Beyond the Order: Results Review With Patients
A series of failed communications surrounding disclosures of imaging results over many years led to an incremental increase in radiologists communicating about significant findings with referring physicians and, ultimately, patients.1 The rise in state and federal regulations, including the 21st Century Cures Act, has further fueled radiologist participation in direct conversations about findings. These regulations mandate that health care professionals make health information, including images and radiology reports, available to patients through portals and other web-based tools.
This involvement has brought medicolegal and economic considerations to the forefront, including nuances about patients’ understanding of findings as well as workload challenges for already overworked radiologists. While the duty of communicating results once fell to referring physicians, radiologists are now joining the conversation.
“We need to remember that our patients are reading their reports; we’re no longer just communicating with the clinician who ordered the study,” says Tessa S. Cook, MD, PhD, associate professor of radiology and vice chair of Practice Transformation in the Department of Radiology at Perelman School of Medicine at the University of Pennsylvania in Philadelphia.
With existing strain and growing demand for medical imaging, providers weigh the benefits and challenges of consulting directly with patients in various forms.
What the Research Says
With relationship-building commonplace in patient-facing imaging specialties such as breast imaging and interventional radiology, the American College of Radiology and Radiological Society of North America have led initiatives to promote patient-centered care throughout all of radiology. Integrating radiologists for the duration of a patient’s care journey — from requesting scans through interpretation and communication of results —indeed may bring value to the patient and elevate radiology, says Colbey W. Freeman, MD, assistant professor of radiology at Penn Medicine in Philadelphia, but notes that patient preferences and resultant outcomes must be better understood.
Consulting with patients can take many forms, from quick phone calls to more formal video conference reviews or in-clinic meetings, not a “one-size-fits-all” approach, says Dr Freeman.
“We, as radiologists, may want to talk to patients. The question we need to be asking is do patients really want to talk to us?” The literature on the topic is “all over the place,” he says.
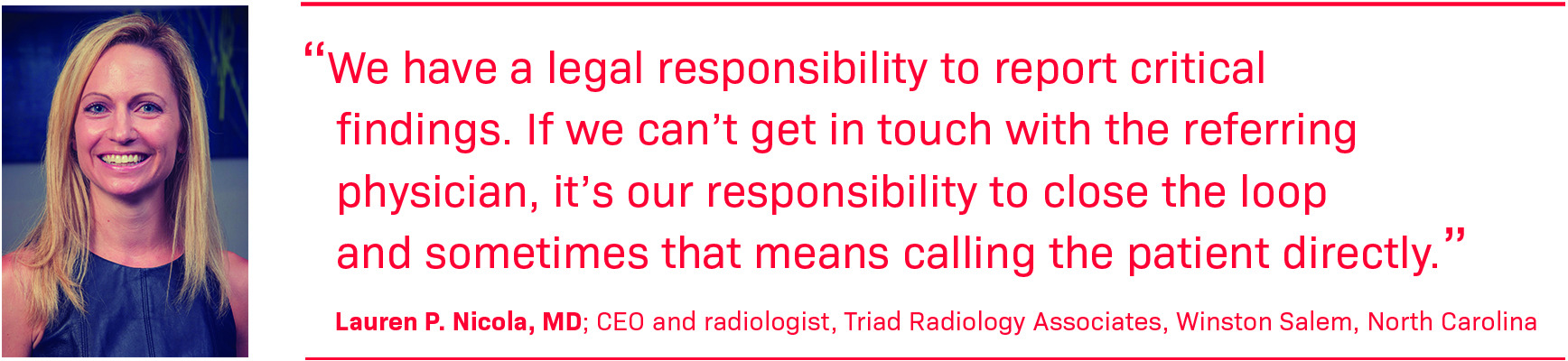
Lauren P. Nicola, MD, CEO, and radiologist at Triad Radiology Associates in Winston Salem, North Carolina, agrees that evidence on patients’ desire for radiologist interaction is “a little contradictory and situational.” “In diagnostic radiology, it depends on how you frame the question, and the literature reflects that.”
In one study by Cabarrus et al, 63% of patients preferred models of results delivery centered on the referring physician as opposed to the radiologist.2 However, respondents were asked about getting results “from someone with whom you already have a relationship [that is the referring physician] vs an expert in imaging with whom you don’t have a relationship,” says Dr Nicola, who calls the phrasing “leading.”
“In other studies when it’s asked if it would be beneficial for radiologists to go over the images, the majority [of patients] say they would find benefit,” she says.
In a study by Mangano et al, patients with common conditions such as atherosclerosis or emphysema were offered the opportunity to formally meet with a radiologist to review their most recent imaging findings, initiated and scheduled by the primary care clinic. Participants rated the consultation as “very helpful,” and all said they would take the opportunity to review studies with the radiologist again.3 Dr Freeman explained that patients offered a consultation in a physical clinic may be a “captive audience” and more inclined to participate in a consultation experience as opposed to one via phone or video conference.
