Assessing MRI Facility Damage Post-Hurricane: Best Practices and Safety Considerations
Introduction
While direct testimonials from MRI technologists regarding post-hurricane damage to MRI scanners may not be widely published, several reports and studies from health care facilities have documented the significant impact of hurricanes on medical imaging equipment, particularly MRI systems ( Table 1 ). Hurricanes Milton and Helene recently inflicted substantial damage along the Gulf Coast, creating challenges for health care facilities equipped with MRI scanners. These events underscore the importance of immediate damage assessments and the implementation of safety protocols to protect MRI equipment, personnel, and patients.1
Issues MRI Centers Commonly Face After Hurricane Damage
| Challenge | Description |
|---|---|
| Water damage | Flooding and water intrusion are major risks, especially in coastal areas. Water can cause humidity issues, leading to condensation that damages the MRI scanner’s electrical and mechanical components. |
| Power outages and quenching | MRI scanners are highly sensitive to power disruptions. Extended power outages can cause quenching, where the magnet loses superconductivity due to helium evaporation, resulting in downtime and costly repairs. |
| Quench pipe blockages | Wind-driven rain during hurricanes can block or obstruct quench pipes, which are essential for safely venting helium gas. Blockages can create risks when restarting the system after the storm. |
| Structural damage and delays | Structural damage to the facility can lead to delays in restarting MRI scanners as inspections and repairs must be completed to ensure safe operation. |
MRI presents unique safety challenges, largely due to the presence and interaction of 3 distinct magnetic fields integral to the imaging process.2 These fields are:
-
Static magnetic field (B0 ). This primary and constant field, generated by the MRI scanner, creates a powerful magnetic environment that affects all ferromagnetic objects and materials within its vicinity. The high-strength static field poses risks such as projectile accidents and interference with electronic implants or devices.
-
Radiofrequency magnetic field (B1 ). This field is essential for generating MRI signals and is time-varying during scans. However, it can lead to patient heating and potential tissue burns if not appropriately managed. The B1 field interacts with human tissues and implanted devices, necessitating rigorous safety protocols to prevent adverse effects.
-
Gradient magnetic fields (dB/dt ). These rapidly varying fields, responsible for spatial encoding in MRI, create risks of peripheral nerve stimulation. While they contribute to the production of clear and detailed images, they can induce electrical currents in the body, leading to discomfort or even unintended muscular contractions.
The complex interplay of these 3 magnetic fields ( Figure 1 ) is at the heart of MRI technology. However, their presence also introduces distinct safety challenges, necessitating stringent protocols to safeguard both patients and health care personnel. Recognizing and mitigating the risks associated with these fields is crucial to maintaining safe MRI practices and ensuring the integrity of diagnostic outcomes.
Schematic diagram of a superconducting magnet MRI system. Closest to the bore wall, adjacent to the patient, is the radiofrequency (RF) coil, which plays a critical role in transmitting and receiving signals. Proximity to this coil can pose a risk of patient heating or burns if safety protocols are not observed. Surrounding the RF coil are the gradient coils, which generate rapidly changing currents responsible for the characteristic acoustic noise during imaging and may also induce peripheral nerve stimulation. The outermost ring represents the static magnetic field (B0), which generates strong translational and rotational forces on ferromagnetic objects. Each of these electromagnetic fields can interact with metallic objects or implanted medical devices, emphasizing the importance of stringent safety measures within the MR environment. From: ACR Committee on MR Safety. ACR Manual on MR Safety (manual). Reston, VA: American College of Radiology, 2024, p. 10; used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.2

In addition to these inherent risks, MR systems rely heavily on maintaining superconductivity within the magnet coils. A critical failure, known as a helium quench, occurs when liquid helium, essential for cooling the superconducting magnets, rapidly transitions to a gaseous state due to an equipment malfunction, power disruption, or operational error. This sudden vaporization can compromise the magnetic field, damage sensitive components, and pose serious safety hazards. To mitigate such risks, facilities must implement robust safety measures, including pressure relief systems and emergency ventilation protocols ( Figure 2 ). Proper training with regular maintenance is essential to managing quench events effectively while sustaining MRI safety and performance.3
A quench event in a research MRI magnet (left) shows the release of gaseous helium. Such events necessitate stringent safety protocols, including appropriate ventilation systems and emergency procedures to protect personnel from cryogenic hazards and asphyxiation risks. In an installation of a quench tube in an MRI (right), the blue arrow points to the tube and the green arrow points to the vent in the ceiling. Quench tubes serve a crucial role in venting helium gas from the MRI scanner during a quench event. Proper attachment and secure connections between the quench tube and vent are vital to maintaining safety within the MRI suite, especially during quench scenarios. Printed with permission from MRIquestions.com.

