branchial fistulae with an internal opening are very rare. They are usually present at birth with the tiny external opening often going initially unnoticed and commonly presenting in childhood or the second decade.
Intermittent or continuous mucoid discharge and recurrent infection, particularly following an upper respiratory tract infection are common presenting symptoms. Abscess with cellulitis may also be a complication. Owing to variability in the course of the tracts and the need for complete excision, preoperative radiologic visualization of the tract is a prerequisite to successful treatment.
Radiographic fistulograms show a smoothly marginated tract with variable width along the usual anatomic course. Neck CT with administration of contrast through cutaneous openings has been shown to be superior for fistula demonstration, over noncontrast or intravenous contrast-only CT and conventional fistulogram.6,7 However, contrast injected into the fistula may not flow freely when the tract is blocked by secretions or granulation tissue.
The advantages of contrast-enhanced CT with a sinogram or fistulogram over conventional imaging include the ability to reconstruct images in multiple planes, including curved reformations, to offer better delineation of the tract in relation to other neck structures; and accurate depiction of the tract course to help guide the surgeon.
A fistulogram can help confirm the clinical diagnosis, to estimate the length and course of the tract, to look for an associated cyst.
The typical course of a second branchial cleft fistula begins at the external opening in the middle or lower third of the neck along the anterior border of the sternocleidomastoid muscle, runs deep to the platysma across the carotid sheath, taking a medial bend, and passes between the internal and external carotid arteries before finally opening into the tonsillar fossa.9
Surgery is the treatment of choice, as these entities will not regress spontaneously and there is increased incidence of recurrent infections due to the external communication. Imaging assists in surgical planning to facilitate complete excision of the tract to prevent recurrence. Sclerosing agents carry the risk of necrosis and perforation.
Recurrence, secondary infection, hematoma, and injury to traversing nerves or the internal jugular vein and are examples of potential surgical complications.10
Conclusion
Lateral cutaneous openings with discharge should raise suspicion for branchial fistulae and radiologic investigation. A CT fistulogram may be valuable to guide surgery.
References
- Ford GR, Balakrishnan A, Evans IN, et al. Branchial cleft and pouch anomalies. J Laryngol Otol. 1992;106:137-143.
- De PR, Mikhail T. A combined approach excision of branchial fistula. J Laryngol Otol. 1995;109:999-1000.
- Shinde K. Complete second branchial fistula: a study of four cases. Int J Head Neck Surg. 2013; 4 (3):129-132.
- Ismail Y, Ozcan C, Nuri O, Fatih B, Beyhan D. Complete fistula of the second branchial cleft: case report of catheter aided total excision. Int J Ped Otorinolaryngol. 2004;68:1109-1113.
- Kamal NR, Simi R, Dheeraj P, Joginder SG, Samar Pal Singh Y. Second branchial cleft fistula. Is fistulogram necessary for total excision. Int J Ped Otorinolaryngol. 2006;70:1027-1030.
- Burton MG. Second branchial cleft cyst and fistula. Am J Radiol. 1980 May;134:1067-1069.
- Ryu CW, Lee JH, Lee HK, Lee DH, Choi CG, Kim SJ. Clinical usefulness of multidetector CT fistulography of branchial cleft fistula. Clin Imaging. 2006; 30(5):339-342. doi: 10.1016/j.clinimag.2006.05.001. PMID: 16919556.
- Sun Z, Fu K, Zhang Z, Zhao Y, Ma X. Multidetector computerized tomographic fistulography in the evaluation of congenital branchial cleft fistulae and sinuses. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(5):688-694. doi: 10.1016/j.oooo.2011.08.015. Epub 2012 Apr 12. PMID: 22668628.
- Talaat M. Pull-through branchial fistulectomy: Technique for the otolaryngologist. Ann Otol Rhino Laryngol. 1992;101:501-502.
- Francisco C, Agaton B, Cosmay GE. Diagnosis and treatment of branchial cleft cysts and fistulae. A retrospective study of 183 patients. Int J Oral Maxillofac Surg. 1996;25: 449-452.
Citation
PJ PP, J VV, J SH. Bilateral Branchial Cleft Fistulae. Appl Radiol. 2024;(1):48g-48i.
January 24, 2024