Another study by Cross et al showed that when a phone number for follow-up questions was embedded in 3896 radiology reports, patients contacted their radiologist for only 0.56% of the exams.4
“When we embarked on the study to add phone numbers to our reports, there was some concern that our phones would start ringing nonstop. But that didn’t happen; the volume of calls was very manageable,” says Dr Cook, noting that in a handful of cases the conversations led patients to get emergent care.
“Life is busy. It’s hard for patients to take out additional time to talk to us,” adds Dr Freeman, who examined patient-radiologist communication regarding results and radiology recommendations. After texting 38 patients following lung cancer screening CT exams, he performed three online consultations.5
“We learned that they were fine with their primary care doctor or pulmonologist talking to them about results,” Dr Freeman says. “Most people are comfortable with the people they see in their more frequent, personal interactions.”
Medicolegal Considerations
The Cures Act has enabled patients to electronically access their health information, most often through portals. However, reviewing imaging results instantaneously, and sometimes before the referring physician, has implications.
“Receiving results without context is never good,” says Dr Freeman, noting that jargon-filled reports were never intended for patients. “Things that are completely benign may sound very frightening out of context.”
“Patients are empowered in this age of the internet and immediate access to information,” adds Dr Nicola. “It helps with health literacy but sometimes those Google searches can cause a lot of unnecessary anxiety.”
When a radiologist detects a suspicious mass, Dr Nicola suggests giving the referrer a “heads-up call” so everyone’s on the same page. This could prevent a patient from seeing the result in the portal and calling their primary care physician about it before the ordering physician is even aware of the report, she says.
Regarding communication of results, Dr Nicola says, “We have a legal responsibility to report critical findings. If we can’t get in touch with the referring physician, it’s our responsibility to close the loop and sometimes that means calling the patient directly.”
Some legal ambiguity remains about who is liable if the radiologist tells the referring physician but the patient is never notified, says Dr Nicola, calling it a “big legal unknown.”
When reviewing findings with patients, Dr Nicola advises radiologists not to make recommendations regarding treatment, and “stay in their lane of expertise.” It’s best to maintain professional courtesy with team members and not second-guess or criticize clinical decisions, she says.
Similarly, Dr. Freeman’s virtual consult service took a “show-and-tell” approach: Demonstrate the results visually and explain the screening recommendations.
“[This way], there wasn’t a fear that we would go outside what the ordering providers intended,” he says. “You don’t want to have two providers giving conflicting information … there are medicolegal challenges there.”
Economic Implications
Radiologists who make themselves available for patient consults face the reality that the service is not billable. Discussing the findings with the referring physician and/or patient is already built into the payment.
“The problem is, we’re not really adding anything beyond what we’re already paid for technically with these consults,” explains Dr Freeman.
While some providers establish radiology consult clinics, they generally cannot bill for the service, as communicating findings to patients is already part of the reimbursement for the original interpretation of the exam. In rare cases when the original interpretation was not performed by a radiologist in the same taxpayer ID (TIN), it may be possible to generate a billing event for the consultation, but these would require a lot of effort on the part of the billing team for limited financial reward.
“There’s not a lot of direct financial upside,” Dr Nicola concurs.
Radiologist availability is also a major challenge. In fact, time or workload is the most cited inhibitor to communicating with patients.6
“Our volumes go up every year,” says Dr Freeman. “How do you carve out time in your day … to look at old studies and not do new work?”
Both radiologists agree, however, that patient consults have potential to benefit providers and patients. As more payers and institutions weigh value-based care metrics, patient satisfaction can generate financial benefits. And by building relationships and loyalty, the patient is more likely to get follow-up scans when applicable, which can prevent additional conditions and disease from worsening, and improve overall health.
Without incentives, only a relatively small number of institutions provide radiology-patient consultation clinics,6 and a major overhaul of payment policy for consultation seems unlikely. Dr Freeman has sought grants to study increasing direct interaction between radiologists and patients but has been told repeatedly that expanding consultation is “not generalizable.”
For practices committed to engaging in consultation, Dr Freeman suggests radiologists be patients’ partners in care.
“Be the person who cares to sit down and talk with them,” he says. “You’re fighting a common enemy. Ask them what they want to know and do your best to improve their understanding of where they are so they can make the most informed decisions.”
“Speaking with patients and helping them understand their health reminds me of why I went into medicine,” adds Dr Cook. “It’s easy to lose sight of that as our worklists grow and our studies become more complex. I hope our systems find a way to make radiologist-patient consultation a realistic service we offer in the future.”
References
Citation
Reeves, K. Beyond the Order: Results Review With Patients. Appl Radiol. 2024; (5):26 - 28.
doi:10.37549/AR-D-24-0028
October 1, 2024