In the context of disaster preparedness, health care facilities must place a high priority on establishing comprehensive safety and recovery strategies. These strategies should encompass thorough risk assessments, environmental controls, and routine technical inspections. The following guidelines, grounded in research and expert recommendations, provide a framework for addressing hurricane-related threats to MRI systems. Implementing these best practices is vital for minimizing risks, ensuring a safe recovery, and preventing long-term damage to critical equipment.
Primary Threats to MRI Facilities: Wind and Water
Hurricanes pose 2 primary threats to MRI facilities: wind and water. Wind-driven debris can cause structural damage, leading to water intrusion. Heavy rainfall, which often exceeds 20 to 40 inches during hurricanes, poses additional risks by overwhelming drainage systems, particularly in low-lying areas. This increases the likelihood of water entering the facility, which can affect MRI equipment by increasing humidity levels and causing condensation on sensitive components.4
The American College of Radiology (ACR) recommends ( Table 2 ) maintaining relative humidity levels of 30% to 50% within MRI suites using dehumidifiers. Such environmental controls help protect MRI systems from damage caused by condensation. Proper inspections should be conducted following severe storms to identify any water intrusion that may threaten equipment functionality.2
American College of Radiology Guidelines
| Key Points | American College of Radiology Guidelines Regarding MRI Safety Best Practices for MRI Facility Safety |
|---|---|
| Environmental controls | Implement dehumidifiers to maintain 30-50% relative humidity levels in MRI suites to protect against condensation. |
| Electrical power management | Equip MRI systems with uninterruptible power supplies and backup generators to mitigate risks of quenching. |
| Quench pipe inspections | Inspect quench pipes for blockages, especially after hurricanes, to prevent obstructions that could cause equipment damage. |
Impact on MRI Quench Pipes
Quench pipes, essential safety components for the controlled release of helium gas during a magnet quench, are particularly vulnerable to wind-driven rain. If water or debris obstructs these pipes, it can prevent proper venting during a quench, leading to significant equipment and structural damage.5 It is critical to inspect quench pipes after a hurricane to ensure their proper function.
Power Outages and MRI Safety
Power outages pose a substantial risk to MRI systems. Unlike most imaging equipment, MRI scanners maintain their magnetic field even during power loss. The cooling system relies on a continuous power supply to prevent helium from warming and evaporating. A key component of this cooling system is the chiller unit, which maintains the superconductive magnet coils in a stable, cold state using liquid helium. When a chiller unit fails, the most immediate consequence is a loss of cooling capacity ( Table 3 ). This interruption causes the air-conditioned space to gradually warm and, depending on the MRI scanner model, error codes may display on the control panel indicating a need for professional service.6
MRI Chiller Features, Troubleshooting, and Key Practices
| Aspect | Key Points | Description |
|---|---|---|
| Chiller failures | No cooling | Loss of effective cooling results in uncomfortable temperatures within the facility. |
| Error codes | Modern chillers have built-in diagnostics that display error codes on the control panel to help identify issues. | |
| Automatic shut-off | Many chillers include safety features that automatically shut down the unit in case of critical malfunctions. | |
| Maintenance required | Professional service is typically needed to diagnose and repair chiller issues. | |
| Possible causes | Low refrigerant levels | A common cause of reduced cooling capacity. |
| Faulty compressors | Malfunctioning compressors often lead to chiller failures. | |
| Clogged condensers | Dirty condenser coils can hinder heat transfer and decrease cooling efficiency. | |
| Water flow problems | Insufficient water flow within the chiller can result in poor cooling performance. | |
| Electrical issues | Power supply problems or faulty electrical components are common triggers of chiller malfunctions. | |
| Additional troubleshooting practices recommended by the American College of Radiology | Routine inspections and maintenance | Regularly inspect chiller components, including condensers, compressors, and electrical connections to prevent failures. |
| Environmental controls | Maintain optimal humidity levels (30-50%) within the MRI suites using dehumidifiers to protect both the chiller and MRI system components. | |
| Backup power testing | Perform routine tests on uninterruptible power supplies and backup generators to prevent cooling system failures during power outages. |
To mitigate these risks, health care facilities should equip MRI systems with uninterruptible power supplies (UPSs) and dedicated backup generators. Routine testing of backup systems is crucial, particularly before hurricane season, to ensure their functionality.7
Safety Precautions for MRI Facilities After a Hurricane
Following a hurricane, immediate action is essential to assess damage and minimize risks. The steps in Table 4 outline critical safety precautions.
Critical Steps and Safety Precautions for MRI Facilities Following a Hurricane
| Action | Description |
|---|---|
| Inspect for wind and rain damage | If severe wind and rain have occurred, assume potential quench pipe blockage and arrange inspection by qualified service personnel. Risk of quench pipe blockage is reduced if weather was mild.1 |
| Assess quench status | If the MRI has quenched, contact service personnel to reseal the magnet and assess each magnet individually. If no quench occurred, keep untrained personnel away from the discharge point. If power remains off, the risk of quenching increases.1 |
| Evaluate building’s power status | If power is available, exercise caution regarding electrical hazards, especially in cases of water infiltration. If power is off, quickly restore it and be aware that it may still pose magnetic field hazards.5 |
| Personnel safety | Prevent untrained personnel from approaching the quench pipe discharge area. Inform staff of risks related to magnetic fields and quench events during cleanup or repairs.5 |
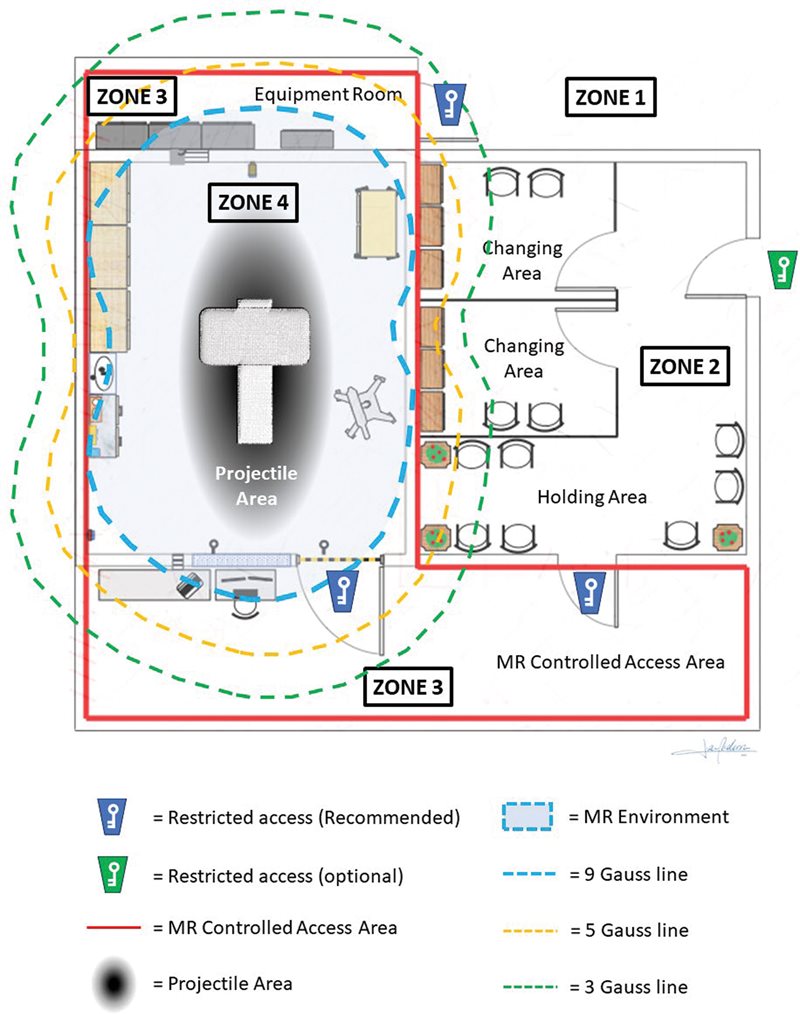
Frank G. Shellock, PhD, has made significant contributions to the field of MRI safety, particularly under extreme conditions such as hurricanes. His work offers valuable insights into magnetic field safety, management of helium quenching, and training for MRI personnel during disaster recovery. Dr Shellock emphasizes the critical importance of adhering to stringent safety protocols in MRI facilities after a hurricane, including inspections for magnetic containment, appropriate system shutdowns, and comprehensive staff training.8 His guidelines on magnetic field safety and emergency protocols, especially in post-hurricane MRI recovery, contain valuable details and recommendations.8 - 12 The MR projectile area, MR environment, and MR-controlled access area and their relationship to the 4 ACR MR safety zones are illustrated in Figure 3 .
Example of a zone layout in MRI facilities. This layout is adapted from Figure 1 in the Medicine and Healthcare products Regulatory Agency Safety Guidelines for Magnetic Resonance Imaging Equipment in Clinical Use. Note depictions of the MR-controlled access area, MR environment, and projectile area as they relate to the 4-zone model. Source: Medicines and Healthcare Products Regulatory Agency. Safety guidelines for magnetic resonance imaging equipment in clinical use. Published November 7, 2014. Accessed November 7, 2024. Magnetic resonance imaging equipment in clinical use: safety guidelines - GOV.UK. www.gov.uk/government/publications/safety-guidelines-for-magnetic-resonance-imaging-equipment-in-clinical-use.
Key considerations for post-hurricane safety and recovery protocols vary across the MRI vendors for their systems. MRI center personnel should be familiar with the common practices and vendor-specific protocols following major disasters.13 - 15 Table 5 shows additional recovery tips and Table 6 summarizes considerations for safety and recovery protocols after a hurricane.
Additional Recovery Tips and Best Practices Following a Hurricane
| Best Practice | Description |
|---|---|
| Infrastructure modifications | Install preventive measures like flood barriers and sump pumps, and elevate electrical systems. Maintain roofing, windows, drainage systems, and quench pipe weatherheads to minimize water intrusion risks.16 |
| Quench simulation drills | Regularly conduct quench simulation drills to train staff in emergency procedures, including safe evacuation and management of quench pipe blockages. Establish detailed emergency shutdown protocols. |
| Communication with emergency services | Develop an emergency response plan that includes communication protocols with local emergency services and first responders to ensure coordinated recovery efforts.17 |
| Risk assessment and insurance | Conduct risk assessments with insurance providers to identify potential financial losses and ensure comprehensive insurance coverage for equipment damage and business interruption costs.18 |
Key Considerations for Post-Hurricane Safety and Recovery Protocols
| Key Points | Recommendations for Post-Hurricane Response |
|---|---|
| Keep MRI service personnel on standby | Ensure MRI service personnel are available after a storm to provide guidance on safe operations and assist with recovery procedures. |
| Maintain MRI refrigeration system | If water is suspected in the quench pipe, maintain the MRI’s refrigeration system to prevent catastrophic quenching. |
| Avoid metal tools during cleanup | During cleanup, avoid using tools with internal metal components as these can become dangerous projectiles near strong magnetic fields.6 |
Conclusions
Hurricanes pose significant risks to MRI facilities, including wind, water damage, and power outages. By understanding these threats and implementing best practices — such as environmental control, electrical power management, and proper personnel training — health care facilities can effectively reduce the risk of equipment damage and ensure a safer recovery process. Incorporating preventive infrastructure modifications, communication strategies, and comprehensive risk assessments into emergency preparedness plans will further enhance the resilience of MRI facilities against hurricane impacts.
References
Citation
Rey-Vasquez LPD, RVT(ARDMS), RT(R)(MR)(ARRT), MRSO(MRSC). Assessing MRI Facility Damage Post-Hurricane: Best Practices and Safety Considerations. Appl Radiol. 2024; (6):12 - 17.
doi:10.37549/AR-D-24-0038
December 1, 2024